- Department of Neurosurgery, University of Pittsburgh Medical Center, Pennsylvania, United States.
- Department of Neurosurgery, University of Pittsburgh School of Medicine, Pennsylvania, United States.
- Department of Pathology, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, United States.
Correspondence Address:
Enyinna Nwachuku
Department of Neurosurgery, University of Pittsburgh Medical Center, Pennsylvania, United States.
DOI:10.25259/SNI_87_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Enyinna Nwachuku, James Duehr, Scott Kulich, Daniel Marker, John Moossy. Cervical intramedullary spinal cavernoma in setting of unresolved myelopathy: A case report. 04-Jul-2020;11:176
How to cite this URL: Enyinna Nwachuku, James Duehr, Scott Kulich, Daniel Marker, John Moossy. Cervical intramedullary spinal cavernoma in setting of unresolved myelopathy: A case report. 04-Jul-2020;11:176. Available from: https://surgicalneurologyint.com/surgicalint-articles/10116/
Abstract
Background: Spinal cavernous malformations are rare, accounting for approximately 5–12% of all spinal cord vascular lesions. Fortunately, improvements in imaging technologies have made it easier to establish the diagnosis of intramedullary spinal cavernomas (ISCs).
Case Description: Here, we report the case of a 63-year-old male with an >11-year history of left-sided radiculopathy, ataxia, and quadriparesis. Initially, radiographic findings were interpreted as consistent with spondylotic myelopathy with cord signal changes from the C3-C7 levels. The patient underwent a C3-C7 laminectomy/foraminotomy with instrumentation. It was only after several symptomatic recurrences and repeated magnetic resonance images (MRI) that the diagnosis of a ventrally-located intramedullary lesion, concerning for a cavernoma, at the level C6 was established.
Conclusion: Early and repeated enhanced MR studies may be required to correctly establish the diagnosis and determine the optimal surgical management of ISCs.
Keywords: Cervical spine, Complex surgery, Diagnosis, Excision, Intramedullary spinal cavernoma, Laminectomy, Magnetic resonance, Myelotomy
INTRODUCTION
Spinal cord cavernous malformations (cavernomas) are rare vascular malformations (e.g., 5–12% of all such lesions).[
Here, we present a 63-year-old male with an ISC documented on magnetic resonance (MR) at the C6 level. Despite an original C3-C6 laminectomy/decompression with C3-C7 fusion, the patient rebled requiring repeated intervention.
CASE DESCRIPTION
History: A 63-year-old male presented with an 11-year history of progressive radiculopathy and ataxia involving the left upper and lower extremities, newly accompanied over the past year by a mild quadriparesis and left leg paresthesia.
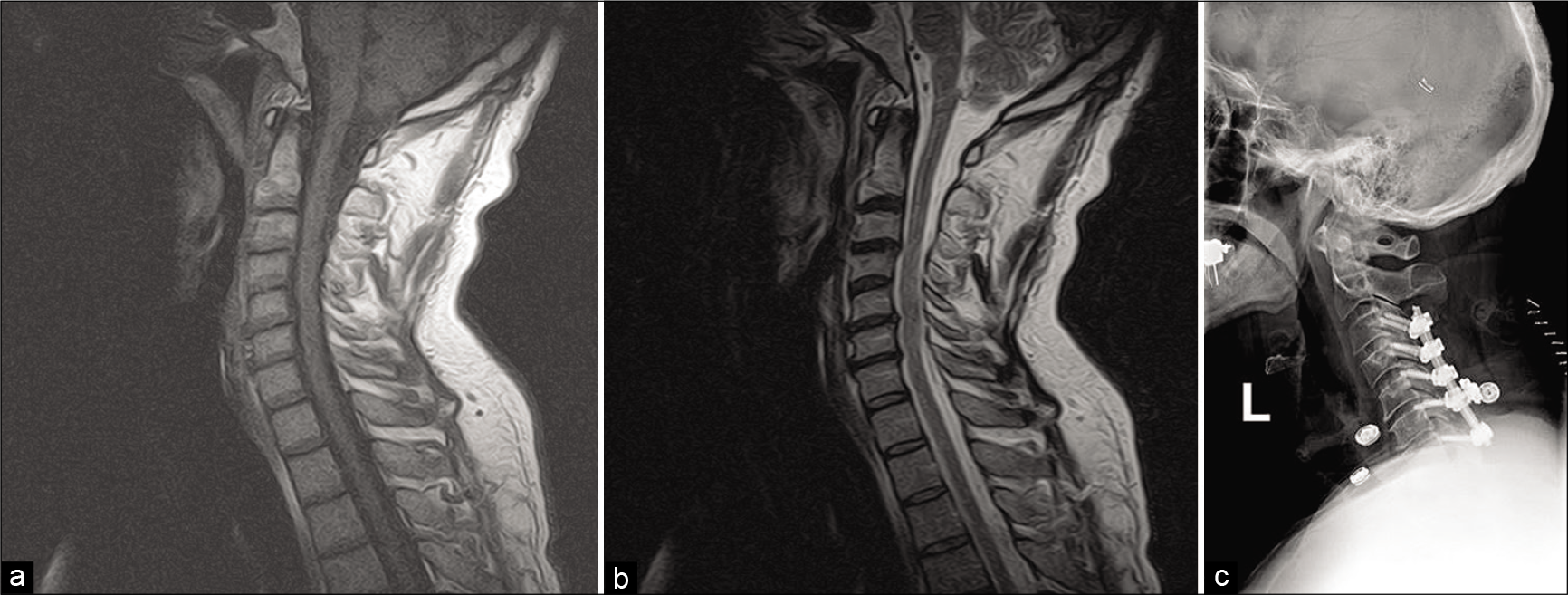
In 2008, MR showed cervical stenosis with C3-C7 spondylotic myelopathy, for which a C3-C7 laminectomy/instrumented fusion was performed [
Figure 1:
Perioperative imaging of the cervical spine fusion performed in 2008. (a) Preoperative T1-weighted magnetic resonance imaging (MRI) of the cervical spine. (b) Preoperative T2-weighted MRI of the cervical spine. No significant foci are noted, but canal stenosis is visible from C3-C6. (c) Postoperative X-ray demonstrated instrumented fusion from C3-C7. “L” denotes that the image taken from the left side of the patient’s body.
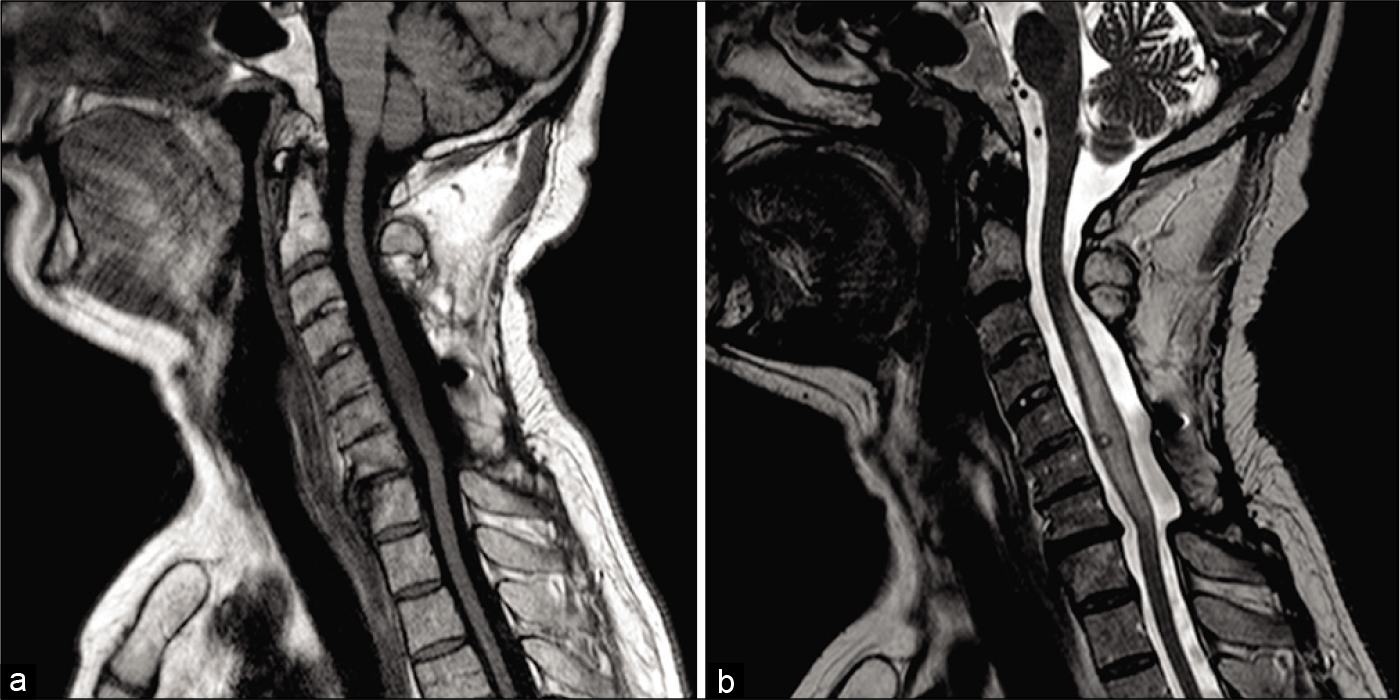
Physical examination: In 2019 (11 years after his original 2008 fusion), he presented with recurrent cervical radiculopathy, a mild quadriparesis, ataxia, and paresthesia in the left lower extremity (the latter over the past year). The follow- up MR documented a small intramedullary nodule ventrally located at the C5-C6 level accompanied by perinodular edema extending throughout the cord; the lesion remained stable on successive MR studies over the ensuring several months [
Figure 2:
Preoperative imaging of the intramedullary spinal cavernoma resection performed in 2019. (a) Preoperative T1-weighted magnetic resonance imaging (MRI) of the cervical spine. (b) Preoperative T2-weighted MRI of the cervical spine. A small but notable signal is visible ventrally at the level of C6 consistent with a focal nodule. A significant signal consistent with peri-nodular edema is also visible from C3-C7.
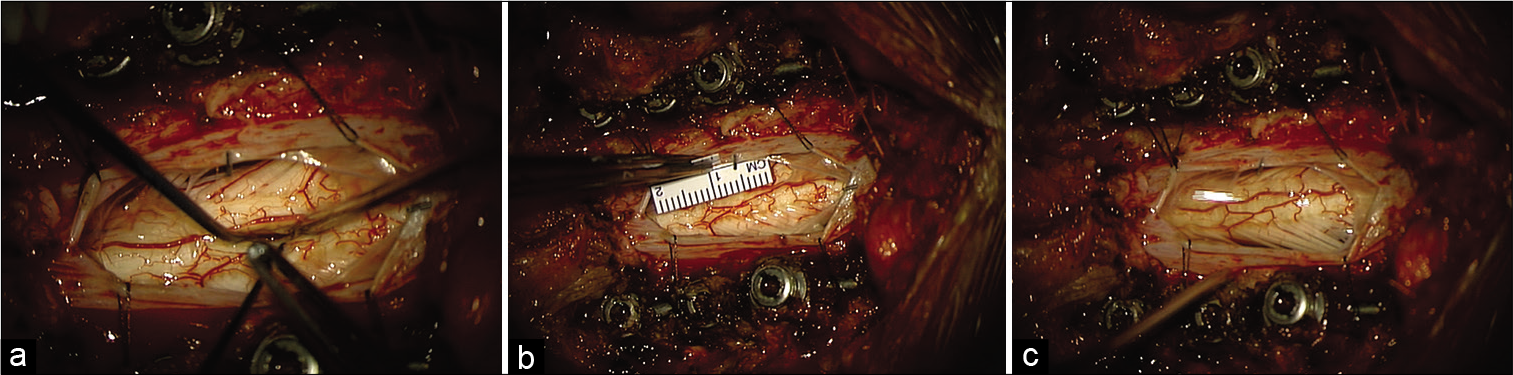
Operative findings: The procedure required the utilization of ultrasound, fluoroscopy, and microsurgical technique to perform a C5-C6 midline myelotomy [
Figure 3:
Intraoperative imaging of myelotomy and dural opening. (a) Color photo of operative field postmyelotomy. The screws depicted in the top and bottom of the photo correspond to instrumentation at C5, C6, and C7 (from cephalad to caudal) (b) Color photo as in a, with added ruler for the measurement. (c) Color photo of operative field postdural opening.
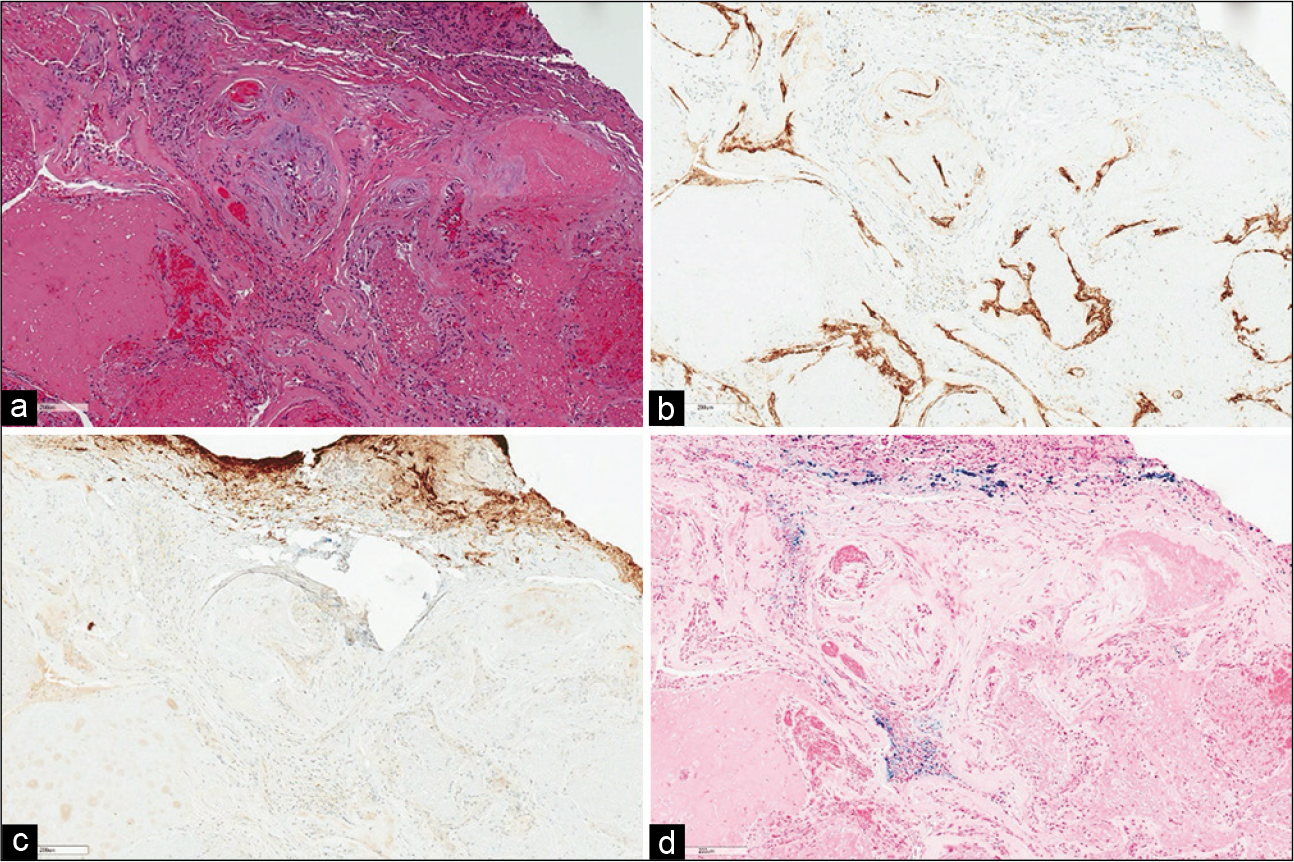
Pathology: Intraoperatively, the frozen section staining demonstrated a collection of thin-walled vessels with focal fibrosis and thrombosis without intervening neural parenchyma, diagnostic for a cavernous angioma [
Figure 4:
Histological examination of cavernous angioma. (a) Hematoxylin and eosin-stained section demonstrating a collection of thin- walled hyalinized vessels surrounded by a thin rim of central nervous system tissue. (b) Immunohistochemical stain for CD34 highlights the vascular endothelium. (c) Immunohistochemical stain for glial fibrillary acidic protein highlights the surrounding reactive astrocytosis in the rim of central nervous system tissue. Of note, there is no appreciable intervening central nervous system tissue between the vessels. (d) Iron stain highlights hemosiderin deposition (blue) indicative of remote hemorrhage. (Magnification ×100; all scale bars equal 200 μm).
Postoperative course: Postoperatively, the patient exhibited a mild paresis in the left L4, L5, and S1 dermatomes (chronic preoperatively), and a new left-sided upper and lower extremity hemisensory deficit without hyperreflexia. The patient was able to ambulate with assistance (i.e., due to proprioception deficits) and was discharged home
DISCUSSION
Here, we described a 63-year-old male with >11-year history of radiculopathy, progressive quadriparesis, and ataxia, with recurrent cervical myelopathy despite two operations. After recurrence, the MR indicated an intramedullary lesion at the C6 level. Following secondary surgical resection with pathological confirmation, the patient sustained significant postoperative sensory deficits but no further hemorrhagic events.[
Review of relevant literature
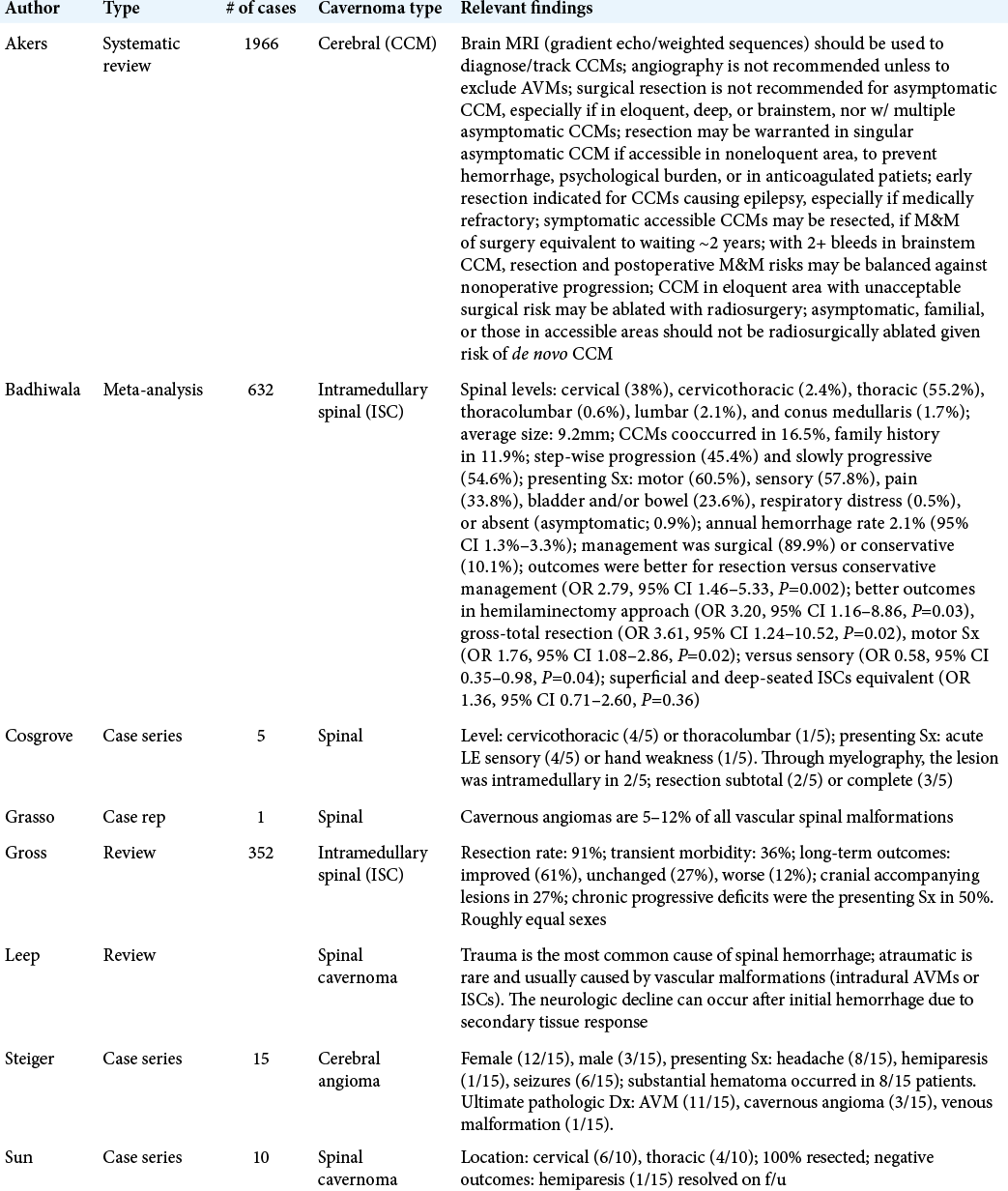
We conducted a review of the literature on intramedullary cavernomas, with a focus on spinal lesions. The preceding case followed a similar course as other chronically untreated ISCs, although, in the other cases, early resection was more common.[
CONCLUSION
As demonstrated in the case presented and following a literature review of ISCs, one must maintain a high index of suspicion for cavernoma, especially when patients exhibit a progressive/stuttering course of neurological deterioration along with repeated intramedullary spinal hemorrhages.
Declaration of patient consent
Patient’s consent not obtained as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Akers A, Al-Shahi Salman R, Awad IA, Dahlem K, Flemming K, Hart B. Synopsis of guidelines for the clinical management of cerebral cavernous malformations: Consensus recommendations based on systematic literature review by the angioma alliance scientific advisory board clinical experts panel. Neurosurgery. 2017. 80: 665-80
2. Badhiwala JH, Farrokhyar F, Alhazzani W, Yarascavitch B, Aref M, Algird A. Surgical outcomes and natural history of intramedullary spinal cord cavernous malformations: A single-center series and meta-analysis of individual patient data: Clinic article. J Neurosurg Spine. 2014. 21: 662-76
3. Cosgrove GR, Bertrand G, Fontaine S, Robitaille Y, Melanson D. Cavernous angiomas of the spinal cord. J Neurosurg. 1988. 68: 31-6
4. Grasso G, Alafaci C, Granata F, Cutugno M, Salpietro FM, Tomasello F. Thoracic spinal cord cavernous angioma: A case report and review of the literature. J Med Case Rep. 2014. 8: 271-
5. Gross BA, Du R, Popp AJ, Day AL. Intramedullary spinal cord cavernous malformations. Neurosurg Focus. 2010. 29: E14-
6. Hunderfund AN, Wijdicks EF. Intramedullary spinal cord hemorrhage (hematomyelia). Rev Neurol Dis. 2009. 6: E54-61
7. Steiger HJ, Tew JM Jr. Hemorrhage and epilepsy in cryptic cerebrovascular malformations. Arch Neurol. 1984. 41: 722-4
8. Sun I, Pamir MN. Spinal cavernomas: Outcome of surgically treated 10 patients. Front Neurol. 2017. 8: 672-