- Departments of Neurosurgery, All India Institute of Medical Sciences, New Delhi, India.
- Departments of Neuroradiology, All India Institute of Medical Sciences, New Delhi, India.
Correspondence Address:
Sachin A. Borkar
Departments of Neurosurgery, All India Institute of Medical Sciences, New Delhi, India.
DOI:10.25259/SNI_346_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ravi Sharma, Sachin A. Borkar, Manoj Phalak, S. Leve Joseph, Shashank S. Kale. Cervical alignment following laminoplasty for cervical spondylotic myelopathy. 02-Aug-2019;10:156
How to cite this URL: Ravi Sharma, Sachin A. Borkar, Manoj Phalak, S. Leve Joseph, Shashank S. Kale. Cervical alignment following laminoplasty for cervical spondylotic myelopathy. 02-Aug-2019;10:156. Available from: http://surgicalneurologyint.com/surgicalint-articles/9550/
Abstract
Background: Laminoplasty can result in the loss of cervical lordosis (LOCL) or the development of kyphosis after surgery. Here, we evaluated the clinical and radiological parameters involved in predicting the postoperative LOCL following laminoplasty in patients with cervical spondylotic myelopathy (CSM) and ossification of the posterior longitudinal ligament (OPLL).
Methods: For 50 patients with CSM and 35 with OPLL undergoing laminoplasty, preoperative and 1-year postoperative X-rays were obtained to determine the incidence and risk factors contributing to postoperative LOCL. The patients were divided into two groups depending on whether the preoperative T1 slope was above or below the median preoperative T1S (26°); Group A – high T1 slope group (n = 40) and Group B – low T1 slope group (n = 45).
Results: Following laminoplasty, Group A patients had significantly higher preoperative lordosis (C2-C7 Cobb’s angle) (P = 0.001) and significantly higher LOCL (P = 0.02) versus Group B patients with low T1 slopes. The preoperative T1 slope was also found to be significantly correlated with the preoperative C2-C7 Cobb’s angles (R = 0.619, P = 0.001), LOCL (R = 0.487, P = 0.001), and preoperative C2-C7 sagittal vertical axis (R = 0.480, P = 0.001). Utilizing multivariate analysis and a generalized linear model, the preoperative T1 slope significantly impacted the Oswestry disability index (ODI) index (P = 0.002) and frequency of LOCL (P = 0.001) following laminoplasty.
Conclusion: The preoperative T1 slope is a significant predictor of the LOCL and change in ODI following laminoplasty for CSM/OPLL utilizing a cutoff value of 29.5°.
Keywords: C2-C7 Cobb’s angle, C2-C7 lordosis, C2-C7 sagittal vertical axis, C2-C3 disc angle, Cervical laminoplasty, Loss of cervical lordosis, T1 slope, Kyphosis
INTRODUCTION
Cervical spondylotic myelopathy (CSM) and ossification of the posterior longitudinal ligament (OPLL) may both be safely managed with laminoplasty.[
MATERIALS AND METHODS
Clinical data
This study was conducted from 2013 to 2018 and included 50 patients with CSM and 35 with OPLL. All the patients underwent clinical, X-ray (flexion/extension), and noncontrast computed tomography evaluations of the cervical spine for CSM/OPLL preoperatively. Males comprised 90% of the study population and averaged 58.2 ± 11.2 years of age. Patients were symptomatic for an average of 22 ± 16 months and were followed an average of 31 ± 15 months (range of 12–60 months). Patients were followed for a minimum of 1 postoperative year. All underwent 2-4-level hinge door laminoplasty using titanium miniplates to keep hinged side open. The radiological parameters were measured using Centricity Enterprise PACS WV 3.0 software [
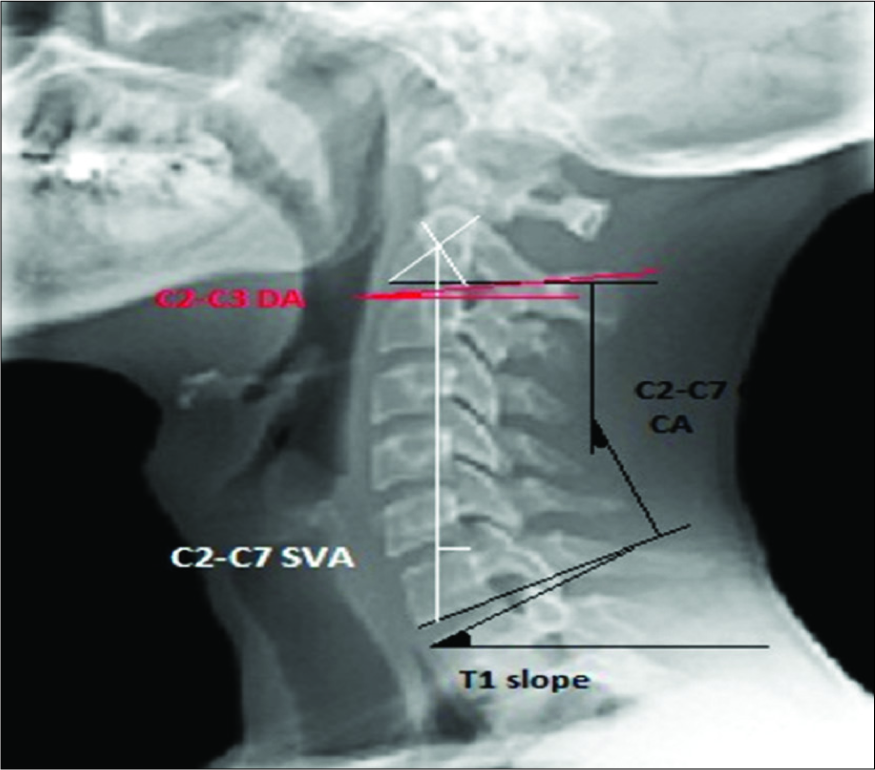
Figure 1:
Lateral X-ray of cervical spine showing measured radiological parameters. C2–7 Cobb angle is defined as the angle between lines extended parallel to the inferior endplate of C-2 and C-7 on the standing lateral radiograph of the cervical spine. Cervical sagittal vertical alignment was defined as the perpendicular distance between a plumb line dropped from the center of C-2 (or dens) and the posterosuperior aspect of C7 (C2–7 sagittal vertical axis). T1 slope is measured as the angle between the horizontal plane and the superior endplate of T1 vertebra. C2-C3 disc angle is measured as the angle between the line drawn parallel to the C2-C3 disc space and the line drawn parallel to the floor on standing X-ray.
Postoperative follow-up
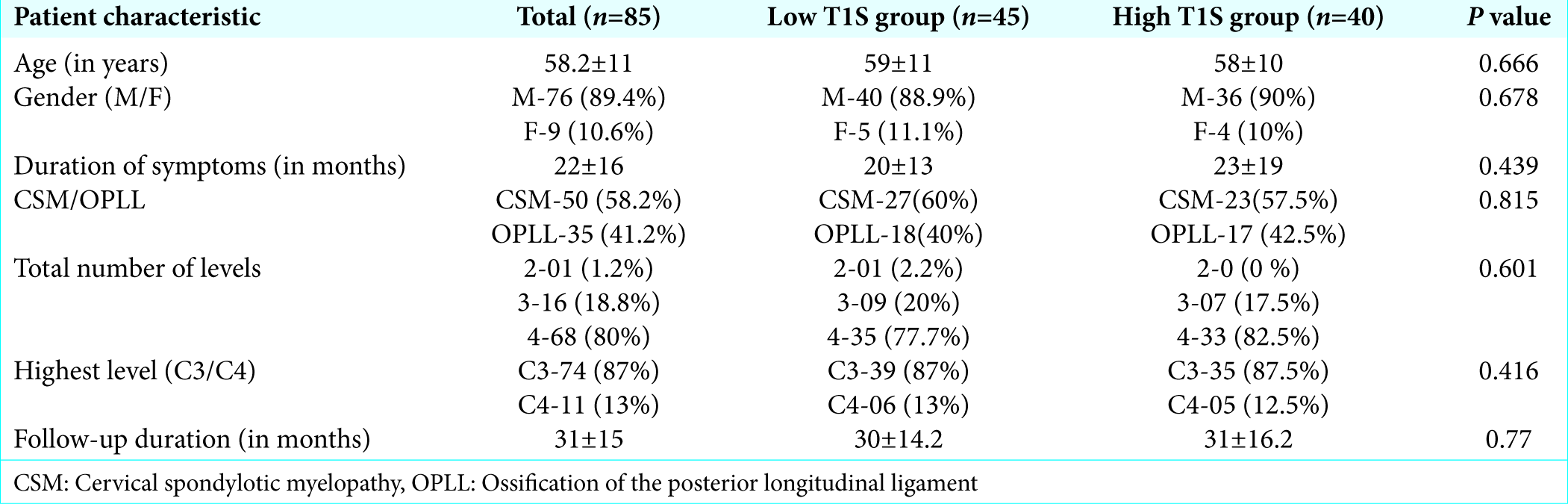
Postoperatively, patients were followed for a minimum period of 1 year and included clinical assessments based on a modified Japanese Orthopedic Association (mJOA) score and Oswestry disability index (ODI). Cervical X-rays were utilized to divide patients into two groups depending on whether the preoperative T1 slope was above or below the median preoperative T1S (26°); Group A: high T1 slope group and Group B: low T1 slope group [
Statistical analysis
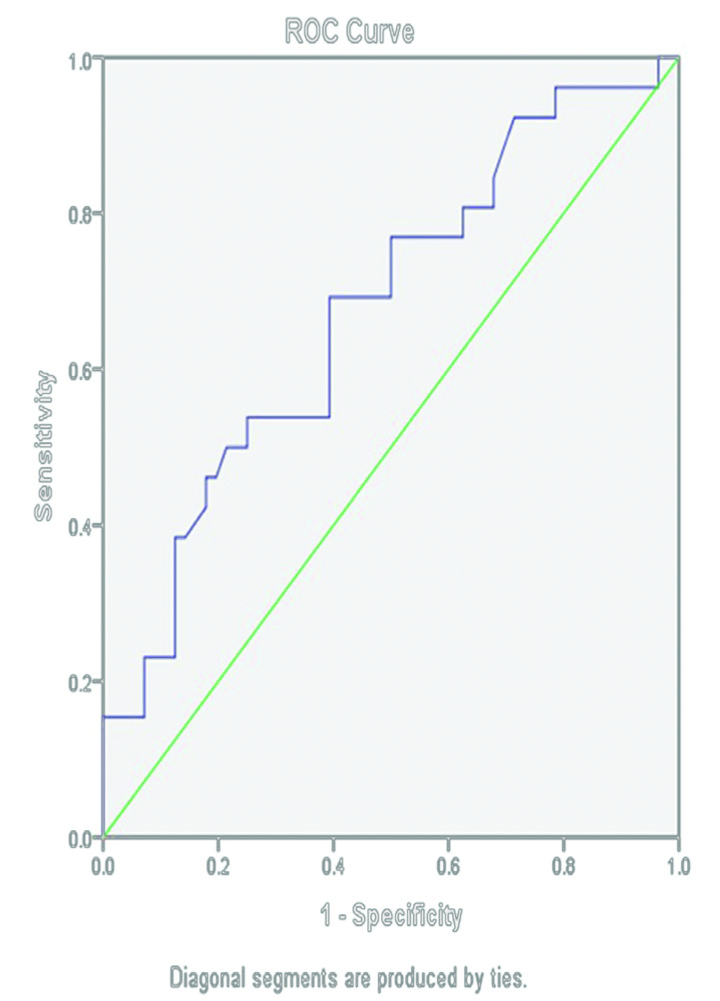
Univariate analysis was performed using Chi-square test/ Fischer’s exact test, Student’s t-test, and Pearson’s product moment correlation coefficient. A generalized linear model was used for multivariate analysis and receiver operator characteristics curve was generated to identify the best cutoff for T1S to predict LOCL. The data were analyzed using IBM SPSS Statistics package version 20.
RESULTS
Comparison of clinical and radiological parameters according to preoperative T1S
The patients in Group A also have a significantly higher preoperative lordosis (C2-C7 Cobb’s angle) and preoperative C2-C7 sagittal vertical axis (SVA) versus Group B (P = 0.001 for both). Group A also showed significantly higher LOCL following laminoplasty versus Group B (P = 0.02). Further, the incidence of LOCL of more than 5° in Group A patients was 45% (P = 0.006) significantly higher than Group B (17%) [
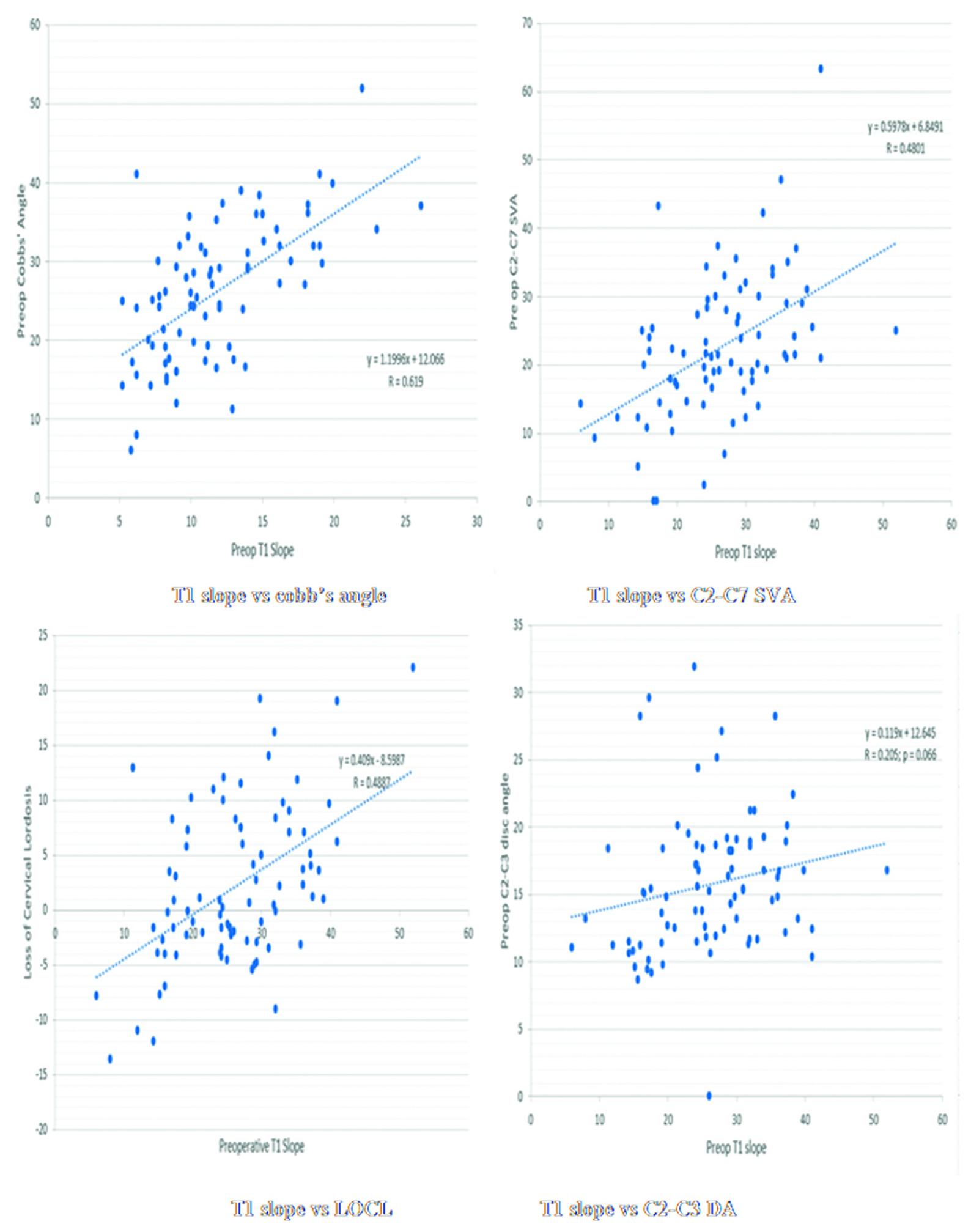
Correlation of preoperative T1S with other radiological parameters
Using Pearson’s correlation, the preoperative T1 slope was found to be significantly correlated with the preoperative C2-C7 Cobb’s angle (R = 0.619, P = 0.001), LOCL (R = 0.487, P = 0.001), and preoperative C2-C7 SVA (R = 0.480, P = 0.001) [
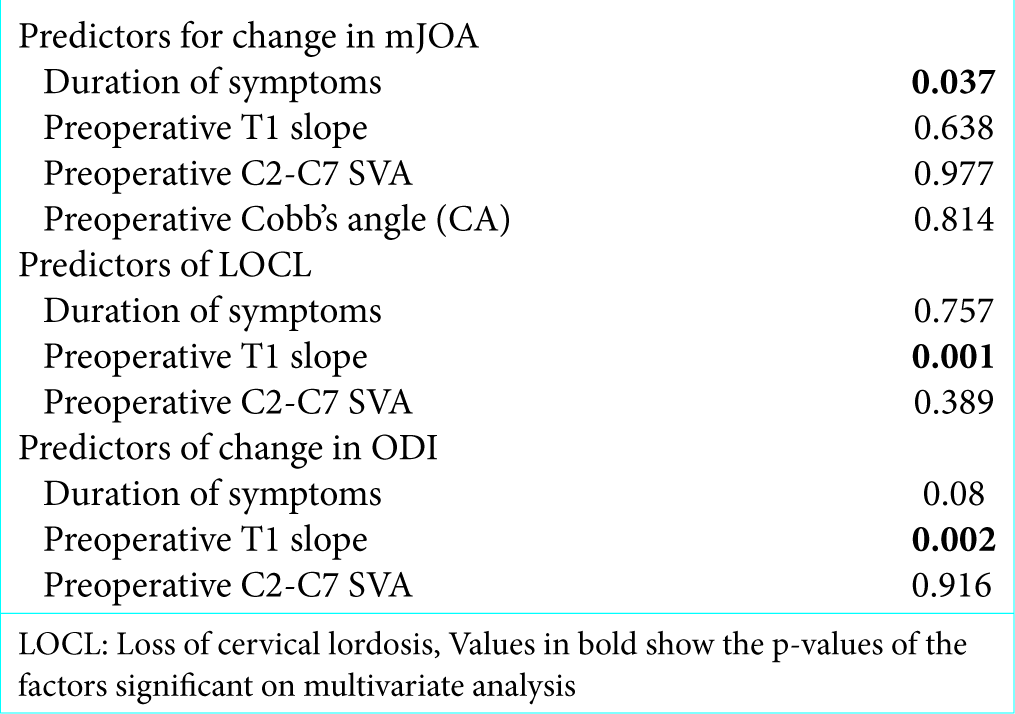
Clinicoradiological outcome predictors of change in mJOA score, ODI index, and LOCL
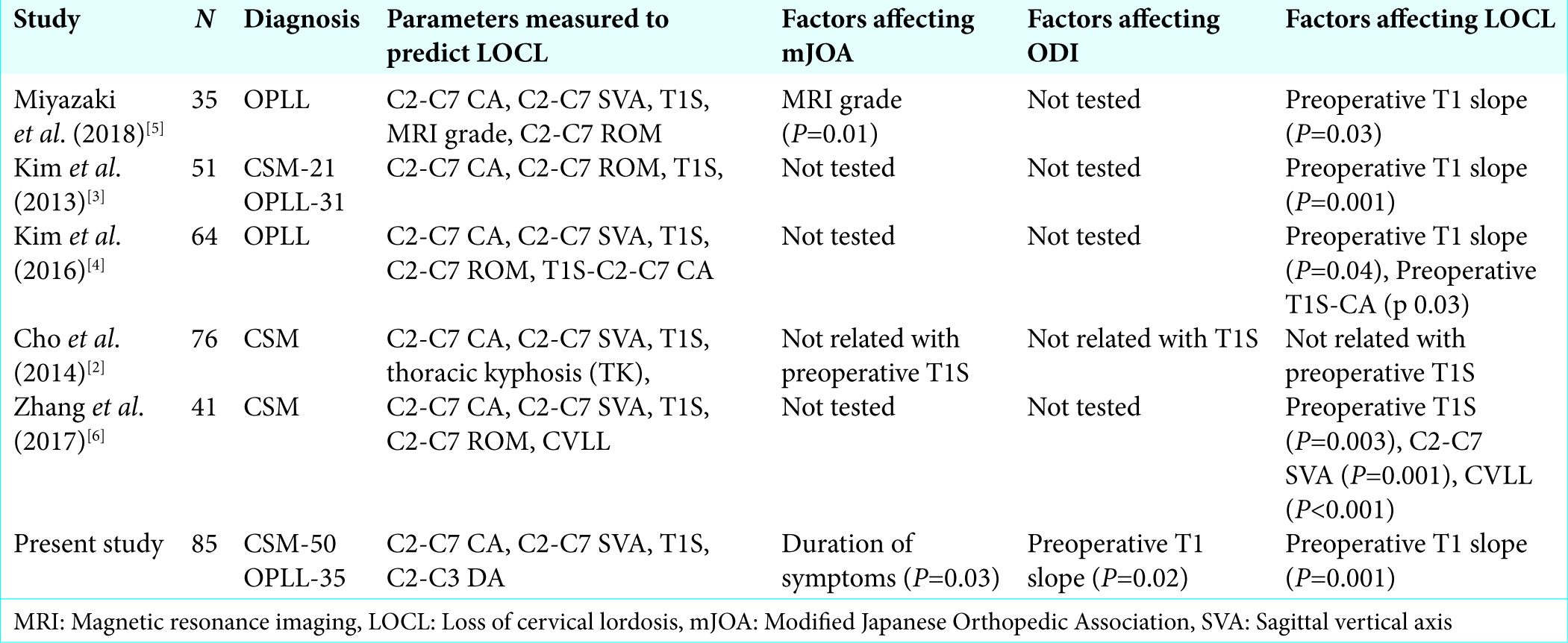
Generalized linear model and multivariate analysis helped determine the preoperative predictors of change in mJOA, ODI, and LOCL [
DISCUSSION
In recent literature, T1 slope emerged as an important predictor for LOCL following laminoplasty.[
We have attempted to create a statistical cutoff value of the preoperative T1 slope (29.5°) that can help predict LOCL following laminoplasty and a relationship between the preoperative T1 slope and change in ODI following laminoplasty [
CONCLUSION
The preoperative T1 slope is a significant predictor for the postoperative LOCL and change in ODI following laminoplasty for patients with CSM/OPLL. If the preoperative T1 slope is greater than 29°, it is a significant predictor for postoperative LOCL following laminoplasty.
References
1. Cao J, Zhang J, Yang D, Yang L, Shen Y. Multivariate analysis of factors associated with kyphotic deformity after laminoplasty in cervical spondylotic myelopathy patients without preoperative kyphotic alignment. Sci Rep. 2017. 7: 43443-
2. Cho JH, Ha JK, Kim DG, Song KY, Kim YT, Hwang CJ. Does preoperative T1 slope affect radiological and functional outcomes after cervical laminoplasty?. Spine (Phila Pa 1976). 2014. 39: E1575-81
3. Kim TH, Lee SY, Kim YC, Park MS, Kim SW. T1 slope as a predictor of kyphotic alignment change after laminoplasty in patients with cervical myelopathy. Spine (Phila Pa 1976). 2013. 38: E992-7
4. Kim B, Yoon DH, Ha Y, Yi S, Shin DA, Lee CK. Relationship between T1 slope and loss of lordosis after laminoplasty in patients with cervical ossification of the posterior longitudinal ligament. Spine J. 2016. 16: 219-25
5. Miyazaki M, Ishihara T, Notani N, Kanezaki S, Tsumura H. Relationship of T1 slope with loss of lordosis and surgical outcomes after laminoplasty for cervical ossification of the posterior longitudinal ligament. Clin Neurol Neurosurg. 2018. 164: 19-24
6. Zhang JT, Li JQ, Niu RJ, Liu Z, Tong T, Shen Y. Predictors of cervical lordosis loss after laminoplasty in patients with cervical spondylotic myelopathy. Eur Spine J. 2017. 26: 1205-10