- Department of Surgery, Division of Neurosurgery, University of Toronto, Toronto, Ontario, Canada
- Division of Neurosurgery, Toronto Western Hospital, Toronto, Ontario, Canada
Correspondence Address:
Mohammed F. Shamji
Department of Surgery, Division of Neurosurgery, University of Toronto, Toronto, Ontario, Canada
Division of Neurosurgery, Toronto Western Hospital, Toronto, Ontario, Canada
DOI:10.4103/2152-7806.174883
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shamji MF, Alotaibi N, Ghare A, Fehlings MG. Chronic hypertrophic nonunion of the Type II odontoid fracture causing cervical myelopathy: Case report and review of literature. Surg Neurol Int 25-Jan-2016;7:
How to cite this URL: Shamji MF, Alotaibi N, Ghare A, Fehlings MG. Chronic hypertrophic nonunion of the Type II odontoid fracture causing cervical myelopathy: Case report and review of literature. Surg Neurol Int 25-Jan-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/chronic-hypertrophic-nonunion-of-the-type-ii-odontoid-fracture-causing-cervical-myelopathy-case-report-and-review-of-literature/
Abstract
Background:Complications of nonunited Type II odontoid fractures can range from neck pain to progressive neurological deficit from cervical myelopathy. Rarely, the hypertrophic nonunion requires both anterior transoral decompression and posterior decompression with instrumented fusion. We present a case and review literature around this entity.
Case Description:A 68-year-old female presented with rapidly progressive cervical myelopathy (from normal to moderate myelopathy modified Japanese Orthopedic Association [mJOA] 13) over 3 months. Her history was positive for a Type II odontoid fracture managed conservatively and lost to follow-up for 25 years. Spinal imaging studies revealed hypertrophic nonunion and craniocervical kyphotic deformity with significant subaxial stenosis and segmental kyphosis. The patient underwent anterior transoral decompression, followed by posterior occipitothoracic decompression and instrumented fusion. At follow-up, the cervical myelopathy has improved to near normalcy (mJOA 17) with no evidence or implant-related complication.
Conclusion:Rarely, nonunion of Type II odontoid fractures may be hypertrophic where both instability and compression cause neurological morbidity. Such cases require anterior transoral decompression, posterior cervical decompression, and instrumented fusions.
Keywords: Hypertrophic pseudoarthrosis, myelopathy, nonunion, odontoid fracture, transoral surgery
INTRODUCTION
Odontoid fractures are among the most common injuries at the craniocervical junction and account for nearly one in six cervical spine fractures. Various algorithms have been proposed for the management of Type II odontoid fractures, with nonsurgical management including cervical orthosis and halo-vest and surgical management including both anterior and posterior options.[
The hazards of nonunited odontoid fractures in adults can include mechanical neck pain[
CASE REPORT
We present the case of a 68-year-old female with a past medical history significant for a Type II odontoid fracture sustained 25 years previously. This presented originally with neck pain and was detected on spinal radiographs, with conservative management in a soft cervical orthosis implemented. There was no further clinical or radiological follow-up for her condition.
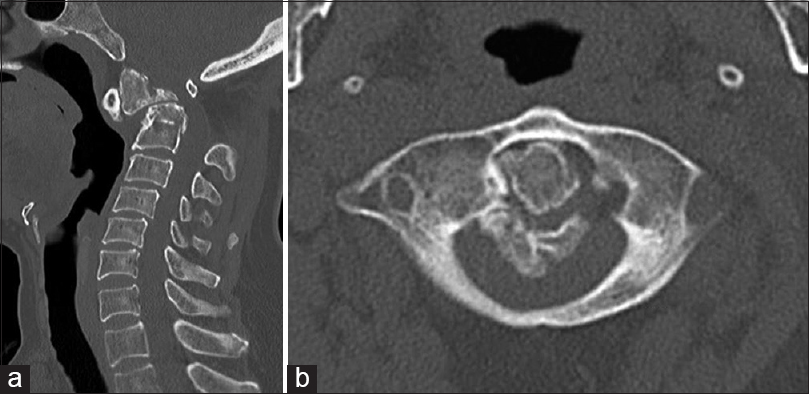
She presented with 6 months of progressive cervical myelopathy that manifests as upper extremity weakness and hand incoordination, extremity paresthesiae, and gait instability. Her modified Japanese Orthopedic Association score (mJOA) was 13. On physical examination, she exhibited increased tone and diffused hyperreflexia, unsteady broad-based and hesitant gait, and bilateral Hoffman and Babinski signs. Computed tomography (CT) [
Figure 1
A 68-year-old female with remote odontoid fracture presents 25 years later with acutely progressive myelopathy. Computed tomography (sagittal, a) demonstrates a chronic odontoid pseudoarthrosis with anterior subluxation, significant osteophyte (arrow), and segmental kyphosis. Axial section (b) demonstrates the severity of canal compromise arising from the combination of deformity and heterotopic osseous formation
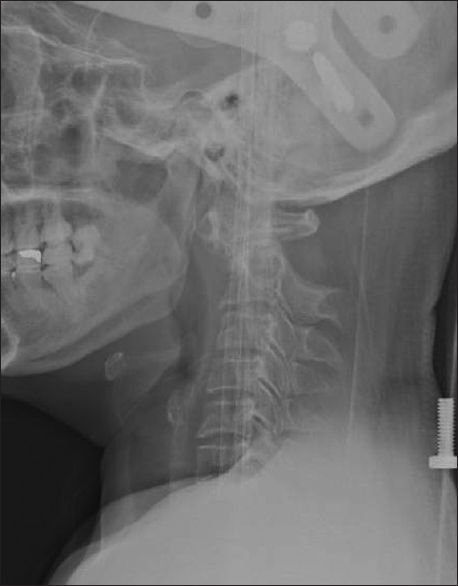
At surgery, following awake preoperative halo traction revealing the deformity to be mobile, permitting kyphosis reduction [
The patient was discharged home in a halo orthosis. At 4 months follow-up, she neurologically improved to functional independence (mJOA 17), with no evidence of pseudoarthrosis or implant failure on CT scan [
DISCUSSION
The mechanisms that underlie nonunion of the odontoid are likely multifactorial. Kirankumar et al.[
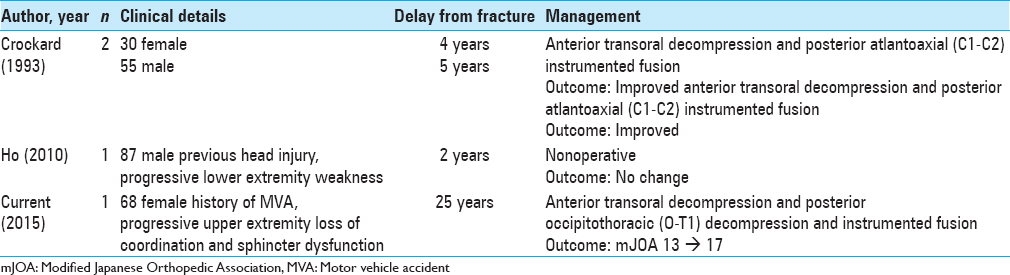
While nonunion of Type II odontoid fractures is common and the various surgical techniques to address this are within the armamentarium of the complex spinal surgeon, there is further substantial complexity when the nonunion is accompanied by hypertrophy of surrounding structures. The sparse literature surrounding the management of such hypertrophic deformity is summarized in
CONCLUSION
This case highlights the structural and neurological hazard of the nonunited odontoid fracture in young patients. This patient developed a complex craniocervical deformity with fragment subluxation, kyphosis, and osteophyte formation, with a long-term neurological consequence of myelopathy. Hypertrophic nonunion of Type II odontoid fractures occur rarely as a cause of progressive cervical myelopathy and requires different management inclusive of spinal cord decompression than that advocated for more straightforward atrophic nonunion in which realignment and stabilization may be the primary surgical objectives. Close follow-up after either initial conservative or surgical management remains important to protect these patients from such delayed complication.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974. 56: 1663-74
2. Avila-Guerra M. Chronic neck pain associated with an old odontoid fracture: A rare presentation. Case Rep Emerg Med 2013. 2013. p.
3. Boldin C, Grechenig W, Fankhauser F. Accident-induced late complaint of odontoid nonunion. Spine (Phila Pa 1976). 2004. 29: E169-71
4. Buchowski JM, Kebaish KM, Ahn NU, Suk KS, Kostuik JP. Odontoid fracture in a 50-year-old patient presenting 40 years after cervical spine trauma. Orthopedics. 2003. 26: 1061-3
5. Crockard HA, Heilman AE, Stevens JM. Progressive myelopathy secondary to odontoid fractures: Clinical, radiological, and surgical features. J Neurosurg. 1993. 78: 579-86
6. Dunbar HS, Ray BS. Chronic atlanto-axial dislocations with late neurologic manifestations. Surg Gynecol Obstet. 1961. 113: 757-62
7. Hadley MN, Dickman CA, Browner CM, Sonntag VK. Acute axis fractures: A review of 229 cases. J Neurosurg. 1989. 71: 642-7
8. Ho AW, Ho YF. Atlanto-axial deformity secondary to a neglected odontoid fracture: A report of six cases. J Orthop Surg (Hong Kong). 2010. 18: 235-40
9. Kirankumar MV, Behari S, Salunke P, Banerji D, Chhabra DK, Jain VK. Surgical management of remote, isolated type II odontoid fractures with atlantoaxial dislocation causing cervical compressive myelopathy. Neurosurgery. 2005. 56: 1004-12
10. Koivikko MP, Kiuru MJ, Koskinen SK, Myllynen P, Santavirta S, Kivisaari L. Factors associated with nonunion in conservatively-treated type-II fractures of the odontoid process. J Bone Joint Surg Br. 2004. 86: 1146-51
11. Moskovich R, Crockard HA. Myelopathy due to hypertrophic nonunion of the dens: Case report. J Trauma. 1990. 30: 222-5
12. Rudzki JR, Lenke LG, Blanke K, Riew KD. Pseudarthrosis of a thirty-nine-year-old dens fracture causing myelopathy. A case report. J Bone Joint Surg Am. 2004. 86-A: 2509-13