- Department of Neurosurgery, Beneficencia Portuguesa de Sao Paulo, Sao Paulo, Brazil,
- Department of Pediatric, Dar Atteb Hospital, Zliten, Libya,
- Department of Neurosurgery, Neurosurgery Teaching Hospital, Baghdad, Iraq,
- Department of Neurosurgery, Dar Atteb Hospital, Zliten, Libya.
Correspondence Address:
Issa Ali Muftah Lahirish, Department of Neurosurgery, Beneficencia Portuguesa de Sao Paulo, Sao Paulo, Brazil.
DOI:10.25259/SNI_307_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Issa Ali Muftah Lahirish1, Faraj Ibrahim Alhdad2, Zahraa F. Al-Sharshahi3, Alhadi Milad Al-Tles4, Mohammed Mustafa Shmila2, Samer S. Hoz3, Mateus Reghin Neto1. Cerebellar mutism following head trauma: A case report and literature review. 06-Sep-2021;12:446
How to cite this URL: Issa Ali Muftah Lahirish1, Faraj Ibrahim Alhdad2, Zahraa F. Al-Sharshahi3, Alhadi Milad Al-Tles4, Mohammed Mustafa Shmila2, Samer S. Hoz3, Mateus Reghin Neto1. Cerebellar mutism following head trauma: A case report and literature review. 06-Sep-2021;12:446. Available from: https://surgicalneurologyint.com/surgicalint-articles/11095/
Abstract
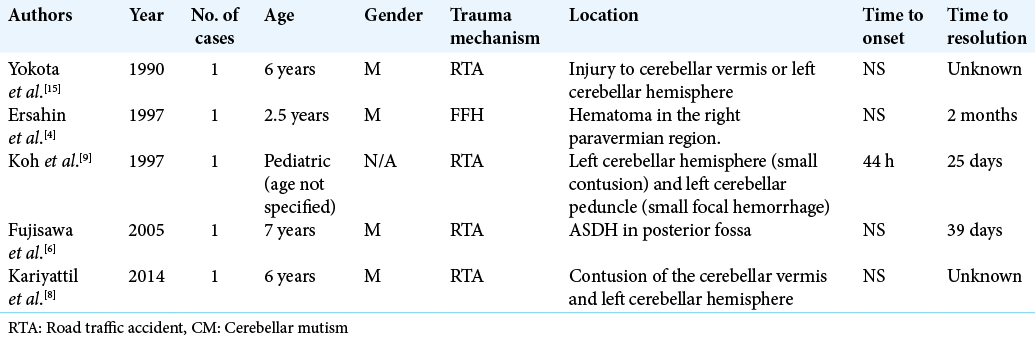
Background: Cerebellar mutism (CM) is defined as the lack of speech production, despite an intact state of consciousness and cognitive function, that happens secondary to a cerebellar insult. To the best of our knowledge, only five cases have thus far been described in the English literature. In this paper, we report the sixth incidence overall, which is also the first case of a CM associated with penetrating head injury. The relevant literature is reviewed and analyzed, our current knowledge of the neuroanatomical and functional relations is summarized, and potential future research endeavors are indicated.
Case Description: An 8-year-old girl was transferred to our hospital having had fallen on a rod that penetrated her neck behind the ear. An urgent computed tomography scan of the head revealed a right cerebellar contusion with surrounding edema. Three days later, she became mute but was still obeying commands. Repeat imaging showed a resolving cerebellar contusion with increased edema and mass effect. By day 9, she had uttered a few words. At 1-month follow-up, the child had regained normal speech.
Conclusion: Posttraumatic CM is a rare and probably underreported condition with only six documented cases to date. Although it may well be on the same spectrum as postoperative CM, further understanding of the exact mechanism, clinical course, and prognosis of this entity is bound to significantly improve the recovery and quality of life of head trauma patients.
Keywords: Cerebellar mutism, Head trauma, Penetrating traumatic brain injuries
INTRODUCTION
Cerebellar mutism (CM) is defined as the lack of speech production, despite an intact state of consciousness and cognitive function, that happens secondary to a cerebellar insult. Conventionally, the extension to this definition is “the absence of evidence for supra or nuclear cranial nerve or long tract injury.” However, with our current limited understanding of the anatomical substrate for the condition, this extension remains subject to alterations.[
CASE DESCRIPTION
An 8-year-old girl was transferred to our hospital having sustained a penetrating head and neck trauma. According to her parents, she was climbing on a side of a water tank outside when she fell and landed on a steel rod. In the emergency department, the patient was conscious, oriented, and screaming. She had a right-sided retromandibular penetrating wound.
Her other findings included right-sided lower motor neuron facial nerve palsy, neck spasm (torticollis), and right-sided cerebellar signs, namely, horizontal nystagmus, impaired finger to nose test, and dysdiadokokinesia were elicited.
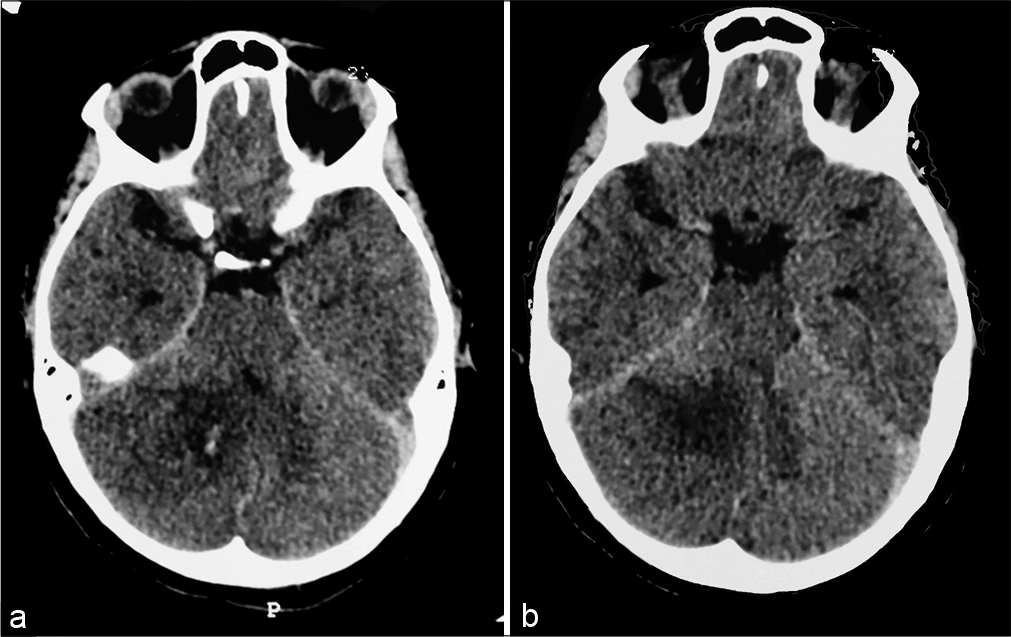
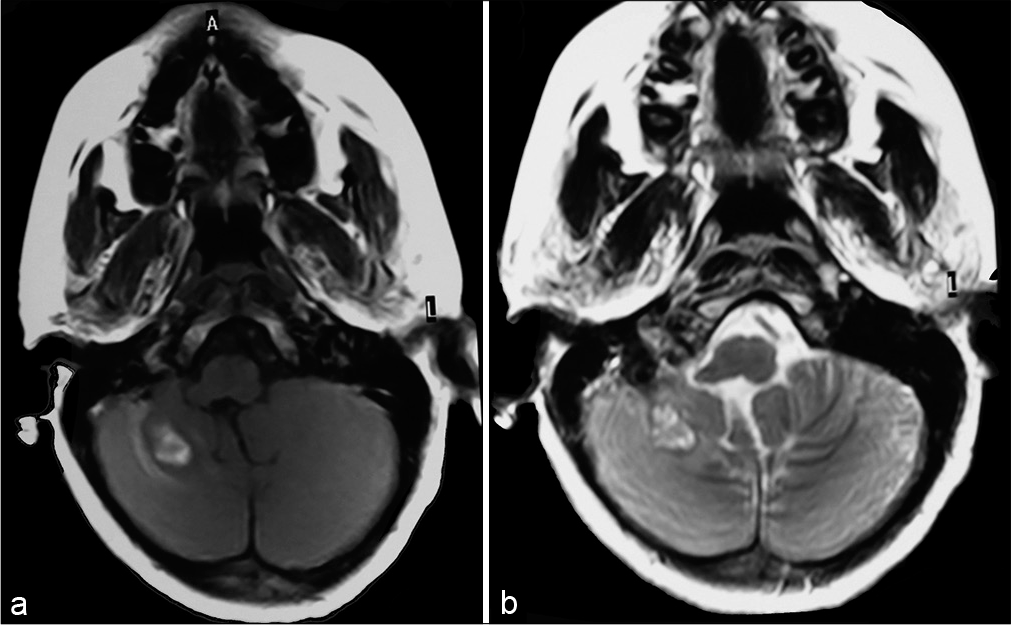
A computed tomography (CT) scan of the head revealed a skull base fracture through the floor of the posterior cranial fossa in association with right cerebellar contusion and edema. A cervical CT scan showed evidence of right parotid gland injury with surrounding hematoma (images not available).
Three days after admission, she became mute but was still obeying commands. Repeat imaging showed a resolving cerebellar contusion with increased edema and mass effect [
On the 7th admission day, she was ambulatory but with an ataxic gait and still could not speak. By day 9, she had spoken a few words and her neurological examination started to improve with a stationary facial exam. At her 1-month follow-up visit, the child had regained normal speech. Her facial palsy, which had persisted, was deemed secondary to direct injury to the extraforaminal segment of the facial nerve.
DISCUSSION
We reported a case of a child who was temporarily mute after penetrating trauma to the posterior fossa. The mental status and cognition of the patient remained intact throughout. Typical CM is characterized by an intact cranial nerve function. In this case, the patient had an injury to the parotid gland resulting in a coexisting CN VII palsy.
CM is characterized by a specific onset and chronology. It is usually diagnosed following a period of latency (1–6 days after the initial insult), with an average duration of 1 day– 4 months. It follows a variable recovery path after that before the subsequent gradual return of verbalization. In its typical form, CM is a temporary condition. However, the resumption of baseline speech function follows a variable course, with residual neurological deficits such as persistent dysarthria, ataxia, and behavioral changes being infrequently documented.[
As for the neuropathological and anatomical coordinates of CM, a number of studies have been published, with most data coming from postsurgical cases. A wide range of theories has thus been put in place and most of them focus on specific anatomical areas. For example, the involvement of median and paramedian structures,[
More recently, the involvement of particular tracts regardless of the specific anatomical areas per se has been identified as the most plausible hypothesis. Specifically, a bilateral disruption to the dentate-thalamocortical tract by ischemia and/or edema and the resultant cerebello-cerebral diaschisis has been cited by multiple authorities as the underlying mechanism.[
The first case of CM was reported in 1985 by Rekate et al.[
Although it is difficult to draw conclusions from such a small number of cases, a number of observations may be made here: first, the scarcity of cases and the unknown time of onset in most instances reflect the possible lack of reporting of such cases, partly due to the intubated, sedated status of trauma patients. The second observation is that six cases have so far been reported in the pediatric age group reflecting the age distribution of surgical CM. Third, there is a lack of evidence in long-term follow-up studies, with none of the patients undergoing any formal neurocognitive testing. Forth, the indistinct anatomical location of cerebellar injuries solidifies the current school of thought on the neuroanatomical coordinates of CM. Further anatomical, functional, and clinical studies are needed to better understand the basis and prognosis of CM.
CONCLUSION
We have reported the first case of a CM following a penetrating head injury. Posttraumatic CM is a rare and probably underreported condition with only six documented cases to date. Although it may well be on the same spectrum as postoperative CM, further understanding of the exact mechanism, clinical course, and prognosis of this entity is bound to significantly improve the recovery and quality of life of head trauma patients.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Catsman-Berrevoets CE, van Dongen HR, Zwetsloot CP. Transient loss of speech followed by dysarthria after removal of posterior fossa tumour. Dev Med Child Neurol. 1992. 34: 1102-9
2. Dailey AT, McKhann GM, Berger MS. The pathophysiology of oral pharyngeal apraxia and mutism following posterior fossa tumor resection in children. J Neurosurg. 1995. 83: 467-75
3. Dietze DD, Mickle JP. Cerebellar mutism after posterior fossa surgery. Pediatr Neurosurg. 1990. 16: 25-31
4. Erşahin Y, Mutluer S, Saydam S, Barçin E. Cerebellar mutism: Report of two unusual cases and review of the literature. Clin Neurol Neurosurg. 1997. 99: 130-4
5. Frassanito P, Massimi L, Caldarelli M, di Rocco C. Cerebellar mutism after spontaneous intratumoral bleeding involving the upper cerebellar vermis: A contribution to the physiopathogenic interpretation. Childs Nerv Syst. 2009. 25: 7-11
6. Fujisawa H, Yonaha H, Okumoto K, Uehara H, Ie T, Nagata Y. Mutism after evacuation of acute subdural hematoma of the posterior fossa. Childs Nerv Syst. 2005. 21: 234-6
7. Gudrunardottir T, Sehested A, Juhler M, Schmiegelow K. Cerebellar mutism: Review of the literature. Childs Nerv Syst. 2011. 27: 355-63
8. Kariyattil R, Rahim MI, Muthukuttiparambil U. Cerebellar mutism following closed head injury in a child. Sultan Qaboos Univ Med J. 2015. 15: e133-5
9. Koh S, Turkel SB, Baram TZ. Cerebellar mutism in children: Report of six cases and potential mechanisms. Pediatr Neurol. 1997. 16: 218-9
10. Mariën P, Ackermann H, Adamaszek M, Barwood CH, Beaton A, Desmond J. Consensus paper: Language and the cerebellum: An ongoing enigma. Cerebellum. 2014. 13: 386-410
11. Papavasiliou AS, Kotsalis C, Trakadas S. Transient cerebellar mutism in the course of acute cerebellitis. Pediatr Neurol. 2004. 30: 71-4
12. Rekate HL, Grubb RL, Aram DM, Hahn JF, Ratcheson RA. Muteness of cerebellar origin. Arch Neurol. 1985. 42: 697-8
13. Tamburrini G, Frassanito P, Chieffo D, Massimi L, Caldarelli M, di Rocco C. Cerebellar mutism. Childs Nerv Syst. 2015. 31: 1841-51
14. Wells EM, Khademian ZP, Walsh KS, Vezina G, Sposto R, Keating RF. Postoperative cerebellar mutism syndrome following treatment of medulloblastoma: Neuroradiographic features and origin. J Neurosurg Pediatr. 2010. 5: 329-34
15. Yokota H, Nakazawa S, Kobayashi S, Taniguchi Y, Yukihide T. Clinical study of two cases of traumatic cerebellar injury. No Shinkei Geka. 1990. 18: 67-70