- Division of Neurosurgery, Department of Surgery, Ministry of the National Guard - Health Affairs, Riyadh, Saudi Arabia.
- King Abdullah International Medical Research Center, Riyadh, Saudi Arabia.
- King Saud Bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia.
- Department of Pathology and Laboratory Medicine, King Abdulaziz Medical City, Ministry of the National Guard - Health Affairs, Riyadh, Saudi Arabia.
Correspondence Address:
Sami Khairy
Division of Neurosurgery, Department of Surgery, Ministry of the National Guard - Health Affairs, Riyadh, Saudi Arabia.
King Abdullah International Medical Research Center, Riyadh, Saudi Arabia.
King Saud Bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia.
DOI:10.25259/SNI_174_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sami Khairy, N. A. Alharbi, Abeer Alaglan, Fahd Al Sufiani, Ahmed Alkhani. Cervical epidural neurosarcoidosis: A case report and literature review. 30-May-2020;11:133
How to cite this URL: Sami Khairy, N. A. Alharbi, Abeer Alaglan, Fahd Al Sufiani, Ahmed Alkhani. Cervical epidural neurosarcoidosis: A case report and literature review. 30-May-2020;11:133. Available from: https://surgicalneurologyint.com/surgicalint-articles/10060/
Abstract
Background: Neurosarcoidosis is a rare disease. In the spine, it commonly presents as an intramedullary lesion. Epidural spinal lesions are extremely rare.
Case Description: A 29-year-old patient presented with a 22-month history of progressive neck, upper limb pain, and myelopathy. The cervical MRI showed a large epidural mass infiltrating the paraspinal soft tissue. After an open biopsy, the diagnosis of neurosarcoidosis was established and was followed-up by appropriate medical management.
Conclusion: To manage cervical epidural neurosarcoidosis, first, you must obtain a tissue diagnosis and then follow with appropriate medical management.
Keywords: Cervical, Epidural, Neurosarcoidosis
INTRODUCTION
Sarcoidosis is a multisystem disease attributed to an accelerated immune response of unknown etiology.[
Here, we present a 29-year-old female with left-sided C2–C7 epidural cervical neurosarcoidosis diagnosed utilizing an open biopsy, followed by appropriate medical management.
CASE REPORT
A 29-year-old female presented with a 22-month history of progressive dysphagia, neck pain, and cervical myelopathy. Although she had no motor deficit, she exhibited impaired pin appreciation on the left side from C2–C7, bilateral Hoffman’s signs, and diffuse upper and lower extremity hyperreflexia.
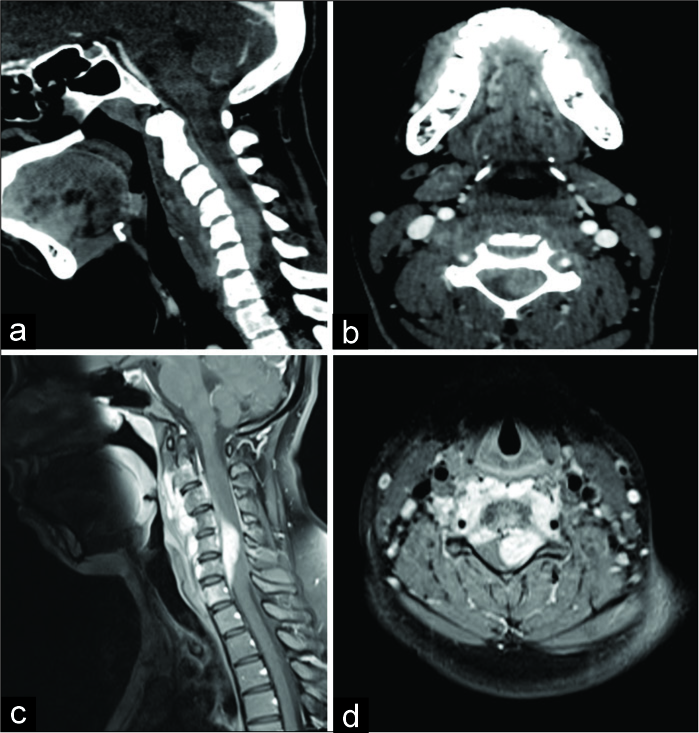
The computed tomography (CT) and full neuraxis enhanced MR studies showed a left-sided epidural enhanced mass from C2 to C7 compressing the spinal cord and displacing it to the right with a paravertebral extension [
Figure 1:
Cervical CT with contrast (a: sagittal and b: axial) and MRI (c: sagittal and d: axial) shows a longitudinally oriented epidural enhancing soft-tissue mass lesion occupying the left side of the spinal canal opposite C2 down to the C7 vertebra. MRI (c: sagittal and d: axial) shows intraspinal epidural and paraspinal avidly enhancing cervical lesions with multiple neural foraminal extensions and cord compression, which was most severe at C5.
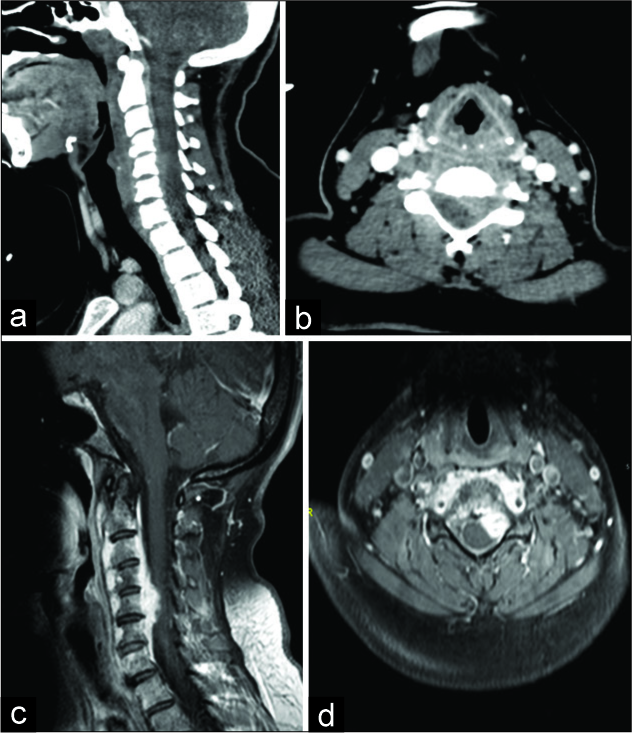
Three days after the presentation, a CT-guided biopsy was performed. However, due to the initiation of steroids (dexamethasone 4 mg every 6 h), the tumor had significantly decreased in size (e.g., repeat MRI showed that the lesion had profoundly regressed), and a biopsy was no longer feasible/ reliable [
Figure 2:
Contrasted cervical CT (a: sagittal and b: axial) during the CT-guided biopsy, preprocedure scan demonstrated improvement of the prevertebral tissue, likely related to steroids treatment. Due to the lack of enough safety margin to perform biopsy, the procedure was cancelled. Repeated cervical MRI (c: sagittal and d: axial), showed the lesion response to the steroids more profoundly.
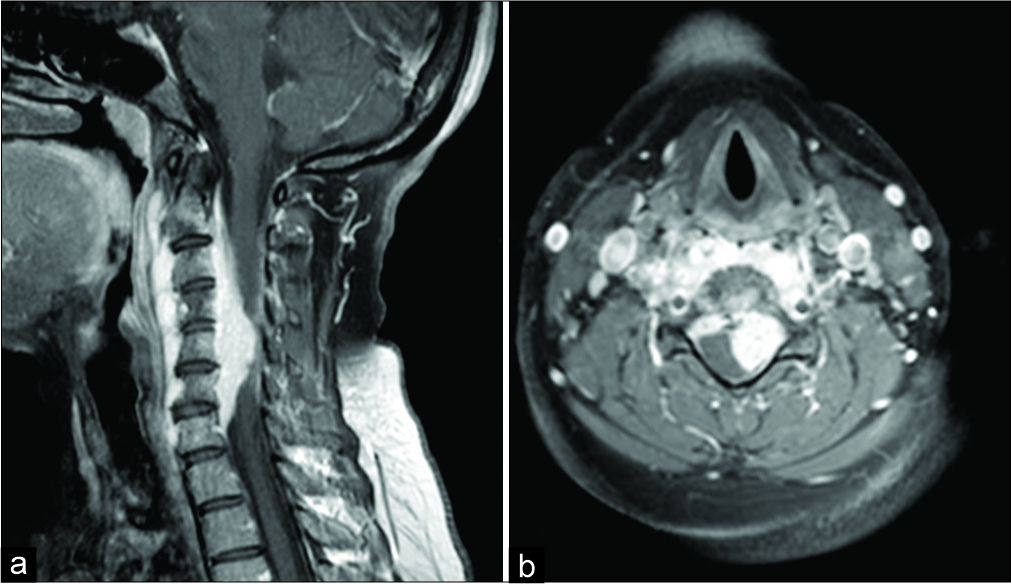
The next MR performed 2 weeks after cessation of steroids revealed significant tumor recurrence [
DISCUSSION
Sarcoidosis is a chronic systemic inflammatory disease characterized by noncaseating granulomas on pathological examination. It most commonly affects the lungs and mediastinal lymph nodes.[
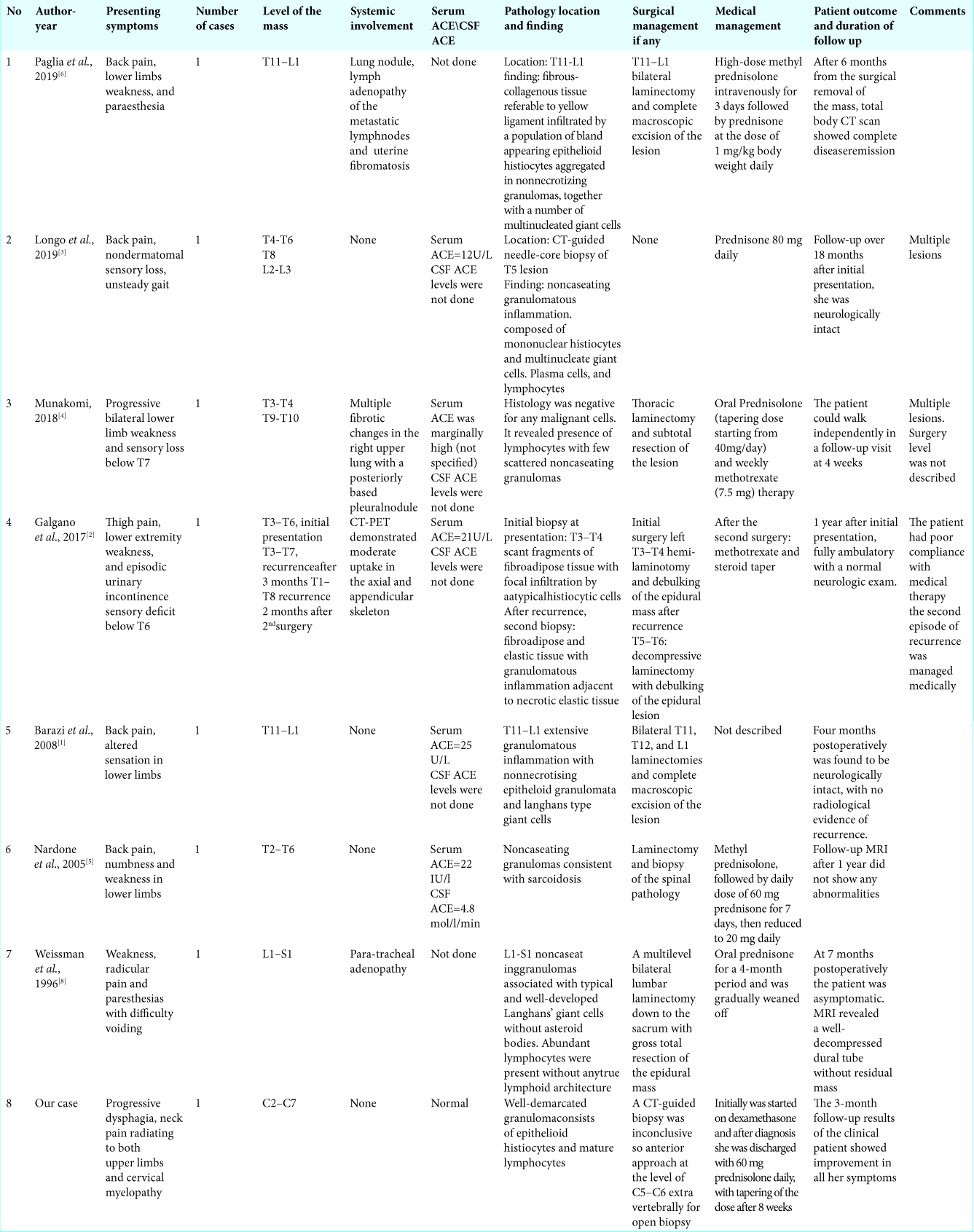
Just 10% of neurosarcoidosis involve the spine. Seven similar cases found in the literature. Of interest, most are intramedullary lesions, and few involve the extradural compartment [
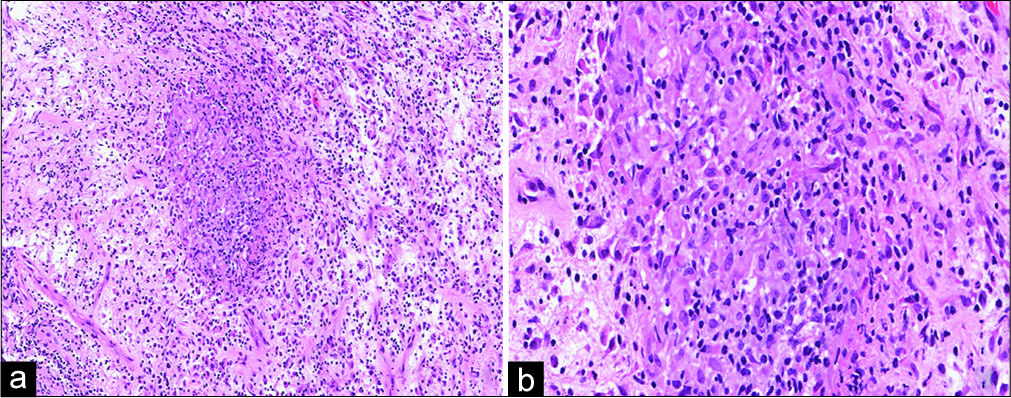
Most cases of neurosarcoidosis have normal levels of ACE, and the histology demonstrates nonnecrotizing granulomas with an inflammatory background [
Although medical management is the standard of care for neurosarcoidosis, most patients initially undergo biopsy surgical decompression or debulking to obtain pathology [
CONCLUSION
Epidural spinal neurosarcoidosis is very rare. Establishing a pathological diagnosis warrants cessation of steroids (i.e., if previously administered), and the performance of a biopsy or open surgical debulking. Once pathology has been established, these lesions can be typically managed with short-long-term steroids and/or other medical regimens.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Barazi S, Bodi I, Thomas N. Sarcoidosis presenting as an isolated extradural thoracolumbar lesion mimicking tumour. Br J Neurosurg. 2008. 22: 690-1
2. Galgano MA, Goulart CR, Chisholm K, Hazen M, Stone S. Rapid-onset thoracic myelopathy due to an epidural sarcoid-like lesion in a pediatric patient. World Neurosurg. 2018. 111: 377-80
3. Longo M, Gelfand Y, Kinon MD, Pullman J, Yassari R. Multifocal epidural neurosarcoidosis causing spinal cord compression: A case report. Cureus. 2019. 11: e4177-
4. Munakomi S. Case report: Case report on multiple extradural thoracic lesions with myelopathy as the clinical presentation in a systemic sarcoidosis-another tale of a lurking entity. F1000Res. 2018. 7: 6-
5. Nardone R, Venturi A, Buffone E, Lochner P, Marth R, Florio I. Extramedullary spinal neurosarcoidosis: Report of two cases. Eur Neurol. 2006. 54: 220-4
6. Paglia F, D’Angelo L, Armocida D, Sampirisi L, Giangaspero F, De Vincentiis L. A rare case of spinal epidural sarcoidosis: Case report and review of the literature. Acta Neurol Belg. 2019. 11: 1-6
7. Sohn M, Culver DA, Judson MA, Scott TF, Tavee J, Nozaki K. Spinal cord neurosarcoidosis. Am J Med Sci. 2014. 347: 195-8
8. Weissman MN, Lange R, Kelley C, Belgea K, Abel L. Intraspinal epidural sarcoidosis: Case report. Neurosurgery. 1996. 39: 179-81