- School of Medicine and Health Sciences, The George Washington University School of Medicine and Health Sciences, Washington, D.C., United States
- Department of Neurosurgery, New York University School of Medicine, Langone Hospital, New York, United States
- Department of Neurosurgery, University at Buffalo, New York, United States
- Department of Neurosurgery, Cairo University, Cairo, Egypt
Correspondence Address:
Jeffrey P. Mullin, Department of Neurosurgery, University at Buffalo, Buffalo, United States.
DOI:10.25259/SNI_299_2025
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hannon W. Levy1, Bennett R. Levy2, Mohamed A.R. Soliman3,4, Esteban Quiceno3, Jacob David Greisman3, Asham Khan3, Juan Bautista Amiotti3, John Pollina3, Jeffrey P. Mullin3. Cervical laminectomy and fusion versus laminoplasty in degenerative cervical myelopathy: A propensity score matching analysis. 06-Jun-2025;16:220
How to cite this URL: Hannon W. Levy1, Bennett R. Levy2, Mohamed A.R. Soliman3,4, Esteban Quiceno3, Jacob David Greisman3, Asham Khan3, Juan Bautista Amiotti3, John Pollina3, Jeffrey P. Mullin3. Cervical laminectomy and fusion versus laminoplasty in degenerative cervical myelopathy: A propensity score matching analysis. 06-Jun-2025;16:220. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13619
Abstract
Background: Degenerative cervical myelopathy (DCM) is a common cause of spinal cord dysfunction. The effectiveness of laminoplasty (LP) versus laminectomy with fusion (LF) for treating DCM is still debated. Here, we compared LP versus LF for treating DCM using propensity score matching (PSM) to minimize selection bias.
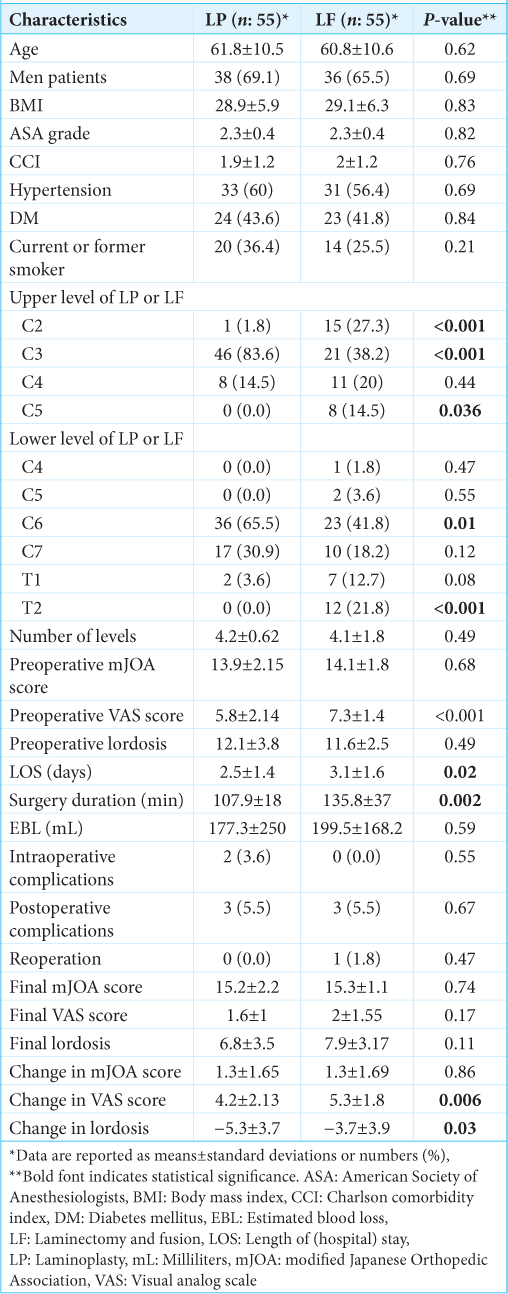
Methods: We identified DCM patients undergoing LP versus LF (2004–2022). Our analysis included demographics, preoperative/postoperative modified Japanese orthopedic association (mJOA) scoring, Visual Analog Scale (VAS) scores, assessment of postoperative cervical lordosis, operative time, blood loss, length of stay (LOS), and adverse events. PSM was performed to create balanced groups and minimize selection bias. Paired t-tests and Chi-square tests were used for statistical analysis.
Results: After PSM, 55 patients in each group were analyzed. LP patients had significantly shorter operative times and LOS, but VAS scores were significantly better for the LF group. Notably, both groups showed similar improvements in mJOA scores, frequency of intraoperative/postoperative adverse events, and reoperation rates. Although changes in cervical lordosis were significantly different between the groups, both groups showed comparable final lordotic curvatures.
Conclusion: LP procedures resulted in significantly shorter operative times and LOS, but VAS scores were correlated with significantly better outcomes in the LF group. Notably, both LP and LF patients demonstrated similar improvement in mJOA scores, frequencies of intraoperative/postoperative adverse events, and reoperation rates.
Keywords: Cervical lordosis, Laminectomy, Laminoplasty, Propensity score matching
INTRODUCTION
Laminoplasty (LP) and laminectomy with fusion (LF) are commonly employed posterior procedures for treating multilevel degenerative cervical myelopathy (DCM).[
MATERIALS AND METHODS
This retrospective cohort study compares open-door LP (55 patients) versus LF (55 patients) for the treatment of DCM. It was approved by the Institutional Review Board (2004–2022). Following 1:1 propensity score matching (PSM) and using multiple inclusion and exclusion criteria, we analyzed multiple clinical and radiological variables to select patients for the LP and LF surgical groups [
PSM and statistical analysis
We utilized PSM to minimize selection bias and confounding variables inherent in retrospective studies. We employed a logistic regression model to estimate the propensity score for each LF versus LP patient by looking at the following variables/covariates: age, body mass index, American Society of Anesthesiologists grade, Charlson comorbidity index, smoking status, hypertension, diabetes mellitus, number of surgical levels, preoperative modified Japanese orthopedic association (mJOA), and preoperative lordosis. Patients in these two groups were then matched 1:1 using a nearest-neighbor matching algorithm with a fuzz factor of 1, resulting in two balanced groups of patients. Differences between the matched groups were assessed using paired t-tests for continuous variables and the Chi-square test for categorical variables. Changes in clinical and radiographic outcomes within each group were assessed using paired t-tests.
RESULTS
The LP group had a significantly shorter mean operative time and their mean length of stay (LOS) was significantly shorter versus the LF group. However, the LF patients demonstrated significantly greater improvement in Visual Analog Scale (VAS) scores versus LP patients and less loss of final lordosis. Notably, no significant differences were found between the two groups regarding estimated blood loss (EBL), number of levels operated on, final mJOA scores, changes in mJOA scores, frequencies of intraoperative/postoperative adverse events, or numbers of reoperations [
DISCUSSION
We compared the safety/efficacy of LP and LF for treating DCM utilizing PSM to minimize the impact of confounding variables. LP was associated with significantly shorter surgical duration and length of hospital stay (LOS) versus LF. Lee et al. voiced similar findings (i.e., they included both randomized and nonrandomized studies, introducing potential selection bias).[
CONCLUSION
This PSM analysis provides compelling evidence for the comparative effectiveness and safety of LP and LF for DCM.
Ethical approval:
The research/study was approved by the Institutional Review Board at University at Buffalo, approval number STUDY00005439 , dated August 6th, 2021.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship:
Nil.
Conflicts of interest:
Asham Khan received a research grant from the Scoliosis Research Society to study scoliosis in Chiari patients. Jeffrey P. Mullin serves as a consultant for SI Bone and Medtronic. John Pollina is involved with surgical training for Medtronic and serves as a consultant for and receives royalties from ATEC spine.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. He X, Zhang JN, Liu TJ, Hao DJ. Is laminectomy and fusion the better choice than laminoplasty for multilevel cervical myelopathy with signal changes on magnetic resonance imaging? A comparison of two posterior surgeries. BMC Musculoskelet Disord. 2020. 21: 423
2. Lau D, Winkler EA, Than KD, Chou D, Mummaneni PV. Laminoplasty versus laminectomy with posterior spinal fusion for multilevel cervical spondylotic myelopathy: Influence of cervical alignment on outcomes. J Neurosurg Spine. 2017. 27: 508-17
3. Lee CH, Lee J, Kang JD, Hyun SJ, Kim KJ, Jahng TA. Laminoplasty versus laminectomy and fusion for multilevel cervical myelopathy: A meta-analysis of clinical and radiological outcomes. J Neurosurg Spine. 2015. 22: 589-95
4. Ma L, Liu FY, Huo LS, Zhao ZQ, Sun XZ, Li F. Comparison of laminoplasty versus laminectomy and fusion in the treatment of multilevel cervical ossification of the posterior longitudinal ligament: A systematic review and meta-analysis. Medicine (Baltimore). 2018. 97: e11542
5. Phan K, Scherman DB, Xu J, Leung V, Virk S, Mobbs RJ. Laminectomy and fusion vs laminoplasty for multi-level cervical myelopathy: A systematic review and meta-analysis. Eur Spine J. 2017. 26: 94-103
6. Yang E, Mummaneni PV, Chou D, Bydon M, Bisson EF, Shaffrey CI. Cervical laminoplasty versus laminectomy and posterior cervical fusion for cervical myelopathy: Propensity-matched analysis of 24-month outcomes from the quality outcomes database. J Neurosurg Spine. 2023. 39: 671-81
7. Yuan X, Wei C, Xu W, Gan X, Cao S, Luo J. Comparison of laminectomy and fusion vs laminoplasty in the treatment of multilevel cervical spondylotic myelopathy: A meta-analysis. Medicine (Baltimore). 2019. 98: e14971
8. Zhao H, Ren R, Ma W, Xu S, Peng L, Zhong Z. Comparison of laminoplasty vs. Laminectomy for cervical spondylotic myelopathy: A systematic review and meta-analysis. Front Surg. 2021. 8: 790593