- Department of Neuroscience, Winthrop Neuroscience, Winthrop University Hospital, Mineola, New York, USA
Correspondence Address:
Nancy E. Epstein
Department of Neuroscience, Winthrop Neuroscience, Winthrop University Hospital, Mineola, New York, USA
DOI:10.4103/2152-7806.194515
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein. Commentary on the management of type II odontoid process fractures in octogenarians: Article by Graffeo et al. and Editorial by Falavigna (J Neurosurgery Spine August 19, 2016). 21-Nov-2016;7:
How to cite this URL: Nancy E. Epstein. Commentary on the management of type II odontoid process fractures in octogenarians: Article by Graffeo et al. and Editorial by Falavigna (J Neurosurgery Spine August 19, 2016). 21-Nov-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/commentary-on-the-management-of-type-ii-odontoid-process-fractures-in-octogenarians-article-by-graffeo-et-al-and-editorial-by-falavigna-j-neurosurgery-spine-august-19-2016/
Abstract
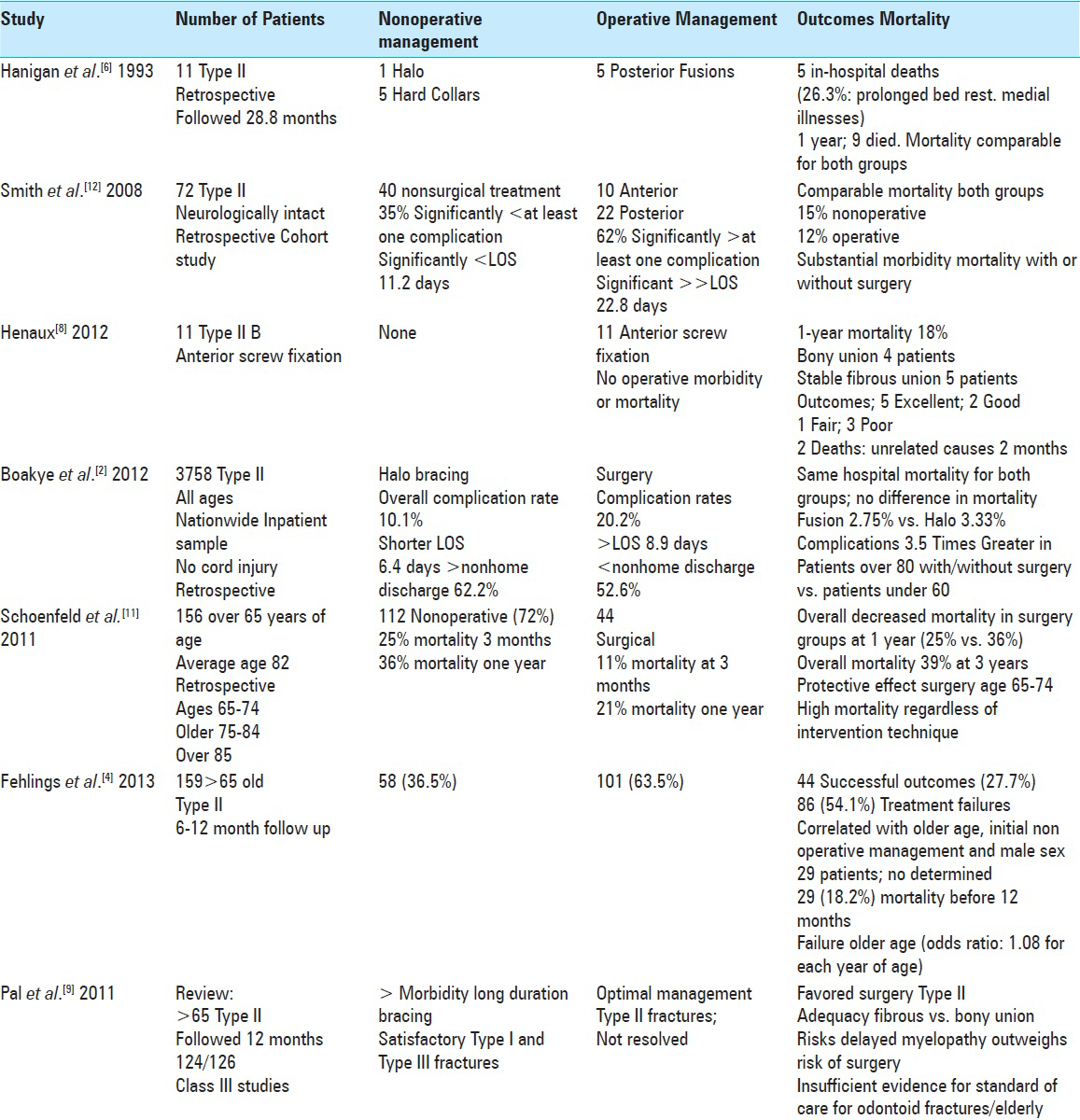
Background:Establishing a clear treatment paradigm for octogenarians with type II odontoid fractures in hampered by a literature replete with level III articles.
Methods:In the study by Graffeo et al., the authors evaluated 111 patients over the age of 79 (average age: 87) with type II odontoid fractures undergoing nonoperative (94 patients) vs. operative intervention (17 total; 15 posterior and 2 anterior). They studied multiple variables and utilized several scales [abbreviated injury scale (AIS), injury severity score (ISS), and the Glasgow coma scale (GCS)] to determine the outcomes of nonoperative vs. operative management.
Results:Graffeo et al. concluded that there were no significant differences between nonoperative and operative management for type II odontoid fractures in octogenarians. They found similar frequencies of additional cervical fractures, mechanisms of injury, GCS of 8 or under, AIS/ISS scores, and disposition to “nonhome” facilities. Furthermore, both appeared to have increased mortality rates at 1-year post injury; 13% during hospitalization, 26% within the first post-injury month, and 41% at 1 year.
Conclusions:In the editorial by Falavigna, his major criticism of Graffeo's article was the marked disparity in the number of patients in the operative (17 patients) vs. the nonoperative group (94 patients), making it difficult to accept any conclusions as “significant”. He further noted that few prior studies provided level I evidence, and that most, like this one, were level III analyses that did not “significantly” advance our knowledge as to whether to treat octogenarians with type II odontoid fractures operatively vs. nonoperatively.
Keywords: Cons, conservative management, pros, octogenarians, odontoid fractures, surery, type II
INTRODUCTION
Falavigna's critique of the radiographic diagnosis of type II fractures in the Graffeo et al. study
In “Deadly falls: Operative versus nonoperative management of Type II odontoid process fracture in octogenarians” (J Neurosurgery Spine, 2016; August 19), Graffeo et al. retrospectively evaluated the management of type II odontoid fractures in 111 octogenarians (e.g., patients over the age of 79, average age of 87) between 1998 and 2014; 94 patients were treated nonoperatively whereas 17 underwent surgery.[
Similar clinical/other data for Graffeo et al. nonoperative vs. operative management of type II odontoid fractures
There were no significant differences in some of the basic clinical data in Graffeo et al., i.e., nonoperative vs. operative populations. Although patients averaged 87 years of age (range: 80–104), there was a “small but significant increase in age” for those treated nonsurgically.[
Falavigna's criticism of Graffeo et al. study; disparate number of patients in nonoperative vs. operative groups
Of the original 111 patients in Graffeo et al. series, 94 were treated nonoperatively (e.g., hard cervical collars used in 85% of patients), whereas 17 had surgery (15 performed posteriorly, and 2 anteriorly). The 15 posterior fusions of C1-C2 utilized Harms and Melchier's segmental polyaxial screw fixation/rods technique.[
Falavigna criticized the study for the large disparity in the number of patients in the nonoperative vs. operative groups, noting that the study design severely limited “statistical analysis.” He also commented that the authors failed to utilize uniform “guidelines” as to which treatment modalities were chosen (e.g., surgeon's experience/preference appeared to largely determine the management strategy). Furthermore, adequate information regarding other critical variables was lacking; e.g. the ultimate fusion status of patients in the two groups, the time elapsed since type II fractures occurred, patients’ attendant comorbidities/medical risk factors, and the initial and final neurological status of patients.
Similar mortality rates in Graffeo et al. series with/without surgery
The average survival for both groups in Graffeo et al. series was 22 months (range: 0–129 months).[
Falavigna also criticized Graffeo et al. for summarily concluding outcomes and mortality rates for octogenarians with type II fractures were comparable with/without surgery based on retrospective data collected at just one institution.[
Recommendation for future analyses
At the end of his analysis, Falavigna cited the potential future advantages of a prospective randomized study (e.g., level I) to better determine optimal treatment for type II fractures in octogenarians. Reviewing the article by Graffeo et al. and editorial by Falavigna reminds us that many level III studies have fundamentally flawed study designs. In this case, the study by Graffeo et al. was a retrospective level III analysis that included an extremely small number of patients in the operative vs. nonoperative group, and spuriously came to the conclusion, without an adequate study design, that nonoperative and operative outcomes of Type II odontoid fracutres were comparable. In fact, this article would have been improved had the editor originally recommended the authors exclude the small operative group entirely, and only focus on improving their presentation of the clinical, radiographic, and nonoperative management of type II odontoid fractures in octogenarians.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Anderson LD, D’Alonzo RT. Fracture of the odontoid process of the axis. J Bone Joint Surg Am. 1974. 56: 1663-174
2. Boakye M, Arrigo RT, Kalanithi PS, Chen YR. Impact of age, injury severity score, and medical comorbidities on early complications after fusion and halo-vest immobilization for C2 fractures in older adults: A propensity score matched retrospective cohort study. Spine. 2012. 37: 854-9
3. Falavigna A. Editorial: Management of Type II Odontoid Process Fracture in Octogenarians. J Neurosurgery Spine. 2016. p.
4. Fehlings MG, Arun R, Vaccaro AR, Arnold PM, Chapman JR, Kopjar B. Predictors of treatment outcomes in geriatric patients with odontoid fractures: AO Spine North America multi-centre prospective GOF study. Spine. 2013. 38: 881-6
5. Graffeo CS, Perry A, Puffer RC, Carlstrom LP, Chang W, Mallory GW. Deadly falls: Operative versus nonoperative management of Type II odontoid process fracture in octogenarians. J Neurosurgery Spine. 2016. p.
6. Hanigan WC, Powell FC, Elwood PW, Henderson JP. Odontoid fractures in elderly patients. J Neurosurg. 1993. 78: 32-5
7. Harms J, Melchier RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine. 2001. 26: 2467-71
8. Hénaux PL, Cueff F, Diabira S, Riffaud L, Hamlat A, Brassier G. Anterior screw fixation of type IIB odontoid fractures in octogenarians. Eur Spine J. 2012. 21: 335-9
9. Pal D, Sell P, Grevitt M. Type II odontoid fractures in the elderly: An evidence-based narrative review of management. Eur Spine J. 2011. 20: 195-204
10. Sasso R, Doherty BJ, Crawford MJ, Heggeness MH. Biomechanics of odontoid fracture fixation. Comparison of the one- and two-screw technique. Spine. 1993. 18: 1950-3
11. Schoenfeld AJ, Bono CM, Reichmann WM, Warholic N, Wood KB, Losina E. Type II odontoid fractures of the cervical spine: Do treatment type and medical comorbidities affect mortality in elderly patients?. Spine. 2011. 36: 879-85
12. Smith HE, Kerr SM, Maltenfort M, Chaudhry S, Norton R, Albert TJ. J Early complications of surgical versus conservative treatment of isolated type II odontoid fractures in octogenarians: A retrospective cohort study. Spinal Disord Tech. 2008. 21: 535-9