- Department of Neurosurgery, University of Toyama, Toyama, Japan.
Correspondence Address:
Satoshi Kuroda, Department of Neurosurgery, University of Toyama, Toyama, Japan.
DOI:10.25259/SNI_386_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shu Ueda, Shusuke Yamamoto, Yuichiro Koga, Satoshi Kuroda. Cauda equina syndrome due to posttraumatic syringomyelia in conus medullaris – A case report. 12-Jul-2024;15:243
How to cite this URL: Shu Ueda, Shusuke Yamamoto, Yuichiro Koga, Satoshi Kuroda. Cauda equina syndrome due to posttraumatic syringomyelia in conus medullaris – A case report. 12-Jul-2024;15:243. Available from: https://surgicalneurologyint.com/surgicalint-articles/12986/
Abstract
Background: Most posttraumatic syringomyelias occur in the cervical or thoracic spinal cord, where they contribute to myelopathic deficits. Here, a 40-year-old patient presented with the left leg monoparesis due to syringomyelia involving the conus medullaris 10 years after an L2 vertebral “crush” fracture.
Case Description: Ten years following an L2 vertebral “crush” fracture, a 40-year-old male presented with the new onset of left lower leg paresis. The magnetic resonance imaging showed a T12–L1 syrinx associated with accompanying high-intensity areas above the syrinx located between the T11 and T12 levels. One month after placing a syringosubarachnoid (SS) shunt, both the syrinx and high-intensity area rapidly disappeared, and the left distal motor weakness resolved.
Conclusion: Ten years following an L2 “crush” fracture, a 40-year-old male presented with the new onset of a cauda equina syndrome secondary to a posttraumatic T12–L1 syringomyelia causing expansion of the conus medullaris.
Keywords: Cauda equina syndrome, Conus medullaris, Posttraumatic syringomyelia, Syringosubarachnoid shunt
INTRODUCTION
Posttraumatic syringomyelia is one of the complications after spinal cord injury and may contribute to the onset of myelopathy. The etiology of such syringomyelias is largely attributed to adhesive arachnoiditis (i.e., disturbed cerebrospinal fluid [CSF] flows around the injured spinal cord). Surgery, whether consisting of shunting, marsupialization, and/or operative resection/decompression, is not always effective.[
CASE PRESENTATION
Ten years ago, the patient sustained an L2 “crush” (i.e., burst fracture). Now, at age 40, he presented in a wheelchair, due to the progressive 3-week onset of the left distal leg weakness (i.e., anterior tibialis muscle [manual muscle testing (MMT), 0/5], soleus muscle [
Radiology
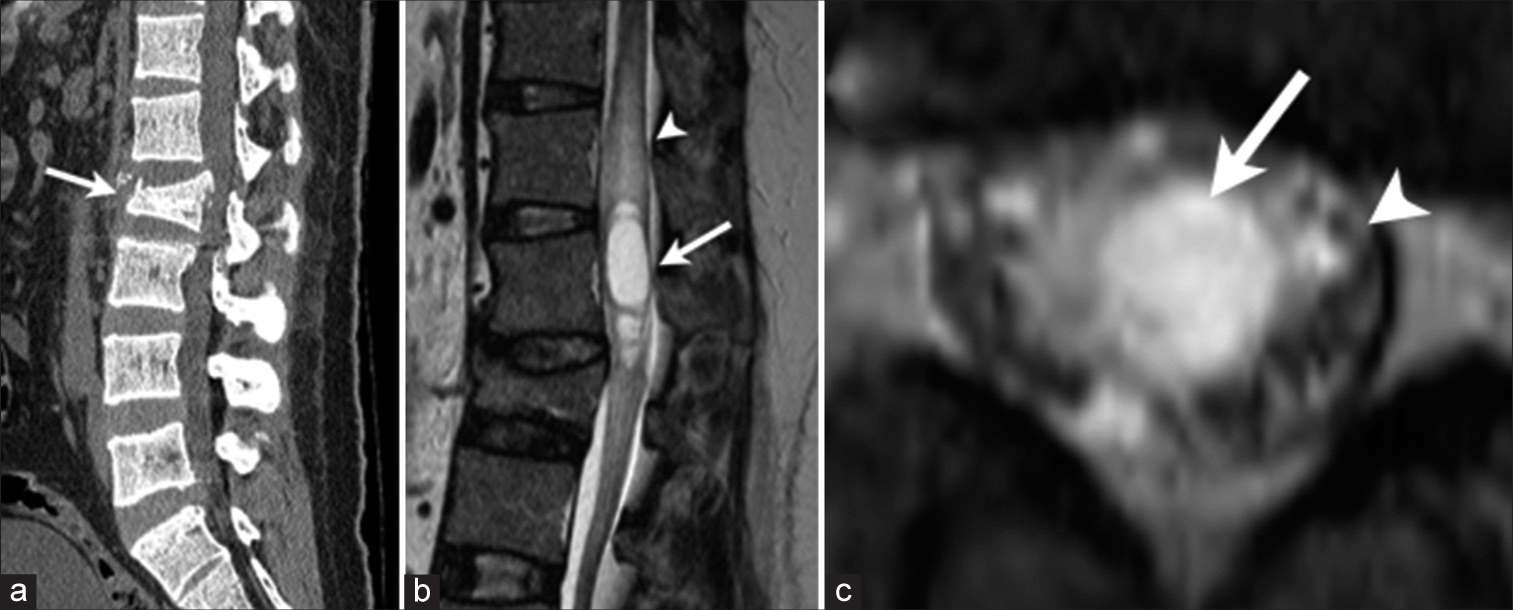
The non-contrast computed tomography showed L2 vertebral deformity with mild compression of the dural sac. In addition, the T2-weighted magnetic resonance imaging (MRI) showed a T12–L1 syrinx, while the cine-MRI showed almost no motion of the CSF around the conus medullaris. The cauda equina was markedly compressed by the expanded conus medullaris syrinx [
Figure 1:
Preoperative radiological findings. (a) A sagittal view of a plain computed tomography scan demonstrates a burst fracture of the L2 vertebra (arrow). Note that the L2 vertebra is narrowing the spinal canal. (b) The sagittal view of T2-weighted magnetic resonance imaging (MRI) shows the formation of a large syrinx in the conus medullaris centered at the L1 level (arrow). Note the high-signal intensity rostral to the syrinx at T11–T12 level (arrowhead). (c) Axial view of T2-weighted MRI at L1 level shows a markedly expanded conus medullaris due to syrinx (arrow). Note the compressed cauda equina around the conus medullaris (arrowhead).
Surgery
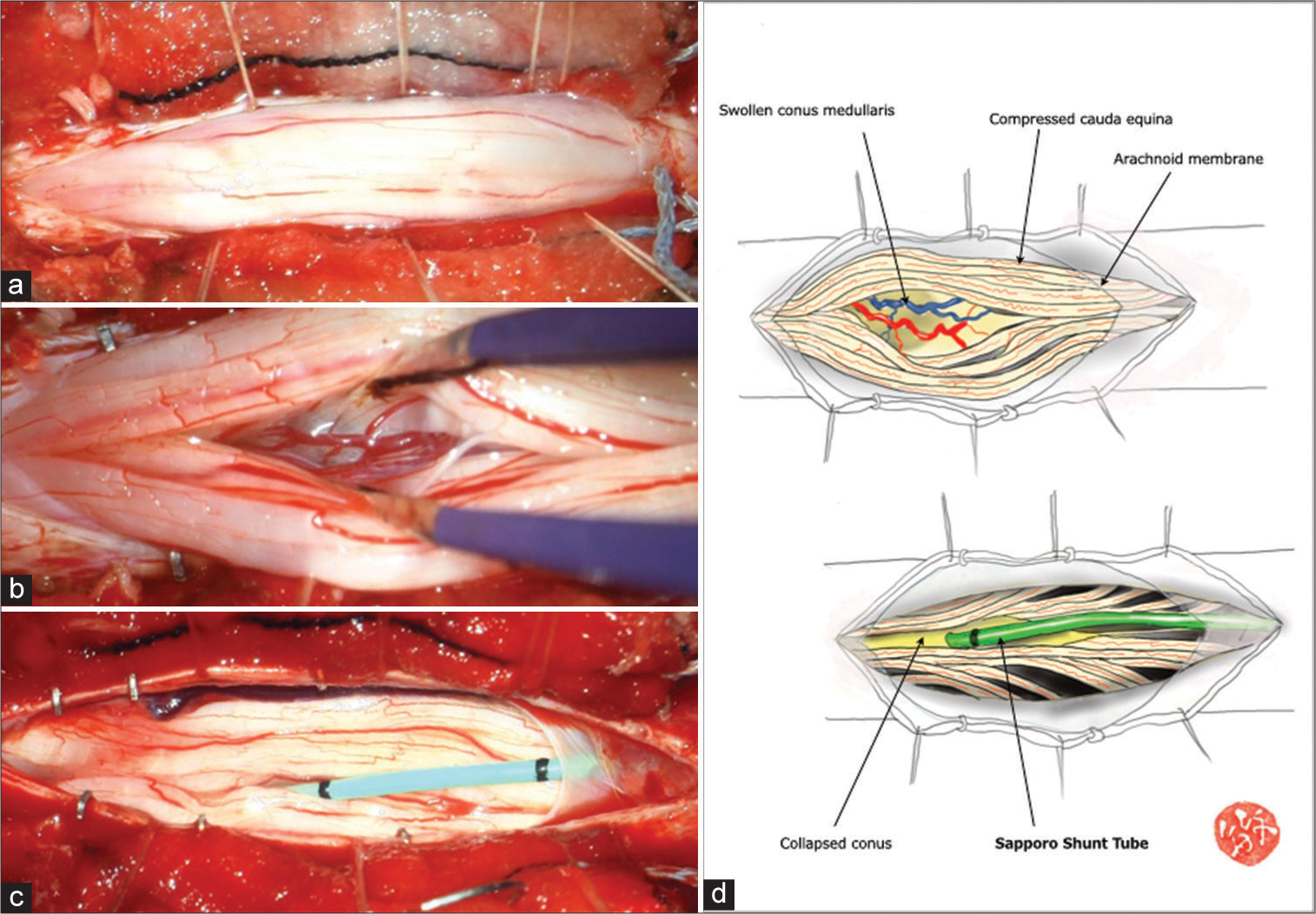
On completing the T12–L2 laminectomy, we found that the dural sac was markedly distended; after opening the dura, the conus/cauda equina protruded from the dural sac under increased pressure [
Figure 2:
Intraoperative findings. (a) Following the dural opening, the conus medullaris and cauda equina protruded from the dural sac. Note no adhesive arachnoiditis. (b) The conus medullaris was markedly expanded, and the syrinx was permeable. (c) After the insertion of the syringosubarachnoid shunt tube into the syrinx, the conus medullaris rapidly shrank, and the cauda equina was settled into the dural sac. (d) Illustration of operative findings by SK demonstrates the post-SS shunting change in the size of the conus medullaris.
Postoperative course
Postoperatively, the left anterior tibialis muscle strength improved from 0/5 to 2/5, and within 12 days, all motor deficits were fully resolved. Three days postoperatively, the MRI showed a 50% decrease in the syrinx size, along with full resolution of the high intensity adjacent signal in the conus. Two months later, the MR showed that the conus syrinx had completely resolved [
Figure 3:
Postoperative radiological findings. (a) Sagittal view of T2-weighted magnetic resonance imaging (MRI) shows almost complete disappearance of syrinx in the conus medullaris (arrow). Note the simultaneous disappearance of the high-signal intensity area rostral to the syrinx at the T11– T12 level (arrowhead). (b) Axial view of T2-weighted MRI at L1 level shows a marked shrinkage of conus medullaris after surgery (arrow). Note the resolution of the compression against the cauda equina (arrowhead).
DISCUSSION
Frequency and time to onset of posttraumatic syringomyelia
Posttraumatic syringomyelia accounts for <4% of all syringomyelias. Their locations depend on the level of the original spinal cord injury. Most occur between the C1 and T11 levels.[
Etiology of posttraumatic syringomyelia
Posttraumatic syringomyelias involving the conus medullaris are typically characterized by the onset of motor weakness in both lower limbs and are accompanied by a neurogenic bladder.[
Treatment of posttraumatic syringomyelia
Surgery for posttraumatic syringomyelia most typically includes SS shunts or syringoperitoneal shunts; some may be accompanied by additional open operative procedures (i.e., marsupialization and/or direct cyst decompression/excision). Reports for the two types of shunts show no significant differences in outcomes (i.e., 61% and 64%, respectively).[
CONCLUSION
A posttraumatic syringomyelia at the T12/L1 level/conus caused a cauda equina syndrome 10 years after an L2 burst fracture; following SS shunt placement, all symptoms were fully resolved.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Bonfield CM, Levi AD, Arnold PM, Okonkwo DO. Surgical management of post-traumatic syringomyelia. Spine (Phila Pa 1976). 2010. 35: S245-58
2. Bratelj D, Stalder S, Capone C, Jaszczuk P, Dragalina C, Potzel T. Spinal cord tethering and syringomyelia after trauma: Impact of age and surgical outcome. Sci Rep. 2023. 13: 11442
3. Brodbelt AR, Stoodley MA. Post-traumatic syringomyelia: A review. J Clin Neurosci. 2003. 10: 401-8
4. Guler-Uysal F, Orkun S, Cila A, Ozgirgin N. Delayed post-traumatic syringohydromyelia after an uncomplicated fracture of the spine: Case report and literature review. Spinal Cord. 1996. 34: 301-4
5. Leclerc A, Matveeff L, Emery E. Syringomyelia and hydromyelia: Current understanding and neurosurgical management. Rev Neurol (Paris). 2021. 177: 498-507
6. Lee TT, Alameda GJ, Camilo E, Green BA. Surgical treatment of post-traumatic myelopathy associated with syringomyelia. Spine (Phila Pa 1976). 2001. 26: S119-27
7. Rothrock RJ, Lu VM, Levi AD. Syrinx shunts for syringomyelia: A systematic review and meta-analysis of syringosubarachnoid, syringoperitoneal, and syringopleural shunting. J Neurosurg Spine. 2021. 35: 535-45
8. Schaan M, Jaksche H. Comparison of different operative modalities in post-traumatic syringomyelia: Preliminary report. Eur Spine J. 2001. 10: 135-40
9. Tsitouras V, Sgouros S. Syringomyelia and tethered cord in children. Childs Nerv Syst. 2013. 29: 1625-34