- Department of Neurosurgery, Al-Ghassany Hospital, Fez,
- Department of Cardiovascular Diseases, Mohamed V University Hospital,
- Faculty of Medicine, Mohamed V University, Rabat, Morocco,
- Department of Neurosurgery, Paris Descartes University Hospital, Paris, France.
DOI:10.25259/SNI_147_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hilal Abboud, Hanane Kharbouch, Yasser Arkha, Mohamed Choukri. Cerebrospinal fluid fistula in a patient with chronic constipation related to an autonomic dysfunction and revealed by bacterial meningitis – A case report. Surg Neurol Int 18-Jul-2020;11:194
How to cite this URL: Hilal Abboud, Hanane Kharbouch, Yasser Arkha, Mohamed Choukri. Cerebrospinal fluid fistula in a patient with chronic constipation related to an autonomic dysfunction and revealed by bacterial meningitis – A case report. Surg Neurol Int 18-Jul-2020;11:194. Available from: https://surgicalneurologyint.com/surgicalint-articles/cerebrospinal-fluid-fistula-in-a-patient-with-chronic-constipation-related-to-an-autonomic-dysfunction-and-revealed-by-bacterial-meningitis-a-case-report/
Abstract
Background: Cerebrospinal fluid (CSF) fistula represents a rare neurosurgical entity that can be defined as a communication between the subarachnoid space and nasal fossa or less commonly the ear cavity. It can be spontaneous without an evident etiology or secondary following a skull base surgery or trauma. The early diagnosis of spontaneous forms remains a challenge as clinical signs (e.g., unilateral rhinorrhea) can be absent or neglected by patients and can result in meningitis.
Case Description: Here, we report the case of a 31-year-old man with chronic constipation complicated by chronic intracranial hypertension, and resulting in rhinorrhea with bacterial meningitis. The etiological assessment of chronic constipation retained an autonomic dysfunction with sympathetic hyperactivity (e.g., pure autonomic failure) as an underlying cause. Beta-2 transferrin testing associated with cerebral magnetic resonance imaging and computed tomography scan confirmed the diagnosis and localization of the fistula at the cribriform plate. The patient underwent an endoscopic endonasal approach with a repair of fistula. He presented with recurrent rhinorrhea 17 months later which required a surgical revision along with CSF diversion with a ventriculoperitoneal shunt.
Conclusion: Although rare, autonomic dysfunction can result in chronic constipation in young patients, with intermittent or permanent intracranial hypertension, leading to CSF leaks. The early identification and treatment of the underlying etiology may prevent severe complications and improve the management and outcome of CSF fistula patients.
Keywords: Constipation, Cerebrospinal fluid rhinorrhea, Meningitis, Pure autonomic failure
INTRODUCTION
Cerebrospinal fluid (CSF) rhinorrhea can be defined as CSF egress from a communication between the subarachnoid space and nasal fossa. It occurs preferentially in osteomeningeal weakened sites within the skull base and is rarely spontaneous without an evident etiology, or more often secondary following a craniofacial trauma or skull base surgery.[
Autonomic dysfunction with sympathetic hyperactivity represents an unusual cause of spontaneous fistulas, which could be revealed by unilateral rhinorrhea or diagnosed following repetitive bacterial meningitis, and resulting in severe complications.[
Biological assessment by beta-2 transferrin testing and cerebral computed tomography (CT) scan coupled to magnetic resonance imaging (MRI) helps in diagnosis and localization of the defect.[
Management strategy is varying according to clinical and radiological features of fistula; the endoscopic endonasal approach combines low morbidity and excellent results.[
CASE PRESENTATION
A 31-year-old man with chronic constipation of 15 years duration presents 6 mounts ago an intermittent clear and watery right nasal discharge accentuated by excessive effort during defecation. Five days before the consultation in the emergency department, the patient reported a persistent headache despite analgesic treatment, with nausea and fever. Clinical examination showed neck rigidity, the diagnosis of meningitis is then retained; we carefully analyzed the patient medical history and found the notion of the right nasal fossa rhinorrhea which was objectified by Valsalva manoeuvers.
We performed a cerebral CT scan and CSF analysis which found a hyperproteinorachia, hypoglycorrachia, and many diplococci suggesting pneumococcal meningitis. The patient underwent an intravenous antibiotherapy based on ceftriaxone and the evolution was favorable.
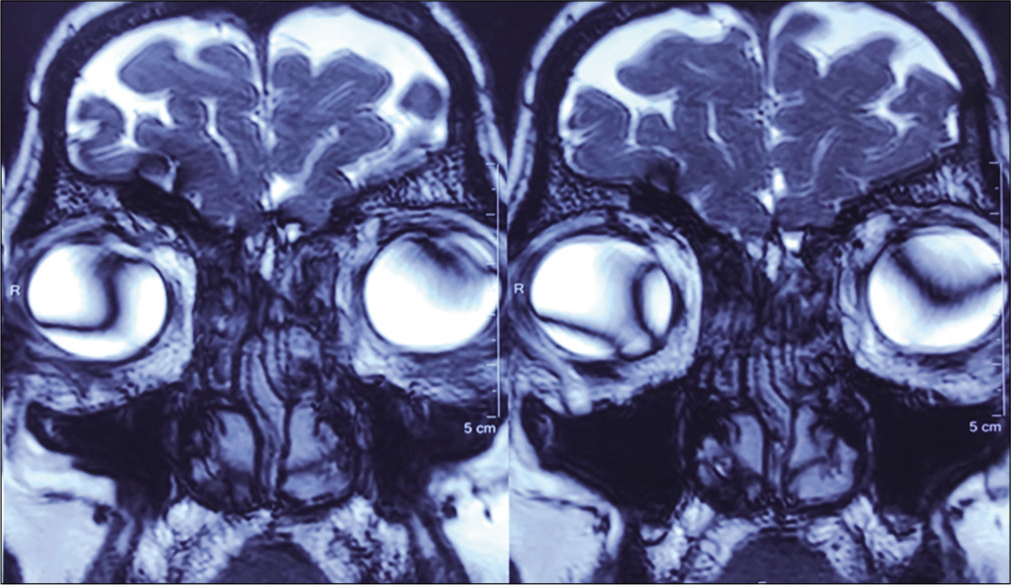
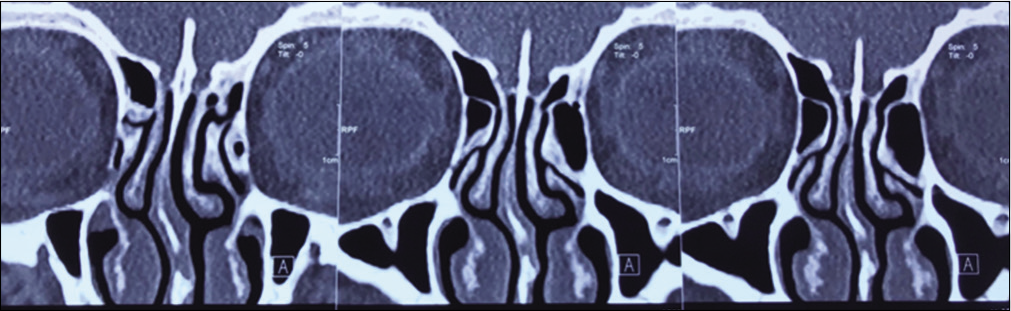
The clinical examination and paraclinical investigations found a chronic constipation complicated by internal and external hemorrhoids with no abnormalities in the colonoscopy performed by a proctologist. The endocrine assessment, including thyroid and pituitary testing, showed no abnormalities. Radiologic assessment including T2-weighted cerebral MRI and CT scan showed a bony defect in the right side of the cribriform plate [
An ECG with Holter ECG showed an asymptomatic and well tolerated sinusal bradycardia, with no echocardiographic abnormalities, the global cardiac examination with autonomic nervous system assessment was carried by a cardiologist and objectified a rare autonomic dysfunction entity with sympathetic hyperactivity designated as: pure autonomic failure (PAF).
The patient underwent an endoscopic endonasal approach with a repair of the leak, there were no signs of recurrence during the early postoperative period; however, the patient kept intermittent chronic constipation and presented with a recurrent rhinorrhea 17 months following surgery, we performed a cerebral CT scan, a preoperative spinal drainage during 72 h with CSF analysis and ICP measuring, we found an intermittent elevated ICP (e.g., opening pressure > 45 cm H2O (33 mmHg)) with sterile CSF, and we performed a CSF ventriculoperitoneal shunting with endonasal surgical revision. The postoperative course was uneventful with a good outcome at 3 months following the second surgery.
DISCUSSION
The most common form of CSF fistula is secondary, following craniofacial trauma or skull base surgery. The spontaneous form is infrequent and occurs in <5% of CSF fistula patients, it occurs mostly in the sphenoidal bone (60%) and can result in meningitis in 12%.[
The pathophysiology of spontaneous CSF fistula remains unknown; however, all factors, leading to increased intra- abdominal and/or intra-thoracic pressure, including chronic constipation, could result in permanent or intermittent ICH which could predispose to spontaneous CSF leaks, this is a very rare condition, but reported in obese patients.[
Chronic constipation is a very common symptom that affects about 25% of the general population, it can be idiopathic, by far the most common form in young patients,[
In our patient, the clinical and paraclinical assessment retained the diagnosis of pure autonomic failure, which is a rare sporadic neurodegenerative disorder of autonomic nervous system with no evidence of CNS dysfunction, clinically characterized by orthostatic hypotension, digestive disorders (e.g., constipation or diarrhea), and genitosphincterian perturbations. This rare autonomic disorder is caused by neuronal degeneration of pre- and postganglionic sympathetic and parasympathetic neurons in the thoracic spinal cord and paravertebral autonomic ganglia and is associated with very low plasma norepinephrine (NE) level suggesting widespread sympathetic denervation.[
The early diagnosis of spontaneous CFS fistula remains a challenge as a minimal or posterior discharge can be neglected by the patient or felt only as a salty pharyngeal taste. In our case, the CSF fistula has been diagnosed following the first meningitis episode; despite, the patient had an intermittent rhinorrhea 6 months ago.
Laboratory assessment, including beta-2 transferrin testing associated with radiologic features in cerebral MRI and CT scan, helps to confirm and localize the fistula and identify ICH signs. Radiologic assessment is also important to eliminate other causes of CSF leakage such as a skull base malformation or tumor.[
The main goal of treatment is to repair the bony and meningeal defect to prevent recurrent bacterial meningitis; the management strategy varies according to clinical and radiological features of CSF fistula. Adjuvant medical treatment based on Acetazolamide with bed rest, whether or not associated with spinal drainage, is proposed first to all patients. Abundant spontaneous rhinorrhea often requires a surgical endoscopic approach that combines low morbidity and excellent results reaching 90% of closure after the first surgery.[
Some CSF fistulas could regress spontaneously after the first episode of meningitis; this may appear as a consequence of fibrosis following the inflammatory episode of meningitis.
VPS was reported as the only surgical modality for treating some cases of fistula;[
In our patient, an initial endoscopic endonasal approach has been performed with a repair of the defect using fascia lata, there were no signs of recurrence during the 1st 17 months following surgery. However, the patient kept chronic intermittent constipation with an intermittent elevated ICP, leading to recurrent rhinorrhea; he underwent a surgical revision with ventriculoperitoneal shunting of CSF. The postoperative course was uneventful with a good outcome at 3 months following the second surgery.
CONCLUSION
There seems to be a logical link between pure autonomic failure and CSF fistula. Hence, although rare, spontaneous CSF fistula may appear as a consequence of sustained intracranial hypertension associated with chronic constipation in patients with pure autonomic failure. The early identification and appropriate management of the autonomic dysfunction could prevent severe complications and improve the treatment and outcome of CSF fistula patients.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Almansa AH, Cutillas AR, Infante AJ, Gómez JR, Busquier H. Idiopathic intracranial hypertension and spontaneous cerebrospinal fluid fistula. Usefulness of intracranial pressure monitoring. Neurocirugia (Astur). 2017. 28: 93-6
2. Aroca AC, Cabrerizo JR, Delago MJ, Solench HM. Spontaneous cerebrospinal fluid fistula in the clivus. Eur Ann Otorhinolaryngol Head Neck Dis. 2017. 134: 431-4
3. Brown TP. Pure autonomic failure. Pract Neurol. 2017. 17: 341-8
4. Coon EA, Singer W, Low PA. Pure autonomic failure. Mayo Clin Proc. 2019. 94: 2087-98
5. Darouassi Y, Touati MM, Chihani M, Akhaddar A, Ammar H, Bouaity B. Spontaneous cerebrospinal fluid leak of the sphenoid sinus mimicking allergic rhinitis, and managed successfully by a ventriculoperitoneal shunt: A case report. J Med Case Rep. 2016. 10: 308-
6. Elrahman HA, Malinvaud D, Bonfils NA, Daoud R, Mimoun M, Bonfils P. Endoscopic management of idiopathic spontaneous skull base fistula through the clivus. Arch Otolaryngol Head Neck Surg. 2009. 135: 311-5
7. Giannetti AV, Santiago AP, Becker HM, Guimarães RE. Comparative study between primary spontaneous cerebrospinal fluid fistula and late traumatic fistula. Otolaryngol Head Neck Surg. 2011. 144: 463-8
8. Kortbus MJ, Roland JT, Lebowitz RA. Sphenoid sinus cerebrospinal fluid leak: Diagnosis and management. Oper Tech Otolayngol Head Neck Surg. 2003. 14: 207-11
9. Kutz JW, Tolisano AM. Diagnosis and management of spontaneous cerebrospinal fluid fistula and encephaloceles. Curr Opin Otolaryngol Head Neck Surg. 2019. 27: 369-75
10. Mathias CJ, Mallipeddi R, Bleasdale-Barr K. Symptoms associated with orthostatic hypotension in pure autonomic failure and multiple system atrophy. J Neurol. 1999. 246: 893-8
11. McCallum IJ, Ong S, Mercer-Jones M. Chronic constipation in adults. BMJ. 2009. 338: b831-
12. Oakley GM, Orlandi RR, Woodworth BA, Batra PS, Alt JA. Management of cerebrospinal fluid rhinorrhea: An evidence-based review with recommendations. Int Forum Allergy Rhinol. 2016. 6: 17-24
13. Quenom K, Bouayad B, Laghmari M, Sogoba Y, Coulibaly O, Hossini A. Non invasive treatment of spontaneous cerebrospinal fluid lack age associated with benign intracranial hypertension. Afr J Neurol Sci. 2008. 27: 122-8
14. Tack J, Müller-Lissner S, Stanghellini V, Boeckxstaens G, Kamm MA, Simren M. Diagnosis and treatment of chronic constipation-a European perspective. Neurogastroenterol Motil. 2011. 23: 697-710
15. Thaisetthawatkul P. Pure autonomic failure. Curr Neurol Neurosci Rep. 2016. 16: 74-
16. Wang EW, Vandergrift WA, Schlosser RJ. Spontaneous CSF leaks. Otolaryngol Clin North Am. 2011. 44: 845-56