- Department of Plastic and Reconstructive Surgery, University of Wisconsin Hospitals and Clinics, Madison, Wisconsin, United States
- Department of Neurological Surgery, University of Wisconsin Hospitals and Clinics, Madison, Wisconsin, United States.
Correspondence Address:
Amgad Hanna, Department of Neurological Surgery, University of Wisconsin Hospitals and Clinics, Madison, Wisconsin, United States.
DOI:10.25259/SNI_824_2023
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mary K. Carbullido1, Paul Samuel Page2, Amgad Hanna2. Clavicular window for brachial plexus schwannoma removal. 19-Apr-2024;15:135
How to cite this URL: Mary K. Carbullido1, Paul Samuel Page2, Amgad Hanna2. Clavicular window for brachial plexus schwannoma removal. 19-Apr-2024;15:135. Available from: https://surgicalneurologyint.com/surgicalint-articles/12864/
Abstract
Background: Schwannomas are benign nerve sheath tumors that can either be sporadic or part of neurofibromatosis type 2 (NF2). Tumors of the brachial plexus (BP) with both supra- and infraclavicular components are uncommon and represent a challenge to complete surgical resection. There are few reports on single clavicular osteotomies for BP exposure; however, there are currently no reports of utilization of a clavicular window for a large schwannoma resection.
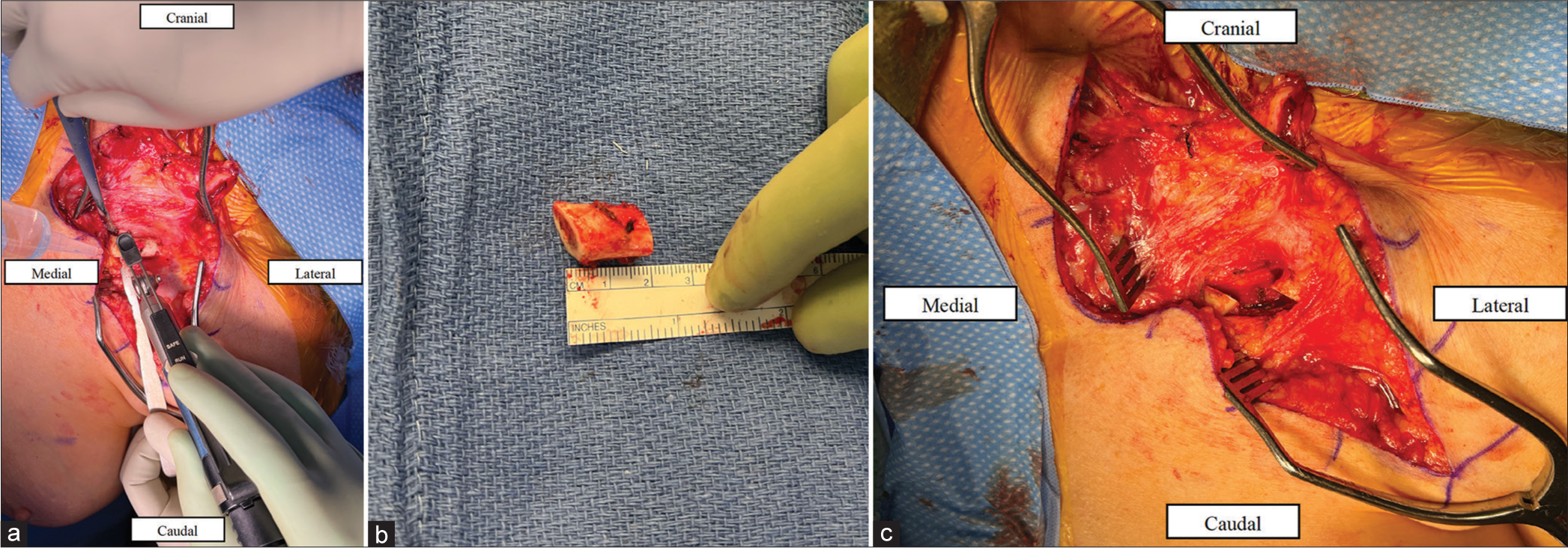
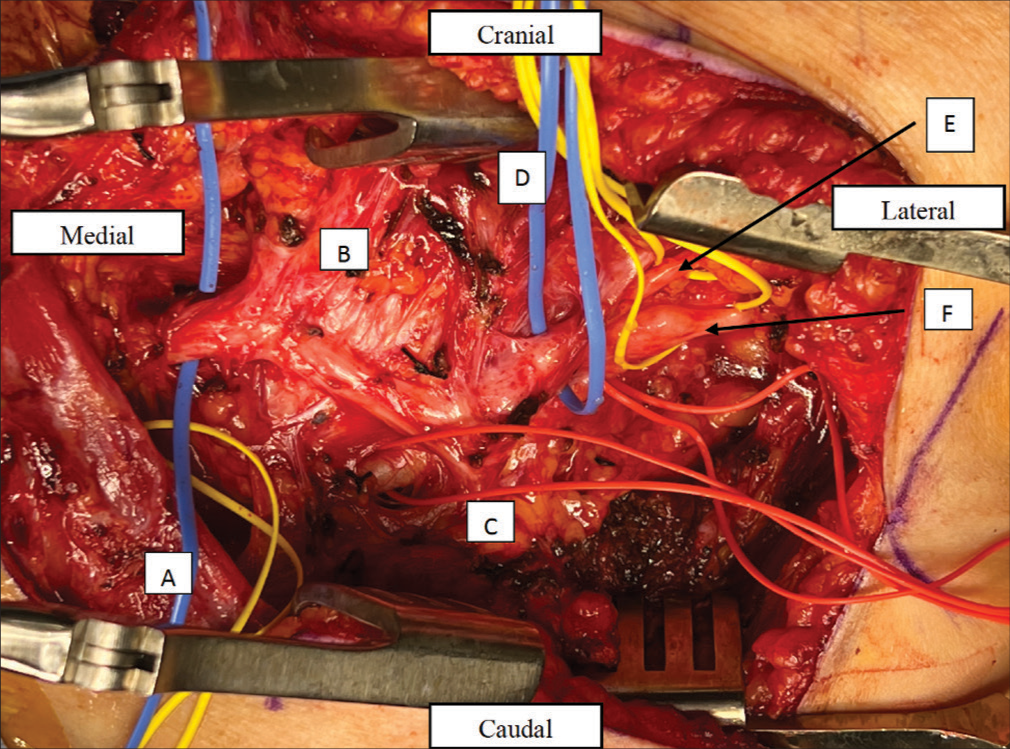
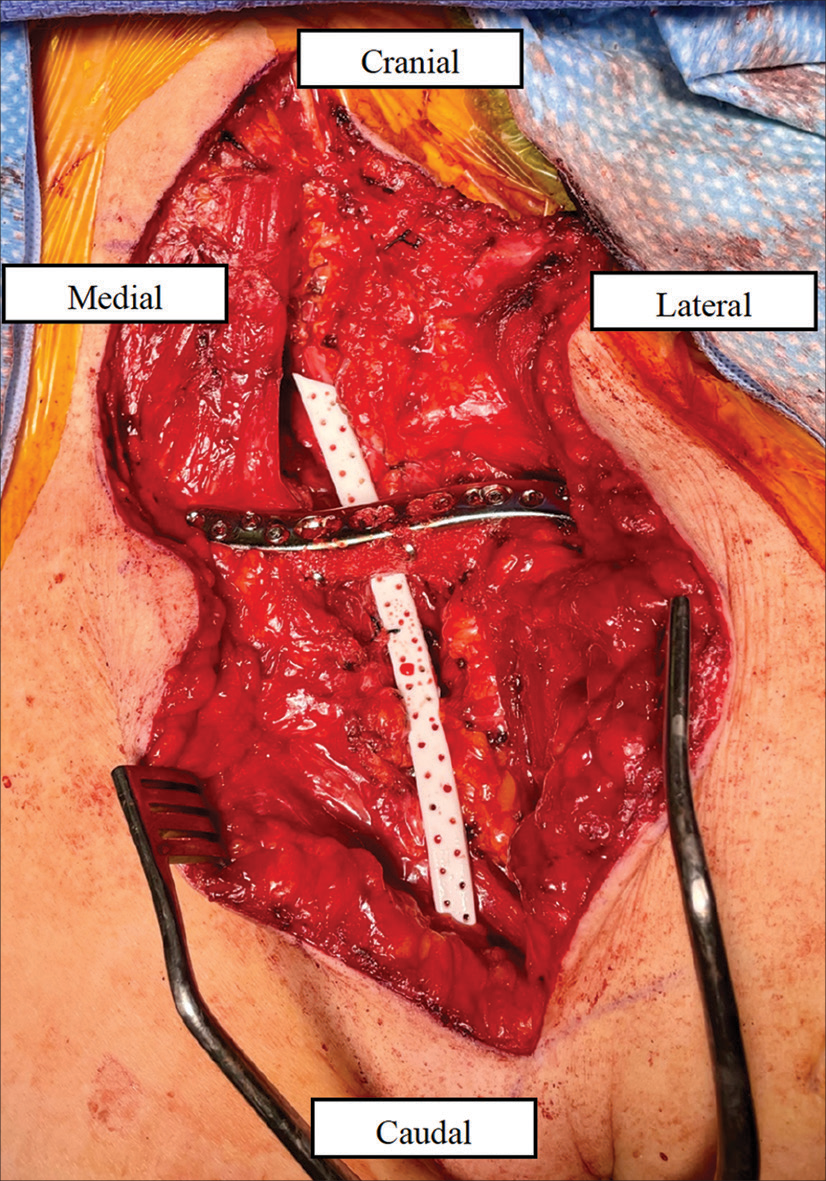
Case Description: We report a case of a patient with a schwannoma spanning the BP roots to the cords, with the majority involving the retro clavicular inferior trunk in the setting of NF2. The patient underwent previous subtotal resection and had postoperative enlargement of the residual mass. A gross total resection was made possible by the creation of a clavicular window to expose the BP. A 2 cm segment piece of the mid-clavicle was removed, allowing for roughly 6 cm of mediolateral exposure through clavicular distraction. This clavicular window facilitated complete exposure of the BP schwannoma underneath the clavicle as well as unobstructed exposure of supraclavicular and infraclavicular tumor. The segment was then refixed with a plate after resection of the tumor.
Conclusion: The use of a clavicular window allowed for extensive exposure of the trunks and divisions of the BP to achieve a gross total resection in this case. The clavicular window approach may provide a benefit for optimizing exposure in the setting of lesions involving the trunks and divisions that the clavicle would traditionally obstruct.
Keywords: Brachial plexus, Clavicle window, Neurilemmoma, Neurofibromatosis, Schwannoma
INTRODUCTION
Schwannomas, or neurilemmomas, are the most common tumors of nerves. They arise from Schwann cells, which form myelin and aid in axonal recovery and regeneration in the event of damage. Schwannomas are benign tumors that are painless and slowly growing, often presenting as a palpable mass with minimal sensory or motor symptoms.[
Typically, clavicular osteotomy without block resection is used to access the plexus divisions that run retroclavicularly.[
CASE DESCRIPTION
Background
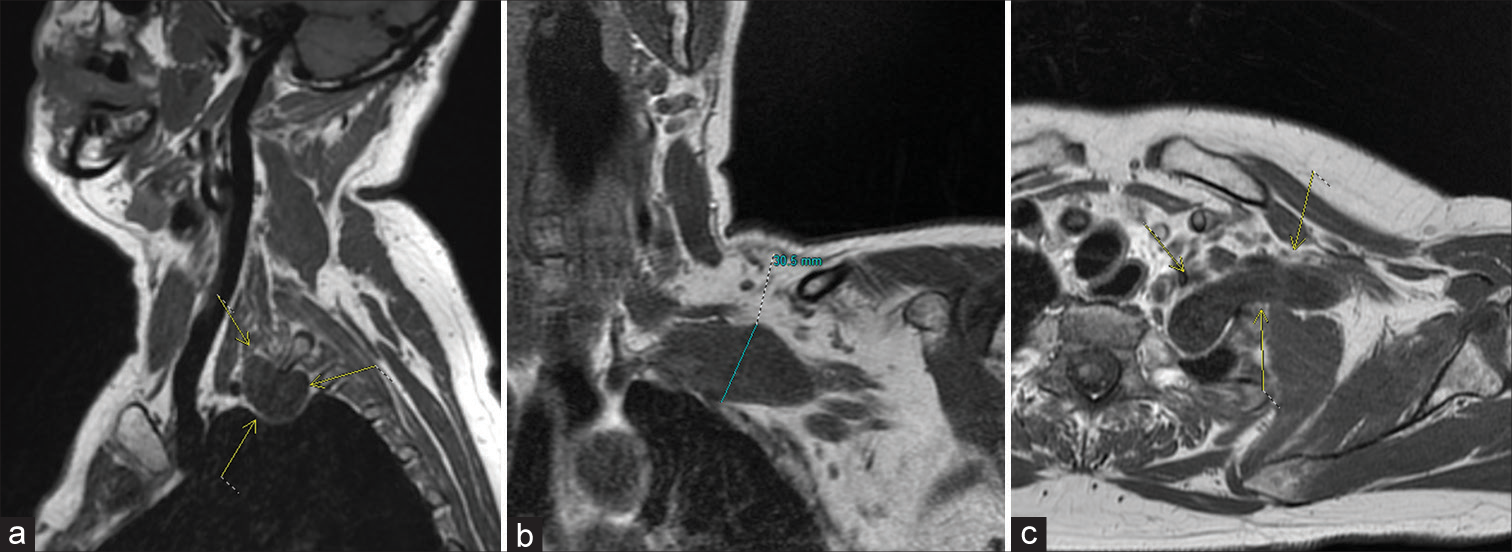
A 48-year-old female presented with recurrent schwannoma to the left BP. She has a history of neurofibromatosis type 2 (NF2) with vestibular schwannomas, multiple intracranial meningiomas, and spinal foraminal schwannomas. She underwent multiple schwannoma excisions, meningioma resections, and radiation therapy to her vestibular schwannomas. She established care with our team at 42 years old and presented with a left supraclavicular mass associated with neck pain that radiated down her lateral arm. Other symptoms included numbness, tingling, and coldness in her fingers. Physical examination was significant for positive Tinel’s sign at the mass and decreased sensation in the C8 distribution. Magnetic resonance imaging (MRI) confirmed a left lower trunk contrast-enhancing mass. She underwent subtotal resection one year after establishing care, and surgical pathology confirmed a schwannoma (the World Health Organization grade 1). The mass located underneath the clavicle was left due to limited visualization in the operative field despite supra and infraclavicular approaches. She had a slow postoperative recovery, which ultimately resulted in nearly full grip strength and functionality but continued decreased sensation at her middle finger. Nearly five years after her initial surgery, she noticed the slow recurrence of radiating pain by her left clavicle throughout her left upper extremity. Follow-up MRI revealed an interval increase in the size of the residual tumor to 65 cm × 31 cm × 27 cm [
Figure 1:
(a-c) Magnetic resonance imaging T1 imaging of the left brachial plexus schwannoma. (a) Sagittal view of the brachial plexus schwannoma with arrows locating the tumor. (b) Coronal view of the schwannoma with maximal height annotated. (c) Axial view of the schwannoma with arrows locating the tumor.
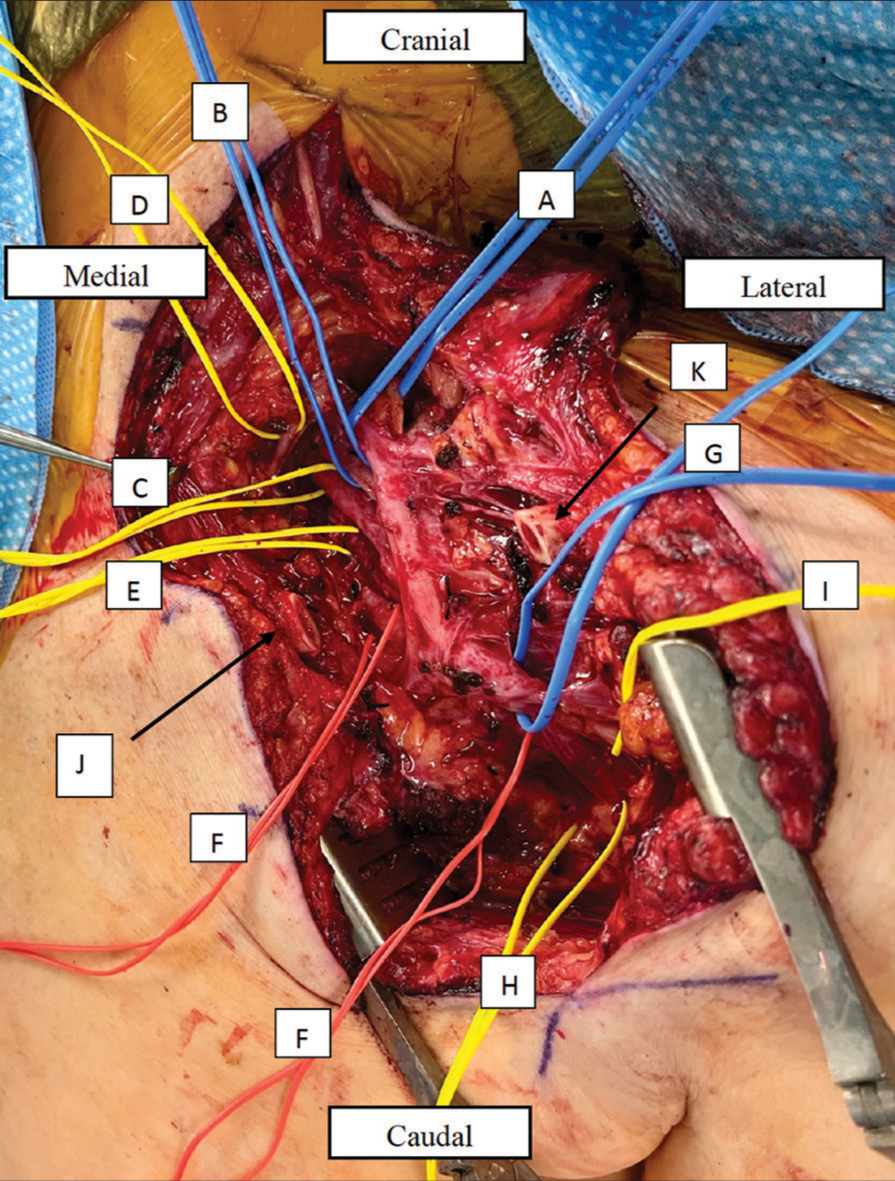
Surgery
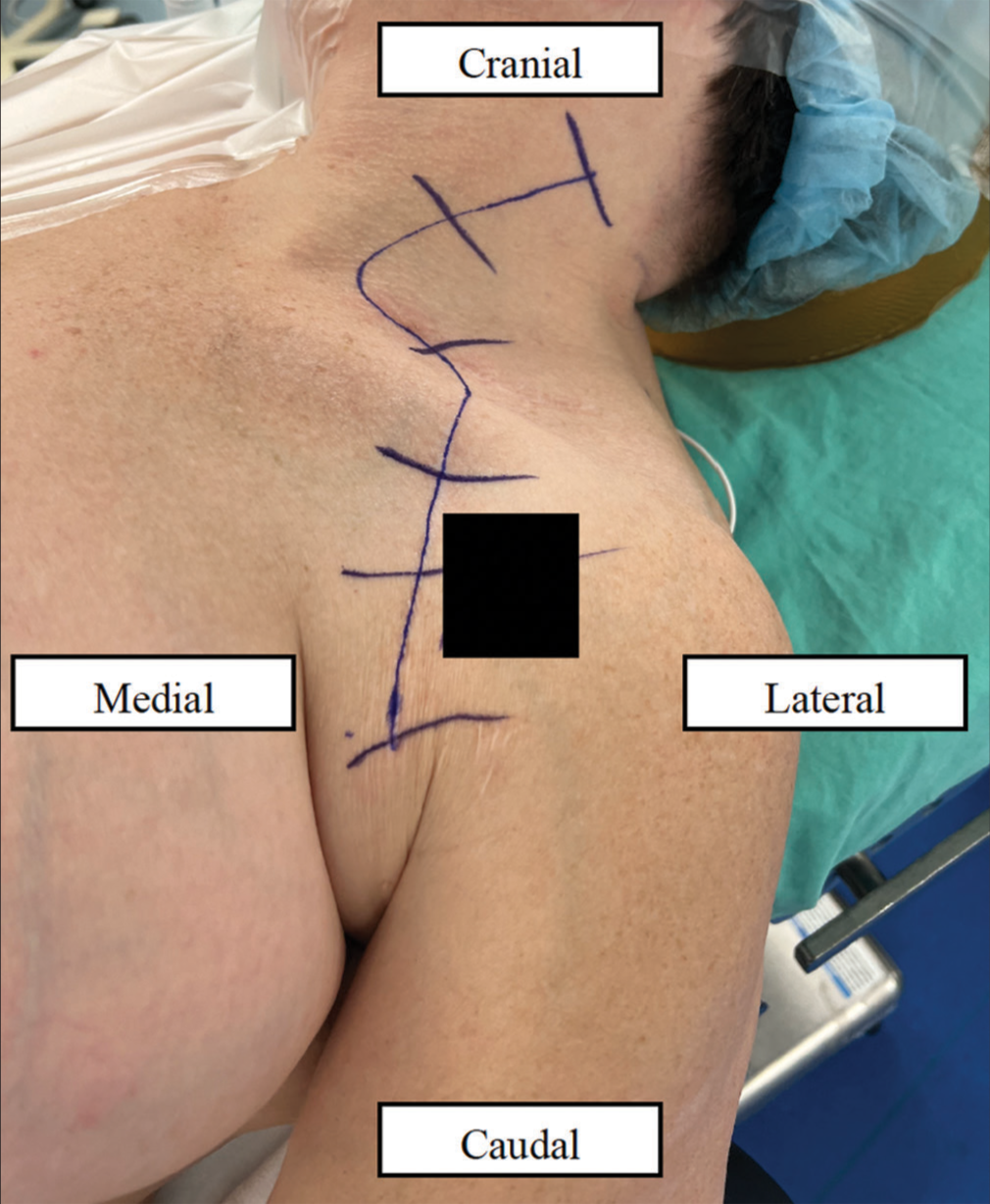
The patient was positioned supine with the head turned to the right under general anesthesia, and a curvilinear incision [
Postoperative course
The patient was seen three months postoperatively with the resolution of her left arm pain. She had residual weakness of finger abduction but was able to use her arm functionally. Her clavicle healed without complication. Postoperative imaging revealed successful resection of the mass.
DISCUSSION
In this case report, a patient with NF2 disease underwent initial debulking of a BP schwannoma with symptomatic recurrence five years later. According to a spinal schwannoma study by Fehlings et al., recurrence after surgery is approximately 5% and occurs several years after resection.[
The clavicle is a bone that allows for a full shoulder range of motion while protecting the BP and large vascular structures such as the subclavian artery and vein.[
When a single osteotomy is utilized to transect the clavicle, exposure is limited by the ability to retract the two clavicular segments medially and laterally. That distance is also mitigated by retaining the full length of the clavicle. Another approach with a single osteotomy is to rotate the two segments out of the operative field. Exposure with this approach is, however, limited by the arch of rotation and the soft-tissue connections to the clavicle that keep it in place. This type of retraction may also distort the BP anatomy and may increase the risk of injury to the delicate underlying neurovascular structures. The advantage of a clavicular window is better exposure with less need for soft-tissue retraction or rotation.
The clavicular window provides wide exposure to the BP that was successful in this report. Utilizing a clavicular window improved exposure of the distal trunks and their divisions when the clavicle would have otherwise limited access to this region. One theoretical difficulty would be to replace the removed clavicle fragment in the same spot without rotation; this could easily be avoided by preplacing the screw holes before cutting the clavicle. Short-term follow-up with this patient has so far been without complications, but there is still a risk of clavicular non-union, BP neurapraxia from malunion,[
Ultimately, the clavicular window allows for extensive BP exposure for total resection of BP tumors that span the length of supraclavicular and infraclavicular components of the BP with significant retroclavicular involvement. Due to bony segment resection, there are less retraction and rotation forces on the surrounding soft tissue that may distort or create traction injury to the BP as compared to if the full length of the clavicle was left in place. The clavicular window should be considered when the surgical approach requires wide exposure of the retroclavicular BP.
CONCLUSION
A mid-clavicular window is created by removing a segment of clavicular bone for wide exposure in a case of BP schwannoma with significant retroclavicular involvement. This is a novel method that has not yet been described and may offer a better option for extensive retro clavicular schwannomas or tumors spanning the entire length of the supraclavicular and infraclavicular BP to aid in more complete resection.
Ethical approval
The Institutional Review Board approval is not required. Patient related content reviewed by institution HIPAA committee.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Beliaev AM, Fougere C. Thoracic outlet syndrome secondary to a mid-clavicle malunion. BMJ Case Rep. 2015. 2015: bcr2015209583
2. Bonnard C, Chapuis JM, Narakas AO. L’ostéotomie de la clavicule avec préostéosynthèse. Son indication et sa technique dans l’exploration du plexus brachial [Osteotomy of the clavicle with preosteosynthesis, Its indications and technic in the exploration of the brachial plexus]. Helv Chir Acta. 1984. 51: 589-600 [French]
3. Brennwald J, Nigst H. Klavikula-Osteotomie und osteosynthese bei operationen am plexus brachialis [Osteotomy and osteosynthesis of the clavicle in brachial plexus surgery]. Handchir Mikrochir Plast Chir. 1985. 17: 277-9 [German]
4. Chen CE, Liu HC. Delayed brachial plexus neurapraxia complicating malunion of the clavicle. Am J Orthop (Belle Mead NJ). 2000. 29: 321-2
5. Fehlings MG, Nater A, Zamorano JJ, Tetreault LA, Varga PP, Gokaslan ZL. Risk factors for recurrence of surgically treated conventional spinal schwannomas: Analysis of 169 patients from a multicenter international database. Spine (Phila Pa 1976). 2016. 41: 390-8
6. Gopinathan NR, Dhillon MS, Kumar R. Surgical technique: Simple technique for removing a locking recon plate with damaged screw heads. Clin Orthop Relat Res. 2013. 471: 1572-5
7. Goyal A, Mahan MA, Maniker AH, Belzberg AJ, editors. Benign and malignant tumors of the peripheral nerve. Youmans and Winn neurological surgery. Philadelphia, PA: Elsevier Saunders; 2208. 285: 22.e4
8. Hyland S, Charlick M, Varacallo M, editors. Anatomy, shoulder and upper limb, clavicle. StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. p. Available from: https://www.ncbi.nlm.nih.gov/books/NBK525990 [Last accessed on 2022 Jul 22]
9. Lusk MD, Kline DG, Garcia CA. Tumors of the brachial plexus. Neurosurgery. 1987. 21: 439-53
10. Takahashi T, Hirai T, Yoshii T, Inose H, Yuasa M, Matsukura Y. Risk factors for recurrence and regrowth of spinal schwannoma. J Orthop Sci. 2023. 28: 554-9
11. Tang CY, Fung B, Fok M, Zhu J. Schwannoma in the upper limbs. Biomed Res Int. 2013. 2013: 167196
12. Tse R, Pondaag W, Malessy M. Exposure of the retroclavicular brachial plexus by clavicle suspension for birth brachial plexus palsy. Tech Hand Up Extrem Surg. 2014. 18: 85-8
13. Thatte MR, Agashe M, Rathod C, Lad P, Mehta R. An approach to the supraclavicular and infraclavicular aspects of the brachial plexus. Tech Hand Up Extrem Surg. 2011. 15: 188-97
14. Zadnik M, Eglseder WA, Shur VB. Transclavicular approach for brachial plexus reconstruction. Tech Hand Up Extrem Surg. 2008. 12: 126-30