- Clinical Professor of Neurosurgery, School of Medicine, State University of NY at Stony Brook, and Editor-in-Chief Surgical Neurology International NY and ℅ Dr. Marc Agulnick 1122 Frankllin Avenue Suite 106, Garden City, NY 11530, USA,
- Assistant Clinical Professor of Orthopedics, NYU Langone Hospital, Long Island, NY, USA. 1122 Franklin Avenue Suite 106 Garden City, NY 11530.
Correspondence Address:
Nancy E. Epstein, M.D., F.A.C.S, Clinical Professor of Neurosurgery, School of Medicine, State University of NY at Stony Brook, and Editor-in-Chief Surgical Neurology International NY and ℅ Dr. Marc Agulnick 1122 Frankllin Avenue Suite 106, Garden City, NY 11530, USA.
DOI:10.25259/SNI_1028_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein1, Marc A. Agulnick2. Cervical disc arthroplasty (CDA)/total disc replacement (TDR) vs. anterior cervical diskectomy/fusion (ACDF): A review. 02-Dec-2022;13:565
How to cite this URL: Nancy E. Epstein1, Marc A. Agulnick2. Cervical disc arthroplasty (CDA)/total disc replacement (TDR) vs. anterior cervical diskectomy/fusion (ACDF): A review. 02-Dec-2022;13:565. Available from: https://surgicalneurologyint.com/surgicalint-articles/12036/
Abstract
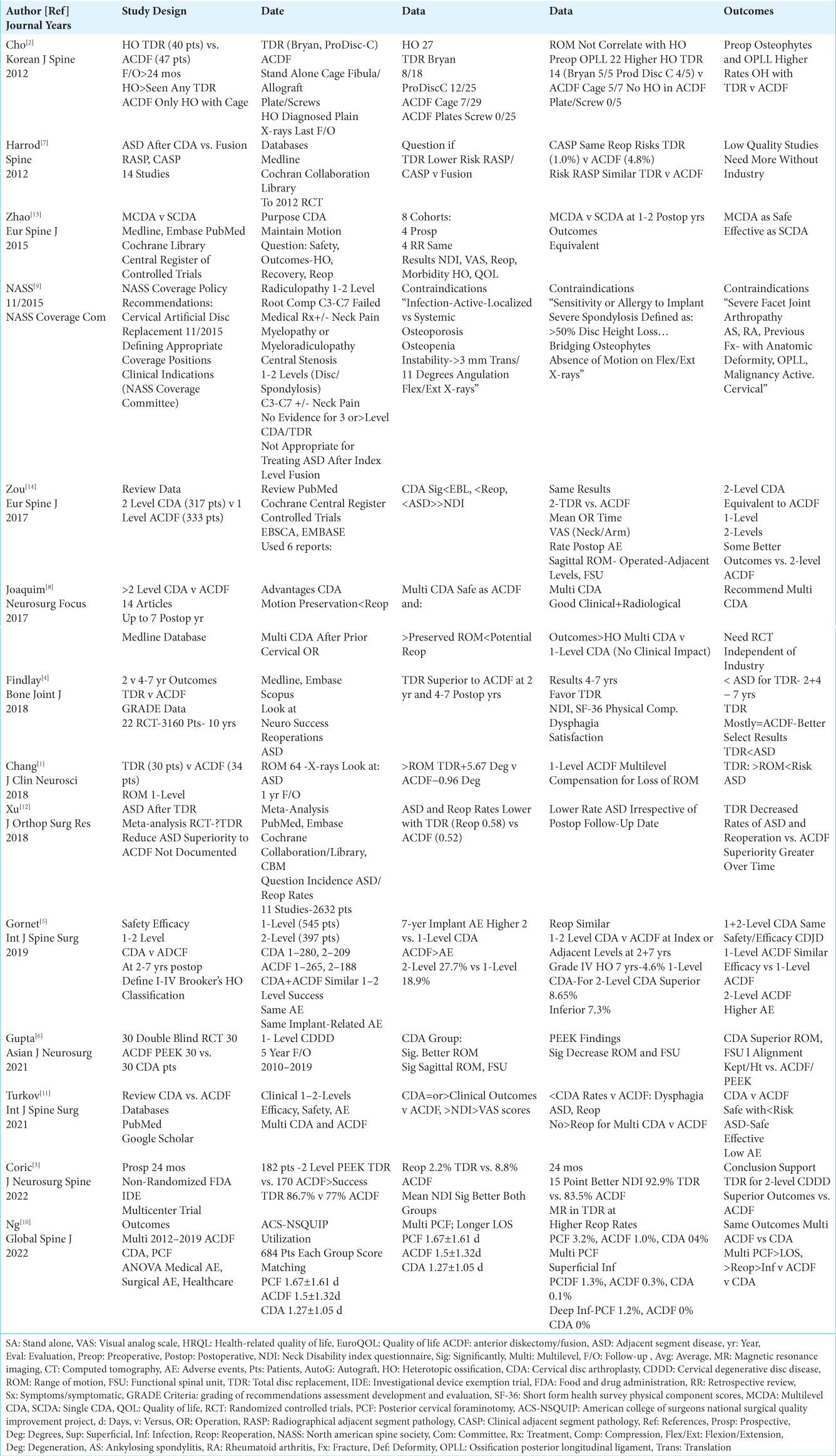
Background: We performed a focused review to determine the “non-inferiority”, potential superiority, and relative safety/efficacy for performing cervical disc arthroplasty (CDA)/total disc replacement (TDR) in carefully selected patients vs. anterior cervical diskectomy/fusion (ACDF). Notably, CDA/TDR were devised to preserve adjacent level range of motion (ROM), reduce the incidence of adjacent segment degeneration (ASD), and the need for secondary ASD surgery.
Methods: We compared the incidence of ASD, reoperations for ASD, safety/efficacy, and outcomes for cervical CDA/TDR vs. ACDF. Indications, based upon the North American Spine Society (NASS) Coverage Policy Recommendations (Cervical Artificial Disc Replacement Revised 11/2015 and other studies) included the presence of radiculopathy or myelopathy/myeloradiculopathy at 1-2 levels between C3-C7 with/without neck pain. Contraindications for CDA/TDR procedures as quoted from the NASS Recommendations (i.e. cited above) included the presence of; “Infection…”, “Osteoporosis and Osteopenia”, “Instability…”, “Sensitivity or Allergy to Implant Materials”, “Severe Spondylosis…”, “Severe Facet Joint Arthropathy…”, “Ankylosing Spondylitis” (AS), “Rheumatoid Arthritis (RA), Previous Fracture…”, “Ossification of the Posterior Longitudinal Ligament (OPLL)”, and “Malignancy…”. Other sources also included spinal stenosis and scoliosis.
Results: Cervical CDA/TDR studies in the appropriately selected patient population showed no inferiority/ occasionally superiority, reduced the incidence of ASD/need for secondary ASD surgery, and demonstrated comparable safety/efficacy vs. ACDF.
Conclusion: Cervical CDA/TDR studies performed in appropriately selected patients showed a “lack of inferiority”, occasional superiority, a reduction in the incidence of ASD, and ASD reoperation rates, plus comparable safety/efficacy vs. ACDF.
Keywords: Adjacent segment disease, Adverse events, Anterior cervical diskectomy/fusion (ACDF), Cervical disc arthroplasty (CDA), Cervical surgery, Comparison, Outcomes, Safety/Efficacy, Secondary surgery/reoperations, Total disc replacement (TDR)
INTRODUCTION
Cervical disc arthroplasty (CDA)/total disc replacement (TDR) were primarily devised to preserve range of motion (ROM) and, thus, lower the incidence of adjacent segment degeneration (ASD), and the requirement for secondary ASD surgery [
Multiple Direct Indications and Contraindications to Performing Cervical CDA/TDR
The indications for performing cervical CDA/TDR taken from the North American Spine Society (NASS) Coverage Policy Recommendations: Artificial Cervical Disc Replacement (i.e. revised 11/2015) included; “Radiculopathy related to nerve root compression from 1-2 level degenerative disease (either herniated disc or spondylotic osteophyte) from C3-C4 to C6-C7 refractory to…non-operative management”, or “Myelopathy or myeloradiculopathy related to central spinal stenosis from 1-2 level degenerative disease (either herniated disc or spondylotic osteophyte) from C3-C4- C6-C7 with or without neck pain” [
Postoperative Dynamic X-rays Confirm Increased Postoperative ROM Following CDA/TDR v ACDF
Several studies documented an increased ROM following CDA/TDR vs. ACDF [
Improvement in Different Variables But Often Comparable Postoperative Outcomes for Single or Multilevel CDA/TDR v ACDF
Various studies showed differences in critical variables (i.e. ASD, reoperation rates for ASD), but comparable outcomes for cervical single or multilevel CDA/TDR vs. 1 level ACDF [
Several Studies Documented Superiority of Postoperative Variables, Including Outcomes, Along with Reduced Dysphagia Rates for Cervical CDA/TDR vs. ACDF
Several studies documented select superior postoperative variables and outcomes along with reduced dysphagia rates following CDA/TDR vs. ACDF [
Comparable Safety/Efficacy of Multilevel Cervical CDA (MCDA)/TDR vs. Single-Level CDA (SCDA)/TDR
At 1 and 2 postoperative years, Zhao et al. (2015) concluded that single (SCDA) vs. multilevel (MCDA) procedures were equally safe/effective with relatively comparable preservation of ROM, reoperation rates, and outcomes [
Comparison of Multiple Variables Including Outcomes for Posterior Cervical Foraminotomy (PCF) vs. CDA/TDR vs. ACDF (ACS-NSQUIP Study)
In a NSQUIP study (ACS-NSQUIP study (American College of Surgeons National Surgical Quality Improvement Project) from 2012-2019, Ng et al. (2022) looked at multiple variables including outcomes for 684 patients undergoing PCF vs. CDSA (684 patients) vs. ACDF (684 patients) [
Definition and Higher Incidence of Heterotopic Ossification (HO) for Cervical CDA/TDR and ACDF Using Stand Alone Cages vs. None for ACDF Performed with Allograft/Screws/Plates but None with Clinical Impact
Definition of HO
Spinal heterotopic ossification (HO) is typically defined by ossification/calcification occurring within the ligaments/soft tissues of the spine. If HO occurs at the index level following cervical surgery utilizing CDA/TDR devices, it can both limit/eliminate the motion-sparing design of these implants, and potentially contribute to recurrent and/or clinically significant spinal cord/nerve root compression. Gornet referenced the Brooker Classification (I-IV) for HO typically applied to total hip arthroplasties (THA) (i.e. I-islands of bone within soft tissues, II->1 cm between bone spurs, III- <1 cm between bone spurs, IV-bony fusion between spurs) [
Different Rates but No Clinical Impact of HO for Cervical CDA/TDR vs. ACDF with Stand Alone Cages
Although several studies documented a higher incidence of HO for cervical CDA/TDR vs. ACDF with stand-alone cages vs. a 0% incidence for ACDF employing allograft/screws/plates, they typically observed that HO did not negatively impact outcomes for any surgical group [
CONCLUSION
Although some studies showed the select superiority for specific variables concerning CDA/TDR (i.e. preservation of ROM, reductions in ASD, lower ASD reoperation rates, and postoperative dysphagia), most concluded CDA/TDR exhibited comparable overall outcomes to ACDF [
Declaration of patient consent
No patients involved in the study other than those discussed in the literature.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
Commentary
Cervical Disc Arthroplasty (CDA) vs Anterior Cervical Discectomy and Fusion (ACDF)
Multiple non-inferiority studies have shown that CDA maintains range of motion and potentially may decrease adjacent segment disease (ASD). But the fact that the surgery is done for radiculopathy in a degenerative condition makes it difficult to measure the true effect on adjacent segment degeneration. Since multiple CDA’s are now approved for 2 level implantation and many are used off-label, it complicates the picture even more. Should some of the earlier CDA’s have had 2 level implants initially but were restricted due to the early FDA indications? The use of finite element models can help us better understand the biomechanics behind ACDF and CDA, and the effects of different biomaterials and CDA designs. With more 2 level CDA implants being performed, time will tell if CDA’s are actually making a significant impact on ASD. However, current data is not conclusive. As we increase the index level range of motion with CDA, we shift the increased stress posteriorly to increase the index level facet forces, and simultaneously decrease the cephalad and caudal adjacent level intradiscal pressures. This tradeoff of increased facet forces may potentially be a source of chronic neck pain or persistent neck pain despite a clinically improved radiculopathy postoperatively.
The issue of heterotopic ossification is frequently overlooked and not documented as the overall spinal range of motion is maintained with CDA’s and spinal segmental motion coupling. Heterotopic ossification occurs in other disease processes (SCI) and with other types of prosthetic joints (hips and elbows etc.). Since the early CDA implants, the perioperative technique has been modified and more surgeons are using NSAIDS postoperatively to try to minimize early HO formation. Many of the CDA studies are not followed long enough, or fail to document HO formation.
As the biomaterials that make up the CDA’s are varied and CDA designs change over time with increasing amounts of translation capabilities added, it will be interesting to see if the CDA will become too mobile, and will anterior migration and anterior osteolysis increase with the newer designs?
Jamie Baisden MD
Professor of Neurosurgery
Medical College of Wisconsin
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Chang SW, Bohl MA, Kelly BP, Wade C. The segmental distribution of cervical range of motion: A comparison of ACDF versus TDR-C. J Clin Neurosci. 2018. 57: 185-93
2. Cho HJ, Shin MH, Huh JW, Ryu KS, Park CK. Heterotopic ossification following cervical total disc replacement: Iatrogenic or constitutional?. Korean J Spine. 2012. 9: 209-14
3. Coric D, Guyer RD, Bae H, Nunley PD, Strenge KB, Peloza JH. Prospective, multicenter study of 2-level cervical arthroplasty with a PEEK-on-ceramic artificial disc. J Neurosurg Spine. Apri 1, 2022. p. 1-11
4. Findlay C, Ayis S, Demetriades AK. Total disc replacement versus anterior cervical discectomy and fusion: A systematic review with meta-analysis of data from a total of 3160 patients across 14 randomized controlled trials with both short-and medium-to long-term outcomes. Bone Joint J. 2018. 100B: 991-1001
5. Gornet MF, Lanman TH, Burkus JK, Hodges SD, McConnell JR, Dryer RF. One-level versus 2-level treatment with cervical disc arthroplasty or fusion: Outcomes up to 7 years. Int J Spine Surg. 2019. 13: 551-60
6. Gupta VK, Basantani N, Carvalho AS, Gupta E. Long-term clinicoradiological outcomes of cervical fusion with polyether ether ketone versus cervical disc arthroplasty in a double-blinded randomized control trial. Asian J Neurosurg. 2021. 16: 725-31
7. Harrod CC, Hilibrand AS, Fischer DJ, Skelly AC. Adjacent segment pathology following cervical motion-sparing procedures or devices compared with fusion surgery: A systematic review. Spine (Phila Pa 1976). 2012. 37: S96-112
8. Joaquim AF, Riew KD. Multilevel cervical arthroplasty: Current evidence. A systematic review. Neurosurg Focus. 2017. 42: E4
9. NASS coverage Policy Recommendations: Cervical Artificial Disc Replacement; Defining Appropriate Coverage Positions. Available from: NASS (www.spine.org) under Cervical Artifical Disc Replacement [Last accessed on 2022 Nov 09].
10. Ng MK, Kobryn A, Baidya J, Nian P, Emara AK, Ahn NU. Multi-level posterior cervical foraminotomy associated with increased post-operative infection rates and overall re-operation relative to anterior cervical discectomy with fusion or cervical disc arthroplasty. Global Spine J. Sep 2, 2022. p. 21925682221124530
11. Turkov D, Job A, Iturriaga C, Verma RB. Current concepts of cervical disc arthroplasty. Int J Spine Surg. 2021. 15: 1174-83
12. Xu S, Liang Y, Zhu Z, Qian Y, Liu H. Adjacent segment degeneration or disease after cervical total disc replacement: A meta-analysis of randomized controlled trials. J Orthop Surg Res. 2018. 13: 244
13. Zhao H, Cheng L, Hou Y, Liu Y, Liu B, Mundra JJ. Multi-level cervical disc arthroplasty (CDA) versus single-level CDA for the treatment of cervical disc diseases: A meta-analysis. Eur Spine J. 2015. 24: 101-12
14. Zou S, Gao J, Zu B, Lu X, Han Y, Meng H. Anterior cervical discectomy and fusion (ACDF) versus cervical disc arthroplasty (CDA) for two contiguous levels cervical disc degenerative disease: A meta-analysis of randomized controlled trials. Eur Spine J. 2017. 26: 985-97