- Departamento de Neurocirugía, Centro de investigación y entrenamiento en Neurocirugía (CIEN), Hospital Universitario de la Samaritana, Universidad el rosario escuela de medicina, Bogotá, Colombia.
Correspondence Address:
Juan Felipe Abaunza-Camacho, Departamento de Neurocirugía, Centro de investigación y entrenamiento en Neurocirugía (CIEN), Hospital Universitario de la Samaritana, Universidad el rosario escuela de medicina, Bogotá, Colombia.
DOI:10.25259/SNI_385_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Esteban Ramirez-Ferrer, Juan Felipe Abaunza-Camacho, Andres Felipe Pineda-Martinez, Maria Paula Aguilera-Pena, William Mauricio Riveros-Castillo, Leonardo Laverde-Frade. Cerebrospinal fluid leak following penetrating trauma to the spine without neurological deficit: A case report. 29-Jul-2022;13:327
How to cite this URL: Esteban Ramirez-Ferrer, Juan Felipe Abaunza-Camacho, Andres Felipe Pineda-Martinez, Maria Paula Aguilera-Pena, William Mauricio Riveros-Castillo, Leonardo Laverde-Frade. Cerebrospinal fluid leak following penetrating trauma to the spine without neurological deficit: A case report. 29-Jul-2022;13:327. Available from: https://surgicalneurologyint.com/surgicalint-articles/11751/
Abstract
Background: Posttraumatic spinal cerebrospinal fluid leak (CSFL) without neurological deficit is a rare entity. Historically, the first-line treatment is a nonsurgical approach, which includes Trendelenburg positioning, carbonic anhydrase inhibitor (acetazolamide), and subarachnoid catheter, with a high successful rate of leak correction. However, in some cases, this first-line treatment could fail, being necessary the surgical approach.
Case Description: A 23-year-old male with a recent stab wound to his lumbar region, complained of positional headache and fluid outflow through his wound. On physical examination, an active CSFL was detected without evidence of neurologic deficit. Imaging studies showed a CSF collection extending from the right L4 lamina to the subcutaneous tissue. CSF studies revealed bacterial meningitis. The treatment with carbonic anhydrase inhibitors, Trendelenburg position, lumbar subarachnoid catheter, and antibiotics was initiated. Failure of conservative measures prompted a surgical treatment to resolve the CSFL. Intraoperatively, a dura mater defect was identified, and an autologous paravertebral muscle flap was used for water-tight closure of the defect. The patient recovered without further complications and with CSFL resolution.
Conclusion: Even though the nonsurgical approach is the first-line of treatment of traumatic CSFL cases, failures can occur. The evidence of a CSF trajectory in imaging studies could be a predictor of treatment failure of the nonsurgical treatment. The surgical treatment as second-line treatment has outstanding results regarding CSFL correction and should be considered when the prediction rate to nonsurgical approach failure is high.
Keywords: Cerebrospinal fluid leak, Headache, Lumbosacral region, Trauma, Young adult
INTRODUCTION
In the United States, spinal cord injury incidence is 17,700 cases/year, and only 0.8% correspond to nonmissile penetrating injuries.[
The severity of neurological compromise in non-missile penetrating injuries is variable. Complete injury is found in 19–38% of patients, and Brown-Séquard Syndrome is observed in 31–55% of them.[
Here, we describe an unusual case of lumbar spine stab injury in a young adult with consequent penetrating fracture of the lamina and secondary CSFL with no neurological deficit that required multimodal intervention, including nonsurgical and surgical treatment.
CASE DESCRIPTION
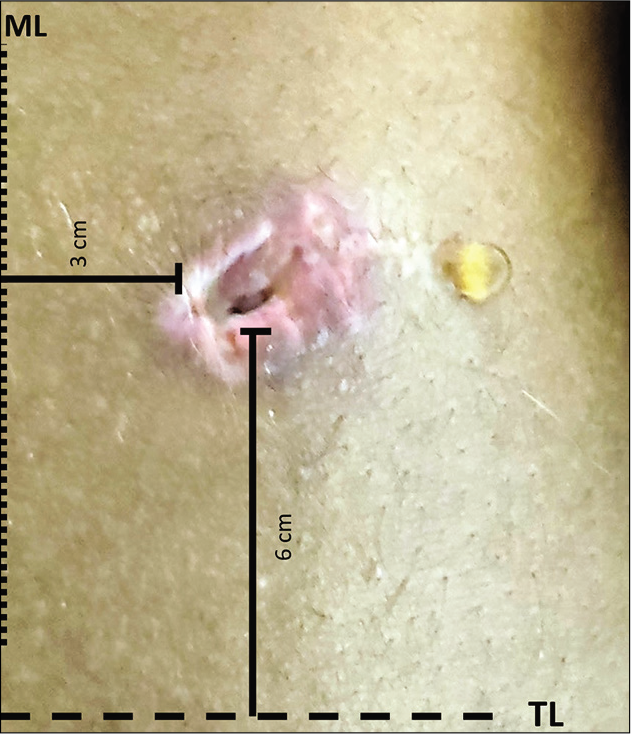
A 23-year-old male stabbed in the right paravertebral lower-back region, 5 days before admission, comes to the emergency room. He presented with a headache that worsened with sitting and standing but was relieved in the supine position. In addition, he noted clear fluid flowing out from his wound. Physical examination revealed a 3-cm skin wound at the right paravertebral lower-back region, 3 cm from the middle line, and 6 cm cephalic from the Tuffier’s line leaking clear fluid [
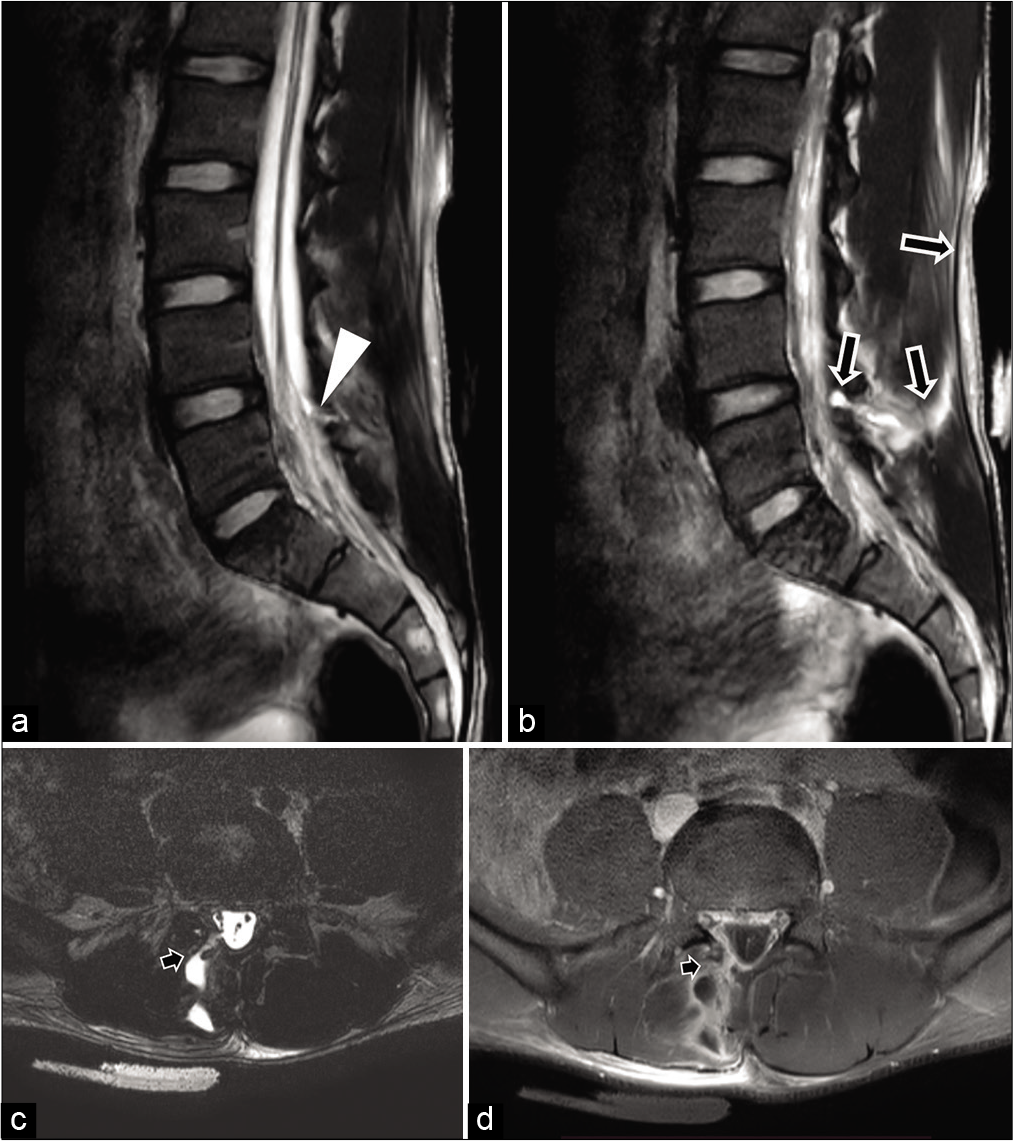
Lumbar puncture at the L3–L4 level was performed. Low opening cerebrospinal fluid (CSF) pressure, pleocytosis, high protein, and low glucose were found. Bacterial meningitis was highly suspected, and broad-spectrum antibiotics were initiated. Spine X-rays documented no foreign body. T2-weighted and T1-contrast-enhanced Magnetic Resonance Imaging (MRI) were performed and confirmed a traumatic CSFL extending from the inferior border of the L4 right lamina, including the paravertebral longissimus, iliocostalis muscles, up to the skin [
Figure 2:
(a and b) Midsagittal view of a T2-weighted (a). MRI of the lumbar spine showing dural tear (white arrowhead) and L4 right lamina relation to the CSFL trajectory (b) (black arrows). (c and d) Axial view of a T2-weighted (c) and contrast-enhanced T1-weighted (d) MRI of the lumbar spine exhibiting paravertebral rupture of the longus and iliocostalis muscles related to dural tear and lamina fracture up to epidermis (black arrow).
Nonsurgical treatment for traumatic CSFL was indicated, including Trendelenburg positioning, carbonic anhydrase inhibitor (acetazolamide), subarachnoid catheter at L3–L4 level for 7 days, skin wound closure, and 14 days of broad-spectrum antibiotics. No bacterial typification was disclosed, and normal control CSF chemistry was obtained after antibiotic therapy completion.
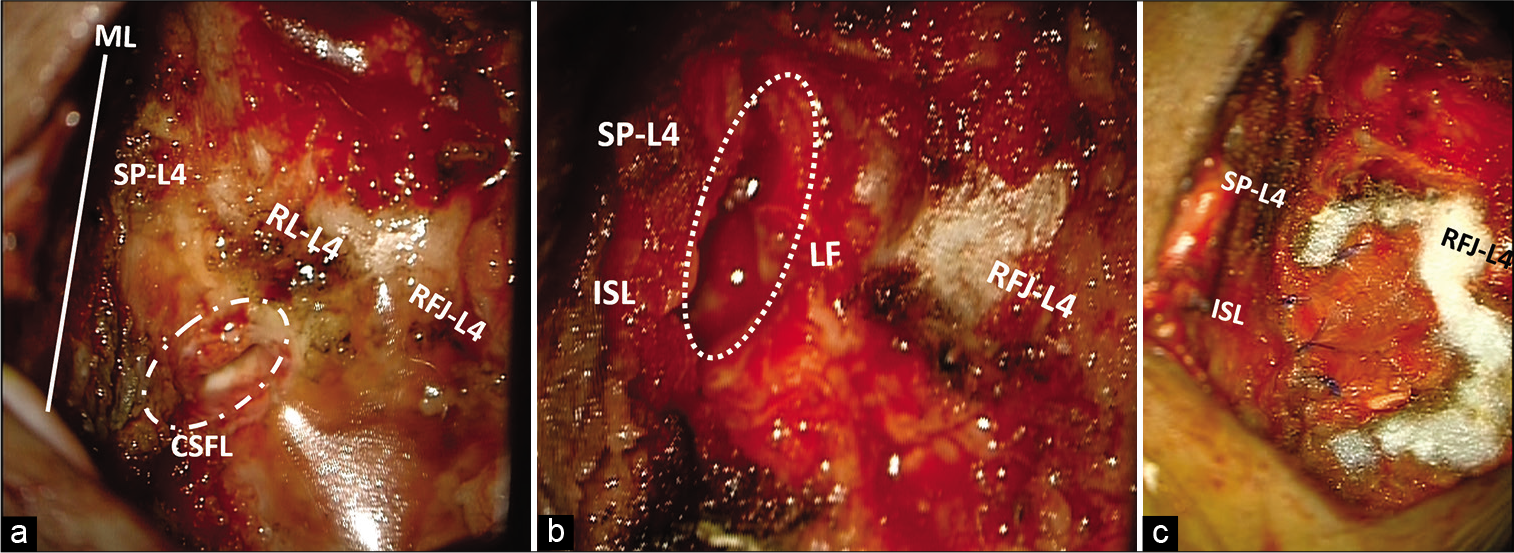
Three days after removing the subarachnoid catheter, the recurrence of the CSFL was noted [
Figure 4:
(a and b) Midline (ML) approach, right paraspinal dissection with exposure of vertebral L4–L5 space. Vertebral L4 Spinal process (SP-L4), right lamina (RL-L4), right facet joint (RFJ-L4), and their relations with the CSFL (white dotted circle) were exposed. Right L4 laminectomy was performed, exposure of the interspinal ligament (ISL) and ligament Flavors (LF) shows the compromised in the traumatic CSFL route until the dural defect in the medial segment (White dotted circle). (c) Paraspinal pedicle flap was obtained from the erector spinae and thoracolumbar fascia fixed to the SP-L4, ISL, and the LF assisted with hemostatic material in the peripheral areas.
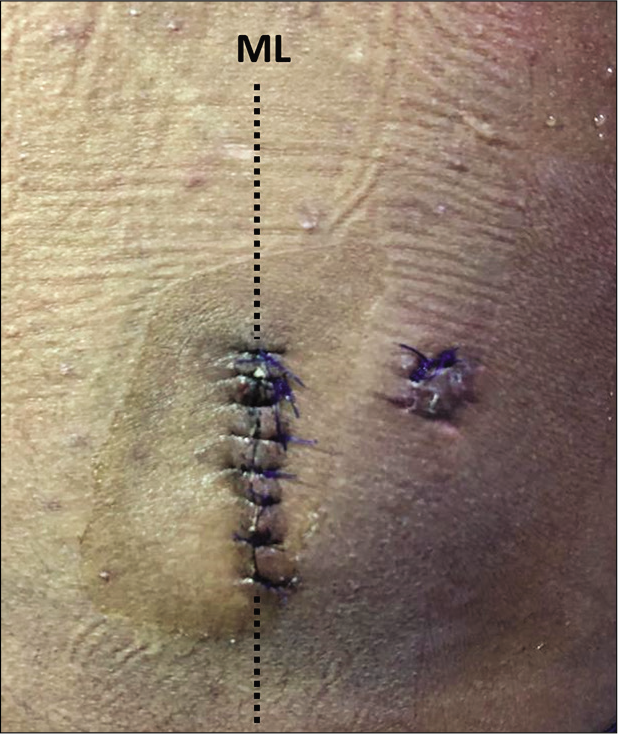
Postoperatively, resolution of the subcutaneous collection and headache was noted [
DISCUSSION
Spinal CSFL incidence is close to five out of 100,000 cases/year in the United States.[
Patients with traumatic dural tears had a high likelihood of neurologic injury. In a study published in 2014, Luszczyk et al. found that a complete neurologic injury was present in 48.7% of patients presenting with traumatic dural tears. Moreover, they found that in patients with complete neurologic injury, 29% had traumatic injuries at the lumbosacral region.[
About traumatic spinal injuries without neurologic deficit, in a retrospective study of 22 patients, Jacobsohn et al. found that only 4.5% patients with stabbing injuries to the spinal cord presented without any neurological deficit.[
The most frequent clinical manifestation of CSFL is a classic intracranial hypotension positional headache. Other common symptoms include nausea, vomiting, sensation of fluid outflow through the wound, soft-tissue fluid collection, vertigo, and among others.[
Plain X-rays should be obtained for all patients to exclude a foreign body’s presence (e.g., metallic objects that must be withdrawn before an MRI is performed).[
Other useful diagnostic tools to identify the leak source include: immunofixation or electrophoresis for beta-2 transferrin, computerized tomography (CT) myelography, cisternography with CT, or radionuclide cisternography.[
Meningitis is a frequent complication in traumatic CSFL.[
Trendelenburg’s position has been described as part of the nonsurgical management for two reasons. First, it reduces hydrostatic pressure applied to the dural defect and eases its closure. Second, it prevents pneumocephalus.[
CSFL requires a challenging, timely, and cautious workup and treatment. In the literature, a nonsurgical approach is the first-line treatment option to reduce the CSF outflow. However, there is no literature about CSFL characteristics that would predict a nonsurgical approach’s failure. At present, the only indication for a surgical approach is in cases, where retained foreign bodies require extraction.
In imaging studies, the evidence of a CSF trajectory from the dural sac through the soft tissues, up to the skin defect, could be considered a predictor of good results utilizing a surgical approach and hence, to be considered a first-line treatment.[
If surgical management is indicated, there are many possible options to treat a CSFL, including direct primary closure of the dura, direct replacement of collagen patches, fibrin glue, and blood-soaked gelatin sponge. No significant differences between techniques have been described.[
In our case, we were able to identify the dural tear under the microscope, which allowed us to achieve a primary closure under direct visualization and achieve better outcomes than when the tear is not identified.[
CONCLUSION
The absence of neurologic deficit in traumatic spine CSFL and the evidence of the CSFL trajectory on imaging studies are uncommon. The latter, could be associated with a low correction rate using a nonsurgical approach, being the surgical exploration approach as an optimal intervention for the leakage’s complete resolution. Further studies are needed to establish specific CSFL features that will predict a successful leakage correction rate using either a conservative or a surgical approach.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Amaya CC, Meré JA, Bustamante AC, Ovalle RM, Alonzo F. Stab injury to the spine without neurological involvement: A report of a rare case. J Surg Case Rep. 2021. 2021: rjab163
2. Brazdzionis J, Ogunlade J, Elia C, Wacker MR, Menoni R, Miulli DE. Effectiveness of method of repair of incidental thoracic and lumbar durotomies: A comparison of direct versus indirect repair. Cureus. 2019. 11: e5224
3. Carpenter H, Hurndall KH, Asokan AK, Fernandes R. Penetrating trauma causing cerebrospinal fluid leak without nerve root damage. BMJ Case Rep. 2018. 2018: bcr2017221461
4. Gandhi J, DiMatteo A, Joshi G, Smith NL, Khan SA. Cerebrospinal fluid leaks secondary to dural tears: A review of etiology, clinical evaluation, and management. Int J Neurosci. 2021. 131: 689-95
5. Jacobsohn M, Semple P, Dunn R, Candy S. Stab injuries to the spinal cord: A retrospective study on clinical findings and magnetic resonance imaging changes. Neurosurgery. 2007. 61: 1262-7
6. Luszczyk MJ, Blaisdell GY, Wiater BP, Bellabarba C, Chapman JR, Agel J. Traumatic dural tears: What do we know and are they a problem?. Spine J. 2014. 14: 49-56
7. McCudden CR, Senior BA, Hainsworth S, Oliveira W, Silverman LM, Bruns DE. Evaluation of high resolution gel β2-transferrin for detection of cerebrospinal fluid leak. Clin Chem Lab Med. 2013. 51: 311-5
8. Menon SK, Onyia CU. A short review on a complication of lumbar spine surgery: CSF leak. Clin Neurol Neurosurg. 2015. 139: 248-51
9. Rahamimov N, Mulla H, Freiman S. Cerebrospinal fluid leakage and pneumocephalus secondary to spine stab wounds. J Orthop Traumatol. 2010. 11: 57-9
10. Styliaras JC, Dalyai R, Amgad H, Sharan A, Harrop J. Cerebrospinal fluid leaks from penetrating injuries: Diagnosis and treatment. ArgoSpine News J. 2012. 24: 183-7
11. Wallace DJ, Sy C, Peitz G, Grandhi R. Management of non-missile penetrating spinal injury. Neurosurg Rev. 2019. 42: 791-8