- Department of Orthopedic Surgery, Akita Red Cross Hospital, Akita, Japan.
- Department of Orthopedic Surgery, Akita University Graduate School of Medicine, Akita, Japan.
- Department of Orthopedic Surgery, Akita Prefectural Center on Development and Disability, Akita, Japan.
Correspondence Address:
Yuichi Ono, Department of Orthopedic Surgery, Akita Red Cross Hospital, Akita, Japan.
DOI:10.25259/SNI_1171_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yuichi Ono1, Michio Hongo2, Yuji Kasukawa2, Akiko Misawa3, Daisuke Kudo2, Naohisa Miyakoshi2. Chronic atlantoaxial rotatory fixation with neurofibromatosis type I: A case report. 11-Feb-2022;13:40
How to cite this URL: Yuichi Ono1, Michio Hongo2, Yuji Kasukawa2, Akiko Misawa3, Daisuke Kudo2, Naohisa Miyakoshi2. Chronic atlantoaxial rotatory fixation with neurofibromatosis type I: A case report. 11-Feb-2022;13:40. Available from: https://surgicalneurologyint.com/surgicalint-articles/11389/
Abstract
Background: Atlantoaxial rotatory fixation (AARF) can be caused by infection, rheumatoid arthritis, surgery of head and neck, and congenital diseases. Type 1 neurofibromatosis (NF-1) is often associated with various musculoskeletal diseases, but few reports have described AARF with NF-1. Here, we report the success of a closed reduction and halo fixation utilized to treat chronic AARF with NF-1 in a 7-year-old female.
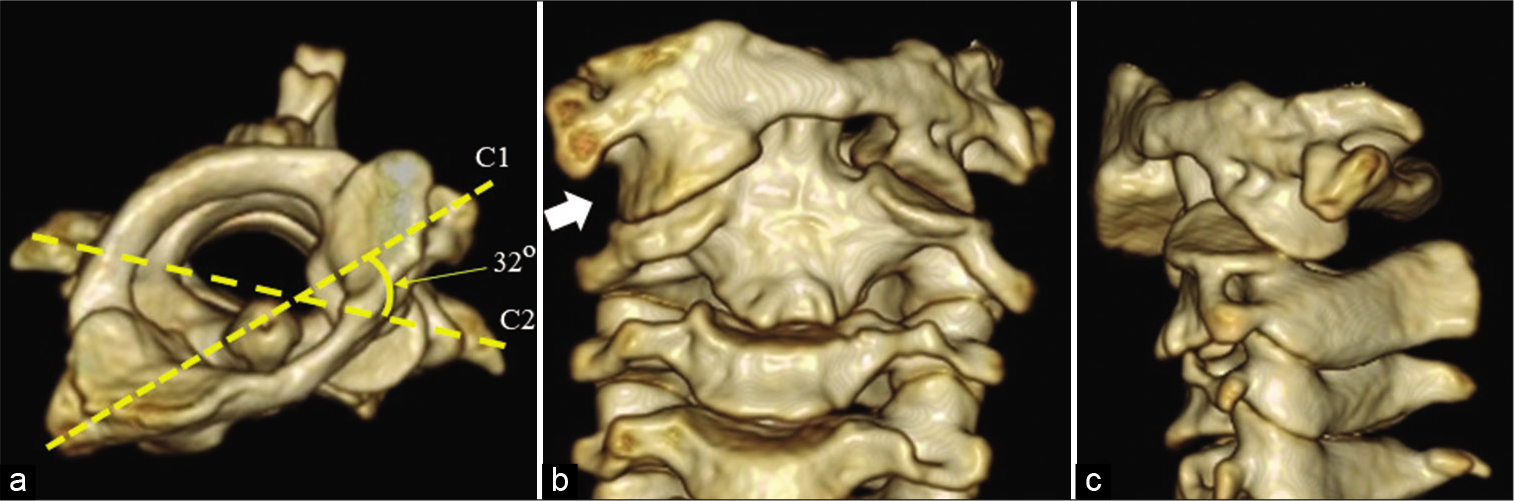
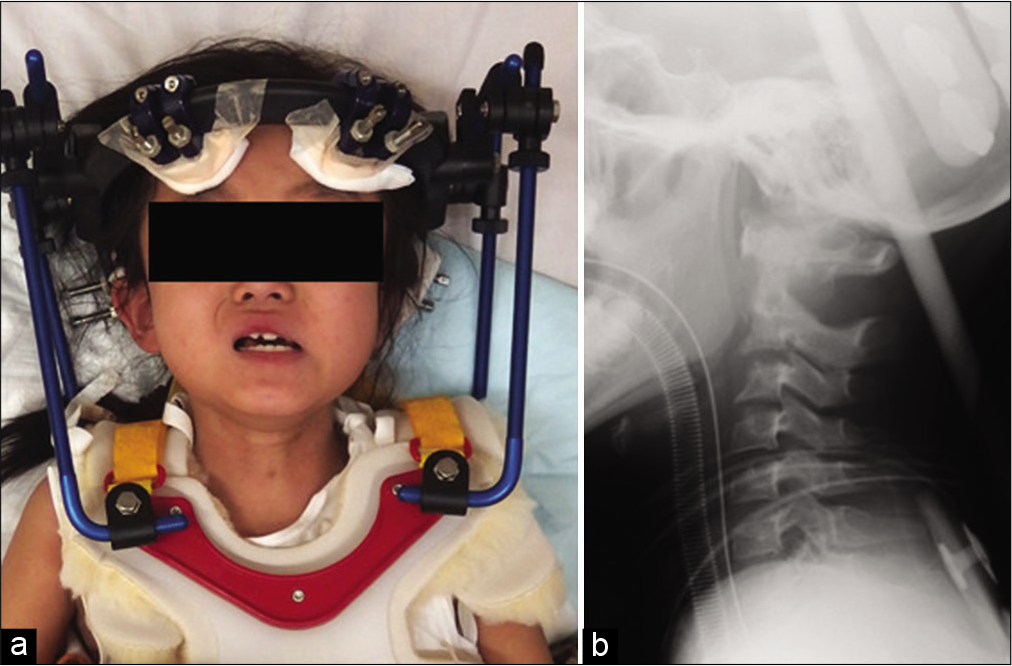
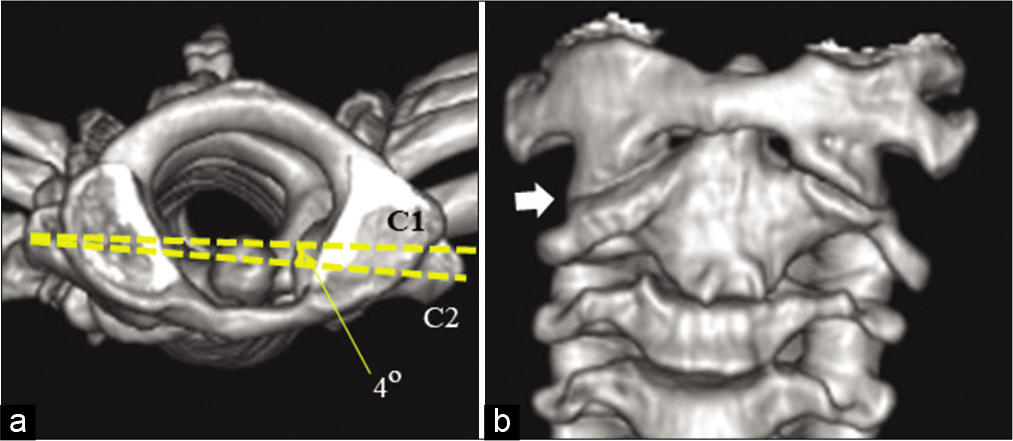
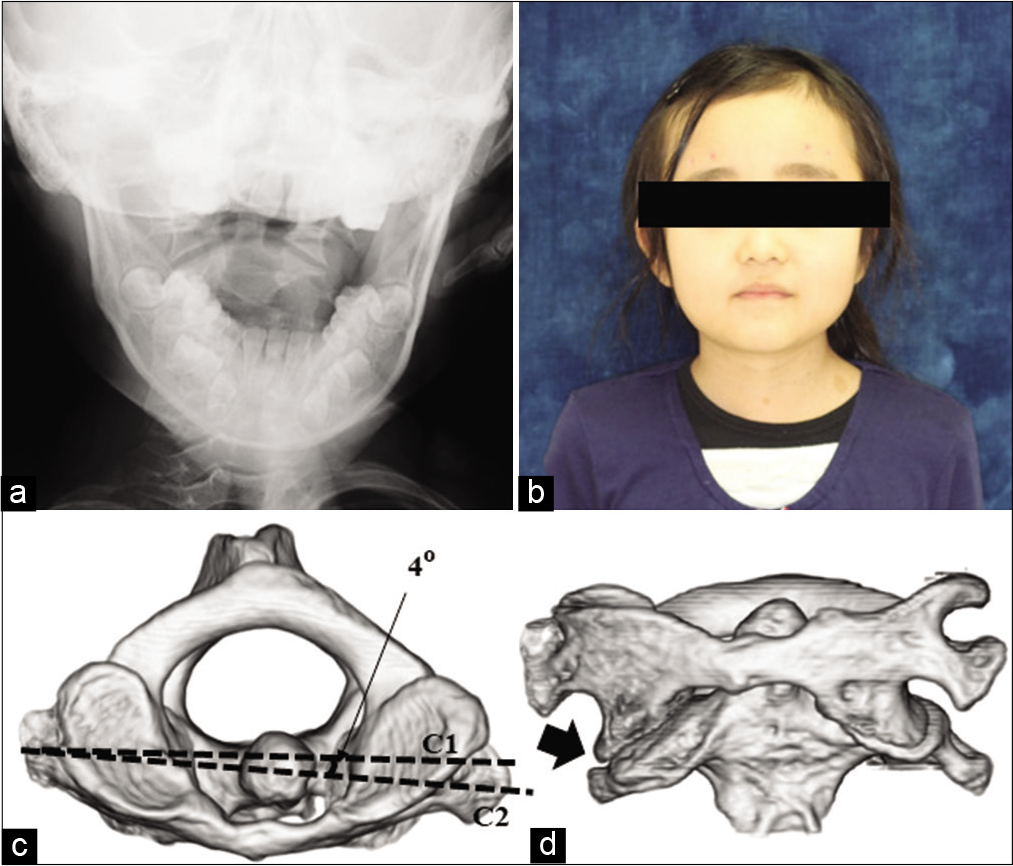
Case Description: A 7-year-old female with NF-1 presented with a 2-month history of torticollis and neck pain. C2 facet deformity had previously been identified on computed tomography (CT) before the onset of neck pain. Cervical radiography and CT showed AARF classified Fielding’s Type I and Ishii’s Grade II. Following 2 weeks of cervical traction, a closed reduction was followed by halo fixation that was utilized for 2 months. The patient fully recovered cervical range of motion following halo vest removal 4 months later. Further, the follow-up CT documented a normal atlantoaxial joint despite residual C2 facet deformity. In addition, no recurrence was evident 2 years later.
Conclusion: Halo fixation for chronic AARF with NF-1 proved effective. C2 facet deformity associated with NF-1 might have contributed to the onset of AARF.
Keywords: Chronic atlantoaxial rotatory fixation, Halo fixation, Neurofibromatosis type I
INTRODUCTION
Atlantoaxial rotatory fixation (AARF) is defined as dislocation or subluxation of the atlantoaxial joint. It occurs predominantly in children.[
CASE PRESENTATION
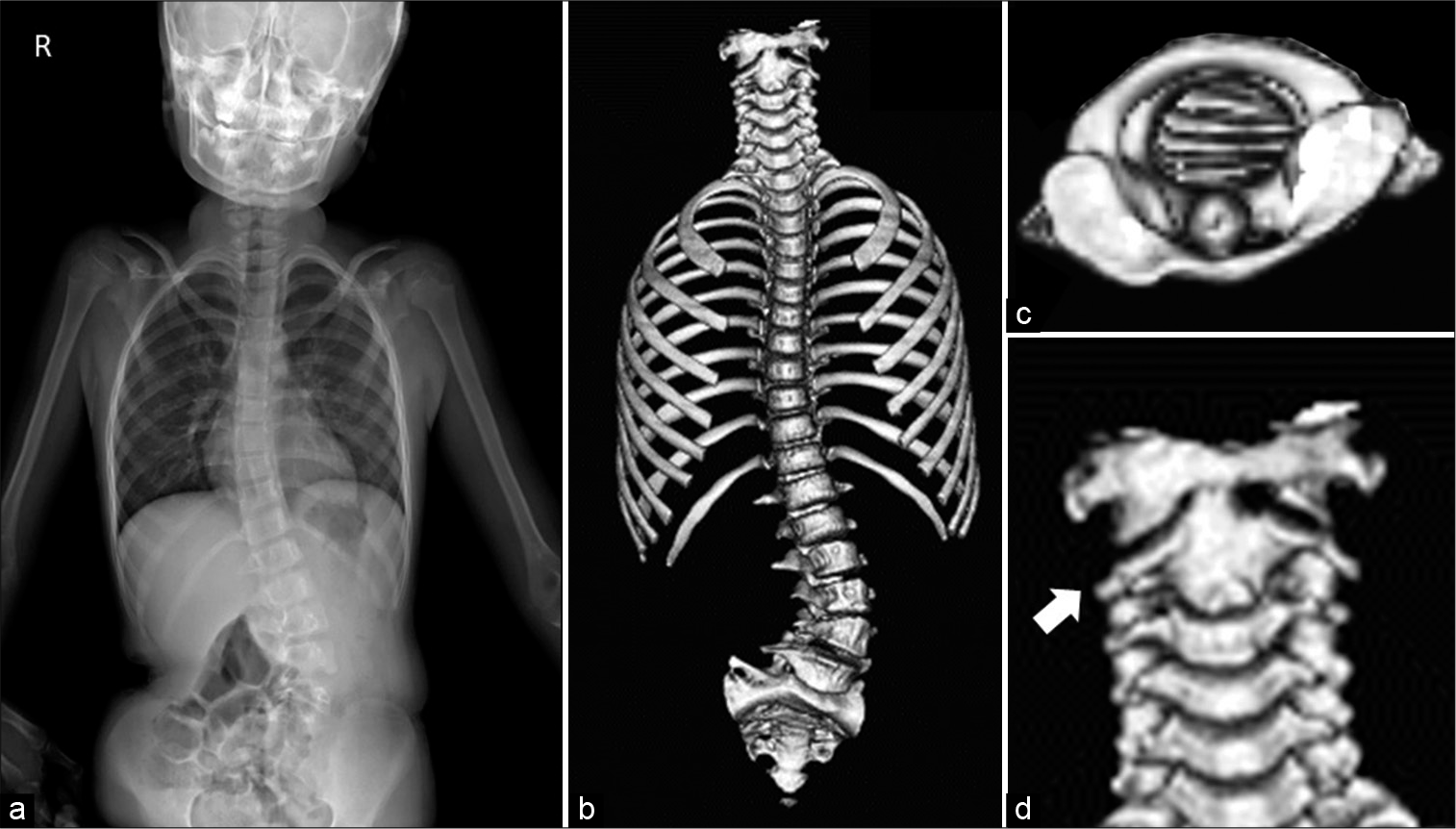
A 7-year-old female with NF-1 presented with a 2-month history of torticollis and neck pain. She had been diagnosed with NF-1 due to the presence of scoliosis and café-aulait spots. Radiographs previously showed a left convex scoliosis with a Cobb angle of 40º between L2 and L5 levels [
On examination, she had a left head tilt (i.e., the typical “cock-robin” posture). Cervical radiography and CT revealed that the C1-C2 joint was locked with C1 rotated 32° to the left and a C2 facet deformity [
Closed reduction and halo fixation
Three months after symptoms onset, a closed reduction and halo fixation were performed under general anesthesia [
DISCUSSION
Causes of AARF include trauma, infection, rheumatoid arthritis, surgery of the head and neck, and congenital diseases (i.e., Down syndrome, Morquio syndrome, and Marfan syndrome).[
CONCLUSION
We successfully performed a closed reduction and halo fixation to treat chronic AARF in a child with NF-1.
Ethical approval
Informed consent was obtained from the patient and her family before data use, and patient confidentiality was assured.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Akbarnia BA, Gabriel KR, Beckman E, Chalk D. Prevalence of scoliosis in neurofibromatosis. Spine (Phila Pa 1976). 1992. 17: S244-8
2. Burkus JK, Deponte RJ. Chronic atlantoaxial rotatory fixation correction by cervical traction, manipulation, and bracing. J Pediatr Orthop. 1986. 6: 631-5
3. Craig JB, Govender S. Neurofibromatosis of the cervical spine. A report of eight cases. J Bone Joint Surg. 1992. 74: 575-8
4. Fielding JW, Hawkins RJ. Atlanto-axial rotatory fixation. (Fixed rotatory subluxation of the atlanto-axial joint). J Bone Joint Surg Am. 1977. 59: 37-44
5. Ishii K, Chiba K, Maruiwa H, Nakamura M, Matsumoto M, Toyama Y. Pathognomonic radiological signs for predicting prognosis in patients with chronic atlantoaxial rotatory fixation. J Neurosurg Spine. 2006. 5: 385-91
6. Ishii K, Toyama Y, Nakamura M, Chiba K, Matsumoto M. Management of chronic atlantoaxial rotatory fixation. Spine (Phila Pa 1976). 2012. 37: E278-85
7. Sirois JL, Drennan JC. Dystrophic spinal deformity in neurofibromatosis. J Pediatr Orthop. 1990. 10: 522-6
8. Tauchi R, Imagama S, Kanemura T, Yoshihara H, Sato K, Deguchi M. The treatment of refractory atlanto-axial rotatory fixation using a halo vest: Results of a case series involving seven children. J Bone Joint Surg Am. 2011. 93: 1084-7