- Department of Neurosurgery, University of Sao Paulo School of Medicine, Sao Paulo, Brazil
- Department of Neurological Surgery, Weill Cornell Medicine/ New York-Presbyterian Hospital, New York, United States
- Department of Neurosurgery, Air Force Galeão Hospital, Rio de Janeiro, Brazil
- Department of Neurological Surgery, State University of Ponta Grossa, Ponta Grossa, Brazil
- Department of Neurosurgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
- The Center for Advanced Neurology and Neurosurgery, Porto Alegre, Brazil
- Department of Neurosurgery, Presidente Antonio Carlos Institute of Tocantins, Porto Nacional, Tocantins, Brazil
- Department of Neurosurgery, University of Sao Paulo, Facultade das Clinicas, Sao Paulo, Brazil
Correspondence Address:
Ricardo Marques Lopes de Araujo, Department of Neurosurgery, University of São Paulo School of Medicine, São Paulo, Brazil.
DOI:10.25259/SNI_550_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ricardo Marques Lopes de Araujo1,2, Dan Zimelewicz Oberman3, Leonardo Christiaan Welling4, Bipin Chaurasia5, Alexander I. Evins2, Antonio Bernardo2, Gustavo Rassier Isolan6, Jose Paulo Dourado7, Nicollas Nunes Rabelo1, Eberval G. Figueiredo8. Comparative anatomical analysis between lateral supraorbital and minipterional approaches. 30-Aug-2024;15:305
How to cite this URL: Ricardo Marques Lopes de Araujo1,2, Dan Zimelewicz Oberman3, Leonardo Christiaan Welling4, Bipin Chaurasia5, Alexander I. Evins2, Antonio Bernardo2, Gustavo Rassier Isolan6, Jose Paulo Dourado7, Nicollas Nunes Rabelo1, Eberval G. Figueiredo8. Comparative anatomical analysis between lateral supraorbital and minipterional approaches. 30-Aug-2024;15:305. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13076
Abstract
Background: The pterional craniotomy, described by Yasargil and Fox in 1975, constitutes the most traditional and important surgical access in vascular neurosurgery. Minimally invasive alternatives include the minipterional (MP) and lateral supraorbital (LSO) craniotomies, which avoid complications such as injury to the frontal branch of the facial nerve, temporal muscle dysfunction, depression of the craniotomy site, frontal sinus opening, and cosmetically unacceptable outcomes. We evaluated and compared the exposures provided by MP and LSO craniotomies through quantitative measurements of the surgical exposure area around the circle of Willis and parasellar regions, as well as angular and linear exposures of the internal carotid artery (ICA) bifurcation, middle cerebral artery (MCA), midpoint of the anterior communicating artery, and tip of the basilar artery (BA).
Methods: Seven fresh cadavers were dissected at the São Paulo Medical Examiner’s Office, SP, and three at the skull base laboratory of Weill Cornell Medical College, New York, USA. The craniotomies were performed sequentially, initially with the LSO craniotomy followed by the MP. After the craniotomy, the surgical exposure area, craniotomy area, and angular exposures in the horizontal and vertical axes were determined.
Results: The MP craniotomy provided better angular exposure for the ipsilateral MCA, while the LSO craniotomy and BA provided better vertical axis exposures. The LSO craniotomy provided better angular exposure in the vertical axis for the midpoint of the anterior communicating artery and contralateral ICA bifurcation. Regarding surgical exposure and craniotomy area, there were no statistically significant differences.
Conclusion: The MP craniotomy offers a significantly larger surgical exposure compared to the LSO craniotomy, with specific advantages regarding angular exposure to important neurovascular structures. This study provides important quantitative data to guide the choice between these minimally invasive access techniques in vascular neurosurgery.
Keywords: Cerebral aneurysm, Lateral supraorbital, Minimally invasive approach, Minipterional craniotomy
INTRODUCTION
The fronto-temporo-sphenoidal craniotomy, conventionally known as the pterional (PT) craniotomy, established by Yasargil and Fox in 1975 [
Since its initial proposal by Yasargil and Fox [
In the age of minimally invasive techniques, the supraorbital approach was initially proposed by Reisch and Perneczky[
The MP craniotomy, described by Figueiredo et al. in 2007, was proposed as an alternative to the classical PT craniotomy to offer similar surgical corridors but with smaller incisions, leading to improved cosmetic and functional outcomes without compromising neurosurgical exposure.[
Our objective was to assess the surgical exposures provided by both the LSO and MP approaches. This was accomplished through measurements of surgical exposure areas surrounding the circle of Willis, as well as angular exposures in both the horizontal and vertical axes, to provide robust anatomical data that might clarify the distinctions between these approaches.
MATERIALS AND METHODS
Anatomical fresh cadaveric dissections were used within 24 h after death, and pertinent measurements were performed after institutionally approved by the Research Ethics Committee, under number 4640664 de 09 de abril de 2021(University of São Paulo). In addition, three formalin-fixed and injected with red and blue colored silicone rubber were carefully dissected at Weill Cornell University, New York, USA.
The approach was performed unilaterally in four specimens and bilaterally in three specimens, totaling ten sides. Cadavers were positioned in a supine position, with the head securely immobilized using a Mayfield headrest, simulating the typical neurosurgical positioning. A brain retractor (Codman Greenberg, Phoenix, Arizona, USA) was employed with minimal pressure on the cerebral tissue. The measurements were performed using a neuronavigation system (Artis Eximus, São Paulo, Brazil).
To mitigate bias resulting from individual anatomical differences, the craniotomies were systematically conducted in the same cadaver, beginning with the MP craniotomy and subsequently proceeding to the LSO approach [
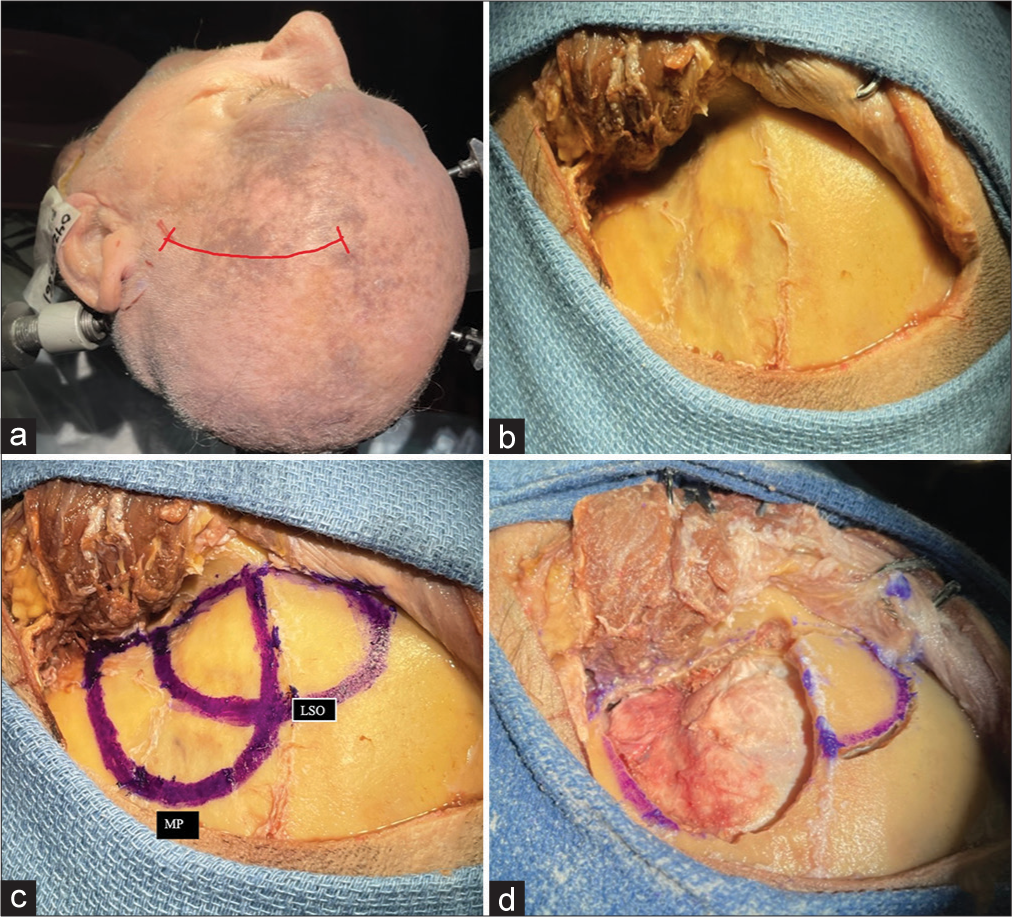
Figure 1:
Stepwise dissection in the lateral supraorbital and minipterional approach. (a) Positioning and marking of the incision for performing LSO and MP craniotomies on the left side; The curve define the skin incision made for the approach (b) after retracting the musculocutaneous flap, revealing the anatomical landmarks and reference points for the LSO and MP craniotomies; (c) marking of the LSO and MP craniotomies; and (d) exposition after performing the MP approach and the visualization before opening the dura mater. LSO: Lateral supraorbital, MP: Minipterional.
The MP technique was performed initially as described by Figueiredo et al.[
Quantification
Area of exposure
After each craniotomy, a data point was acquired by touching the tip of the digitizing probe to the anatomic points of interest while its position was recorded with cameras. The computer connected to the system recorded the x, y, and z data to locate each point of interest. The retractor was secured firmly to prevent measurement errors while the points were located spatially.
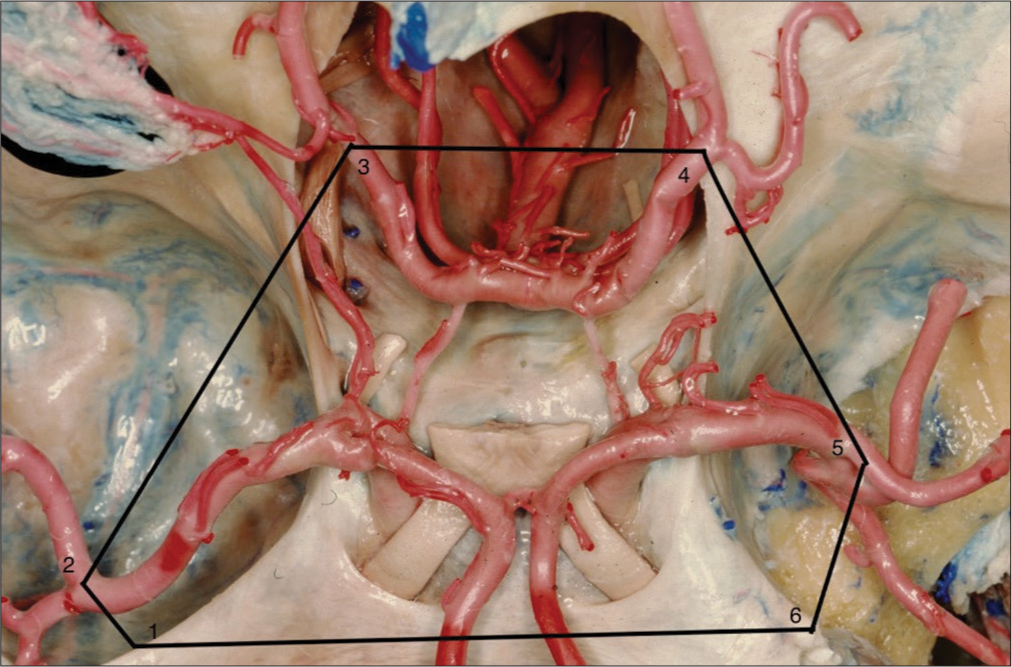
The exposure area was determined by a hexagon bounded by the points of interest (POI) around the circle of Willis. Anatomical targets were defined according to the surgical experience of the authors (EBF and RMLA) and based on relevant structures that could be reached with these craniotomies. Six points were used: (1) lateral aspect of the superior orbital fissure in the ipsilateral sphenoid wing; (2) bifurcation of the middle cerebral artery (MCA); (3) the most posterior point of the ipsilateral posterior cerebral artery; (4) the most posterior point of the contralateral posterior cerebral artery; (5) the most distal point of the contralateral MCA; and (6) the farthest lateral point of the contralateral lesser wing of the sphenoid [
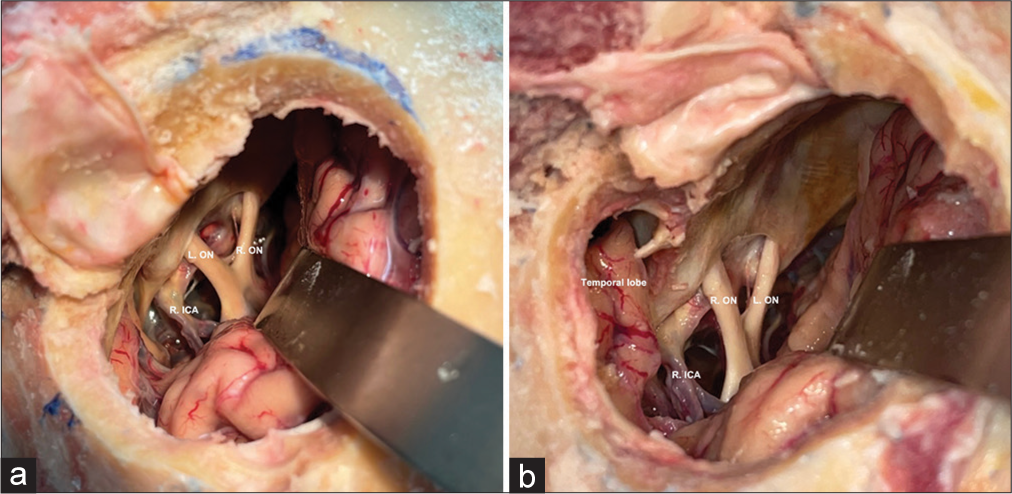
Figure 3:
Photograph in superior view of the base of the skull of an anatomical specimen with an illustrative drawing of the six anatomical points used in the calculation of the exposure area for each craniotomy. (1) Most lateral point of the superior orbital fissure in the lesser wing of the ipsilateral sphenoid bone; (2) bifurcation of the ipsilateral middle cerebral artery; (3) most distal point of the ipsilateral posterior cerebral artery; (4) most distal point of the contralateral posterior cerebral artery; (5) most distal point of the contralateral middle cerebral artery; and (6) most lateral point in the lesser wing of the contralateral sphenoid bone. Courtesy of the Rhoton Collection, American Association of Neurological Surgeons/Neurosurgical Research and Education Foundation.
Angular exposure
The angles of approach in the vertical and horizontal planes were utilized to assess angular exposure. The angular exposure area was determined for the six most relevant structures in vascular neurosurgery, including (1) ipsilateral MCA bifurcation; (2) ipsilateral internal carotid artery (ICA) bifurcation; (3) apex of the basilar artery (BA); (4) midpoint of the anterior communicating artery; (5) contralateral carotid bifurcation; and (6) most distal point of the contralateral MCA. Angular exposure was attained by calculating the relationship of these structures with the boundaries of the craniotomy along the horizontal and vertical axes, as defined by the neuronavigation mapping system. The horizontal axis is parallel to the skull base, and the vertical axis is perpendicular to the horizontal axis.
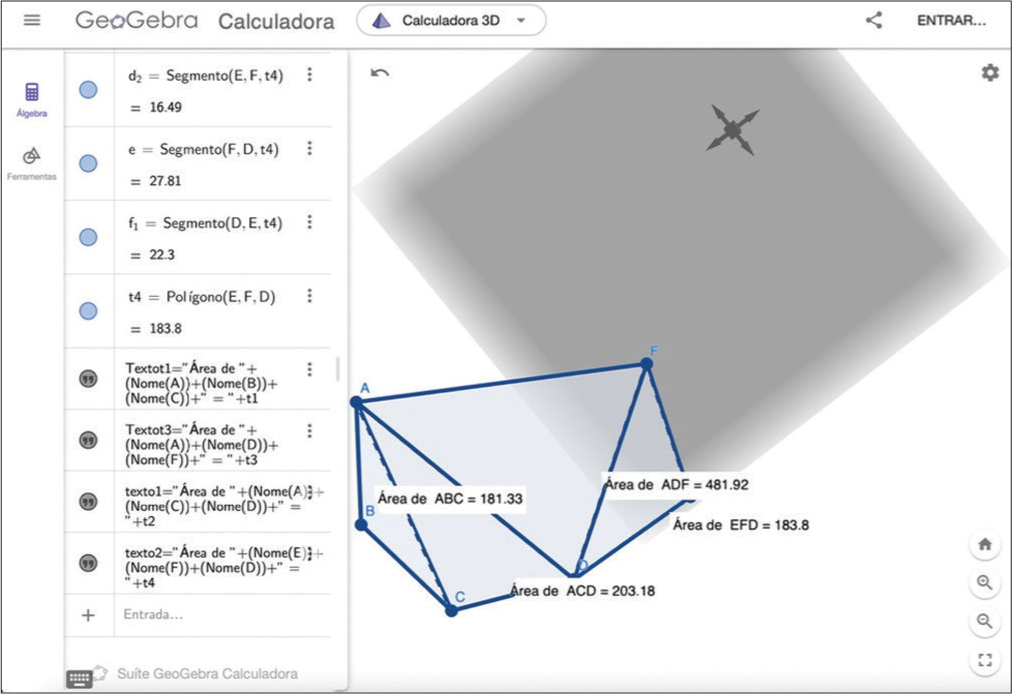
After acquiring values for each predetermined point of interest, a 3D spatial calculator (GeoGebra) was employed to compute areas and obtain data on surgical exposure, craniotomy area, and angular exposure [
Statistical analysis
The data were analyzed as two different groups, LSO and MP. For descriptive purposes, the data were presented as means and standard deviations. Statistically relevant results were analyzed using parametric tests (Student t-test). P < 0.05 was considered significant. All tests were calculated using the software Prism 10 (Macbook- Osx).
RESULTS
Area of exposure
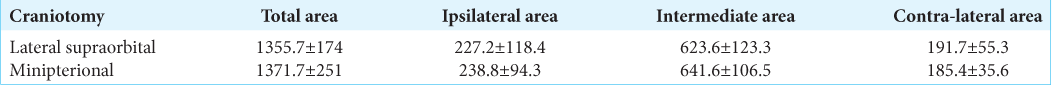
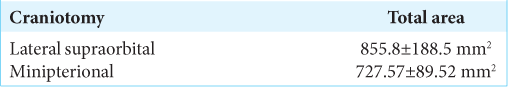
The total surface area of surgical exposure for LSO craniotomy was 1355.70 ± 174 mm2 and 1371.70 ± 251 mm2 for MP (P > 0.05). The results for ipsilateral areas were 227.2 ± 118.40 mm2 for LSO craniotomy and 238.80 ± 94.3 mm2 for MP (P > 0.05). Contralateral areas were 191.70 ± 55.3 mm2 for LSO and 185.4 ± 35.6 mm2 for MP (P > 0.05). Intermediate areas were 623.60 ± 123.30 mm2 for LSO and 641.60 ± 106.50 mm2 for MP craniotomy (P > 0.05). The results are presented in
Horizontal angle of exposure
The angles for the ipsilateral MCA bifurcation were 40.47 ± 7.37° for LSO craniotomy and 47.28 ± 7.29° for MP (P > 0.05); for the ICA bifurcation, they were 41.64 ± 5.92 for LSO and 38.36 ± 3.79 for MP (P > 0.05); for the apex of the BA, they were 33.76 ± 2.59° for LSO and 30.64 ± 3.21° for MP (P > 0.05); for the midpoint of the anterior communicating artery, they were 37.58 ± 2.75° for LSO and 33.85 ± 2.35 for MP (P = 0.0019); for the contralateral ICA, they were 35.52 ± 3.30 for LSO craniotomy and 30.60 ± 2.86 for MP craniotomy (P = 0.0014); and for the contralateral MCA bifurcation, they were 30.58 ± 3.98° for LSO craniotomy and 27.10 ± 3.20 for MP (P > 0.05). The results are summarized in
Vertical angle of exposure
The angles for the ipsilateral MCA bifurcation were 35.18 ± 7.96° for LSO craniotomy and 47.51 ± 9.91 for MP (P = 0.0156); for the ICA bifurcation, they were 31.96 ± 2.67 for LSO and 38.92 ± 5.15 for MP (P > 0.05); for the apex of the BA, they were 25.60 ± 2.30 for LSO and 28.86 ± 1.75 for MP (P = 0.0085); for the midpoint of the anterior communicating artery, they were 28.31 ± 2.61 for LSO and 30.03 ± 3.66 for MP (P > 0.05); for the contralateral ICA, they were 25.77 ± 3.37 for LSO craniotomy and 26.61 ± 4.08 for MP craniotomy (P > 0.05); and for the contralateral MCA, they were 22.50 ± 2.50 for LSO craniotomy and 23.62 ± 3.39 for MP (P > 0.05). The results are summarized in
DISCUSSION
Advancements in microneurosurgery and technology have revolutionized our ability to adopt less invasive techniques, significantly enhancing our surgical capabilities. In both vascular and skull base surgery, the core principles emphasize strategic bone removal to optimize operative exposure while minimizing brain retraction.[
Conventionally, the PT craniotomy has been considered the gold standard approach for addressing tumor and vascular pathologies. However, its extensive drilling, potential for esthetic deformity, patient dissatisfaction, and risk of facial nerve damage have prompted a shift toward alternative approaches.[
The minimally invasive approaches discussed herein provide access to a range of pathologies in the anterior segment of the circle of Willis, Sylvian fissure, and the interpeduncular fossa. These approaches boast several advantages over the standard PT craniotomy, including fast craniotomies, minimized trauma, heightened safety for the facial nerve, favorable cosmetic results, preservation of muscle function, and improved pain management.[
While several clinical series have demonstrated the feasibility of these minimally invasive approaches, there remains a scarcity of objective quantitative data comparing the working space between the LSO and MP approaches. Further, research in this area is essential to understand the comparative benefits and limitations of each technique.
No statistically significant variances were detected in the surgical exposure areas among the assessed approaches in this study. The anatomical exposure remained consistent irrespective of the extent of the craniotomy performed. It appears that bone removal primarily amplifies the working angles accessible to the surgeon rather than directly expanding the surgical exposure area. Interestingly, a similar extent of visualization and dissection of the subarachnoid space was achieved regardless of the chosen technique.
Notably, the dissection of the Sylvian fissure, whether on the same side or opposite side, could be accomplished to a comparable degree in both approaches.
In contrast to the area, angular exposure is enhanced by working within the superficial portion of the craniotomy, achieved through bone removal. Wider angles facilitate multidirectional maneuverability and provide a more accommodating surgical pathway, thereby reducing the necessity for brain retraction. Our findings indicate a statistically significant discrepancy between the horizontal angles at the ipsilateral MCA bifurcation and the apex of the BA. The MP approach offers a superior horizontal working angle compared to the LSO craniotomy.
Similarly, a statistically significant distinction was noted in the vertical angles between the midpoint of the anterior communicating artery and the contralateral ICA. The LSO approach yields a superior vertical working angle compared to the MP craniotomy. Such angular disparities are achieved through bone drilling, emphasizing the tradeoff involved.
Our findings are corroborated by previous anatomical studies[
A thorough comprehension of the anatomical exposure associated with a particular neurosurgical approach can improve the decision-making process when choosing the appropriate approach. Moreover, tailored techniques exist for both approaches, enabling enhanced local exposure when addressing specific areas. Ultimately, the selection of approach should be guided by the pathology and treatment objectives tailored to the patient’s needs.
Finally, both the LSO and MP approaches can be adapted based on the characteristics of the lesion, enabling a lesion-specific surgical strategy rather than employing traditional techniques for various lesions.
Limitations
In this study, cadavers were utilized, acknowledging inherent limitations regarding retraction or structural shrinkage despite efforts to maintain consistency in these variables. Specifically, our investigation employed fresh cadavers, recognized as a more dependable model for anatomical studies. Tissue properties such as consistency and resistance persist even hours after death, providing a more accurate representation of living patient anatomy.
This study primarily focuses on anatomical aspects to refine microsurgical techniques. It’s important to note that we could not replicate clinical risks inherent in actual surgical situations, such as bleeding, brain edema, intracranial lesions, temporal contusion, and postoperative cosmetic outcomes for each craniotomy.
CONCLUSION
Our study offers an objective anatomical analysis comparing the LSO and MP approaches by quantifying morphometric parameters for specific targets. The LSO craniotomy offers comparable anatomical exposure to that provided by the MP craniotomy. It provides good maneuverability to lesions in the anterior communicating artery complex and contralateral ICA. However, it features a narrower surgical corridor to the interpeduncular fossa and the MCA and Sylvian fissure, while the MP craniotomy offers superior visibility and maneuverability for lesions in the interpeduncular area and ipsilateral MCA aneurysms.
Ethical approval
The research/study approved by the Institutional Review Board at Universidade de Sao Paulo, number 4640664, dated September 04, 2021.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. . Available from: https://wfns.org/wfnsdata/document/clinicalresources/helsinki.pdf [Last accessed on 2024 Mar 16].
2. Caplan JM, Papadimitriou K, Yang W, Colby GP, Coon AL, Olivi A. The minipterional craniotomy for anterior circulation aneurysms: Initial experience with 72 patients. Neurosurgery. 2014. 10: 200-6 discussion 206-7
3. Choque-Velasquez J, Hernesniemi J. One burr-hole craniotomy: Lateral supraorbital approach in Helsinki neurosurgery. Surg Neurol Int. 2018. 9: 156
4. Figueiredo EG, Deshmukh P, Nakaji P, Crusius MU, Crawford N, Spetzler RF. The minipterional craniotomy: Technical description and anatomic assessment. Neurosurgery. 2007. 61: 256-64 discussion 264-5
5. Figueiredo EG, Deshmukh P, Zabramski JM, Preul MC, Crawford NR, Siwanuwatn R. Quantitative anatomic study of three surgical approaches to the anterior communicating artery complex. Neurosurgery. 2005. 56: 397-405 discussion 397-405
6. Figueiredo EG, Deshmukh P, Zabramski JM, Preul MC, Crawford NR, Spetzler RF. The pterional-transsylvian approach: An analytical study. Neurosurgery. 2008. 62: 1361-7
7. Figueiredo EG, Deshmukh V, Nakaji P, Deshmukh P, Crusius MU, Crawford N. An anatomical evaluation of the mini-supraorbital approach and comparison with standard craniotomies. Neurosurgery. 2006. 59: ONS212-20 discussion ONS220
8. Figueiredo EG, Gomes M, Vellutini E, Rosemberg S, Marino R. Angioleiomyoma of the cavernous sinus: Case report. Neurosurgery. 2005. 56: E411
9. Figueiredo EG, Teixeira MJ, Spetzler RF, Preul MC. Clinical and surgical experience with the minipterional craniotomy. Neurosurgery. 2014. 75: E324-5
10. Figueiredo EG, Welling LC, Preul MC, Sakaya GR, Neville I, Spetzler RF. Surgical experience of minipterional craniotomy with 102 ruptured and unruptured anterior circulation aneurysms. J Clin Neurosci. 2016. 27: 34-9
11. Hernesniemi J, Ishii K, Niemelä M, Smrcka M, Kivipelto L, Fujiki M. Lateral supraorbital approach as an alternative to the classical pterional approach. Acta Neurochir Suppl. 2005. 94: 17-21
12. Im SH, Song J, Park SK, Rha EY, Han YM. Cosmetic reconstruction of frontotemporal depression using polyethylene implant after pterional craniotomy. Biomed Res Int. 2018. 2018: 1982726
13. Lee MS, Lee YS, Lee JH, Ryu KY, Kang DG. The efficacy of temporal mesh plate floating technique for keyhole site depression after frontotemporal craniotomy. J Korean Neurotraumatol Soc. 2011. 7: 78-82
14. Martínez-Pérez R, Albonette-Felicio T, Hardesty DA, Prevedello DM. Comparative anatomical analysis between the minipterional and supraorbital approaches. J Neurosurg. 2020. 134: 1276-84
15. Park HH, Sung KS, Moon JH, Kim EH, Kim SH, Lee KS. Lateral supraorbital versus pterional approach for parachiasmal meningiomas: Surgical indications and esthetic benefits. Neurosurg Rev. 2020. 43: 313-22
16. Raygor KP, Garcia J, Rutledge C, Tonetti DA, Raper DM, Abla AA. The lateral supraorbital craniotomy approach for anterior circulation aneurysms: A modern surgical case series in the endovascular era. World Neurosurg. 2022. 166: e799-807
17. Reisch R, Perneczky A. Ten-year experience with the supraorbital subfrontal approach through an eyebrow skin incision. Neurosurgery. 2005. 57: 242-55 discussion 242-55
18. Sturiale CL, La Rocca G, Puca A, Fernandez E, Visocchi M, Marchese E. Minipterional craniotomy for treatment of unruptured middle cerebral artery aneurysms. A single-center comparative analysis with standard pterional approach as regard to safety and efficacy of aneurysm clipping and the advantages of reconstruction. Acta Neurochir Suppl. 2017. 124: 93-100
19. Van Lindert E, Perneczky A, Fries G, Pierangeli E. The supraorbital keyhole approach to supratentorial aneurysms: Concept and technique. Surg Neurol. 1998. 49: 481-9 discussion 489-90
20. Vishteh AG, Marciano FF, David CA, Baskin JJ, Spetzler RF. The pterional approach. Oper Tech Neurosurg. 1998. 1: 39-49
21. Yagmurlu K, Safavi-Abbasi S, Belykh E, Kalani MY, Nakaji P, Rhoton AL. Quantitative anatomical analysis and clinical experience with mini-pterional and mini-orbitozygomatic approaches for intracranial aneurysm surgery. J Neurosurg. 2017. 127: 646-59
22. Yasargil MG, Fox JL. The microsurgical approach to intracranial aneurysms. Surg Neurol. 1975. 3: 7-14








Ismail Akkol
Posted September 13, 2024, 1:47 pm
nice manuscript. tnx.
by mistake;
in figure 2 /a : R ICA is Left ICA
in figure 2/b : Rights will be Left…
with respect