- Department of Neurological Surgery, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, USA
Correspondence Address:
Raymond F. Sekula
Department of Neurological Surgery, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania, USA
DOI:10.4103/2152-7806.194145
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Seyed H. Mousavi, Raymond F. Sekula, Ariel Gildengers, Paul Gardner, L. Dade Lunsford. Concomitant depression and anxiety negatively affect pain outcomes in surgically managed young patients with trigeminal neuralgia: Long-term clinical outcome. 15-Nov-2016;7:98
How to cite this URL: Seyed H. Mousavi, Raymond F. Sekula, Ariel Gildengers, Paul Gardner, L. Dade Lunsford. Concomitant depression and anxiety negatively affect pain outcomes in surgically managed young patients with trigeminal neuralgia: Long-term clinical outcome. 15-Nov-2016;7:98. Available from: http://surgicalneurologyint.com/surgicalint_articles/concomitant-depression-anxiety-negatively-affect-pain-outcomes-surgically-managed-young-patients-trigeminal-neuralgia-long%e2%80%91term-clinical-outcome/
Abstract
Background:Onset of trigeminal neuralgia (TN) is uncommon in young adults with less favorable benefit from surgical interventions. The aim of this study was to evaluate the role of concomitant psychosomatic disorders in long-term surgical outcomes in this population.
Methods:Twenty-one patients younger than 30 years of age were diagnosed initially as having medically refractory TN, and each patient underwent microvascular decompression (MVD) as initial surgical management. Correlation of clinical outcome and psychosomatic disorders (DSM-IV) was evaluated during a 15-year interval.
Results:A total of 93 procedures were performed for the management of TN and subsequent iatrogenic craniofacial pain disorders. At a median of 81 months, 8 of 21 patients were free of facial pain. Fourteen patients with concomitant major depressive disorder (MDD) or other anxiety disorders underwent a higher median of procedures compared with 7 patients without known MDD or anxiety (4.5 versus 1 intervention, P = 0.038). Two of 14 patients who were diagnosed with MDD or other anxiety disorders were free of craniofacial pain, whereas 6 of 7 patients without mood or anxiety disorders were free of craniofacial pain (P = 0.0005). Thirteen patients developed treatment-related complications that required further surgical procedures. Presence of MDD or other anxiety disorders was associated with higher rate of complications (P = 0.026). One patient with past medical history of severe anxiety died of unknown causes.
Conclusions:In young patients with TN, comorbid MDD or anxiety disorders was associated with seeking multiple invasive procedures in multiple academic centers with limited benefit and high rates of surgical induced complications.
Keywords: Anxiety, depression, surgical intervention, trigeminal neuralgia
INTRODUCTION
The incidence of trigeminal neuralgia (TN) increases with age, peaking by the 5th and 6th decades of life. However, a small incidence of TN occurs in the younger population as well.[
MATERIALS AND METHODS
Study population
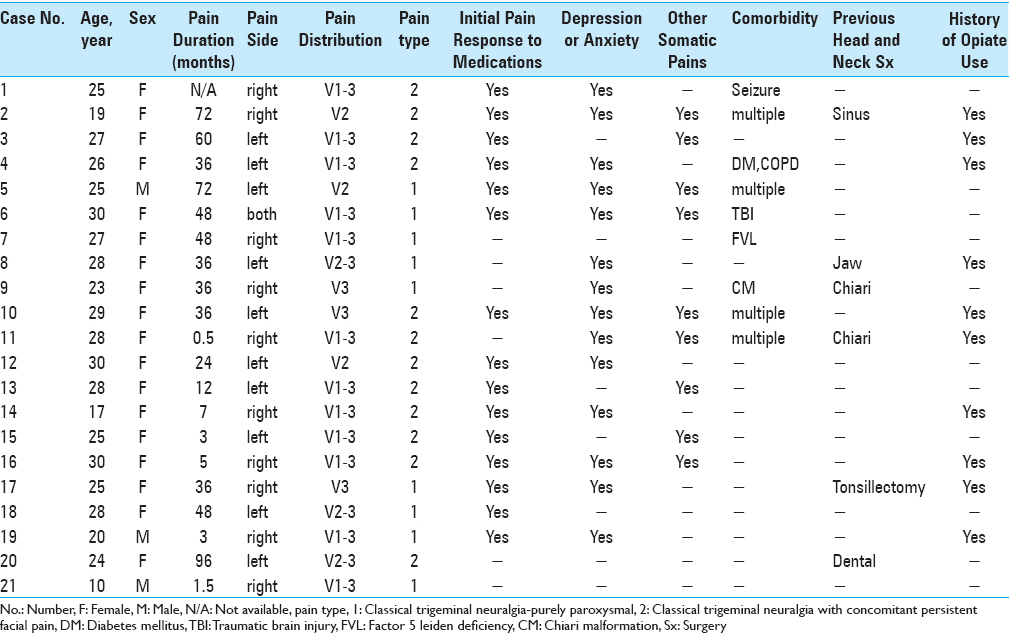
This study was conducted with the approval of the University of Pittsburgh Institutional Review Board. We retrospectively identified 25 medically refractory idiopathic TN patients, younger than 30 years of age, all of whom underwent initial MVD between January 2000 and December 2014. Four patients were lost to follow-up and 21 patients enrolled in study. No patient had an identified structural or demyelinating lesion as a cause of TN. Sixteen patients had at least some initial pain relief with medications. Four patients had poor response to medication, and one patient could not tolerate the side effects of medications. TN was categorized using Burchiel classification.[
Surgical technique
MVD was performed using the standard approach as described previously.[
Follow-up and data collection
The patient medical records were reviewed and pertinent information was recorded. Patients were contacted by telephone for additional information by two authors (SHM/BA) who did not provide patient care to any of the patients included. The results were analyzed in order to determine the clinical outcomes in this population following therapeutic interventions. Patients’ psychological history was reviewed retrospectively from medical records or contacting patients. Patients were specifically asked whether they underwent additional surgical procedures in other centers during the course of their pain history. Diagnosis of psychological disorder was made based on DSM-IV-TR criteria.[
RESULTS
Surgical approaches and clinical outcome
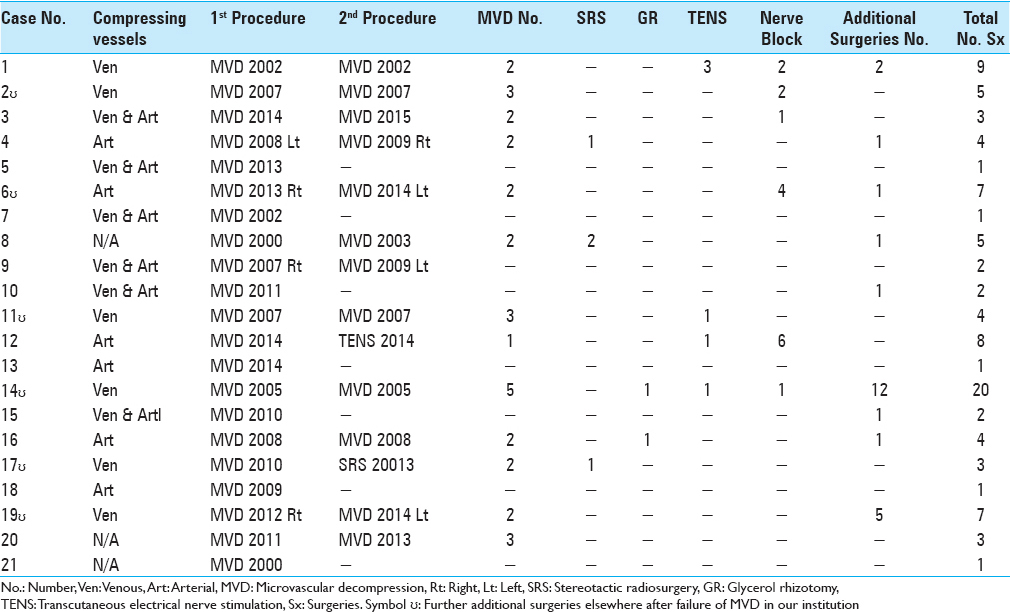
Patients in this series had a median of 3 procedures for the management of TN. For management of TN and surgically induced complications, 21 patients underwent 93 procedures. Four patients each had an additional MVD for TN onset on the contralateral side (three onsets of which developed post-initial ipsilateral MVD). Nine patients developed ipsilateral occipital neuralgia after MVD and underwent additional surgical interventions or nerve block. Patients’ operative procedures are shown in
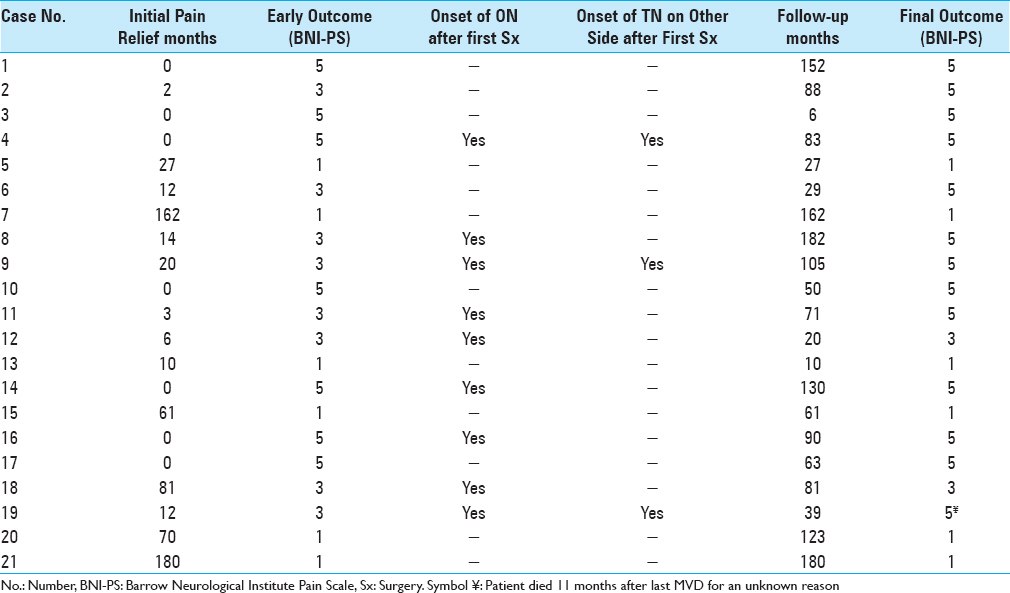
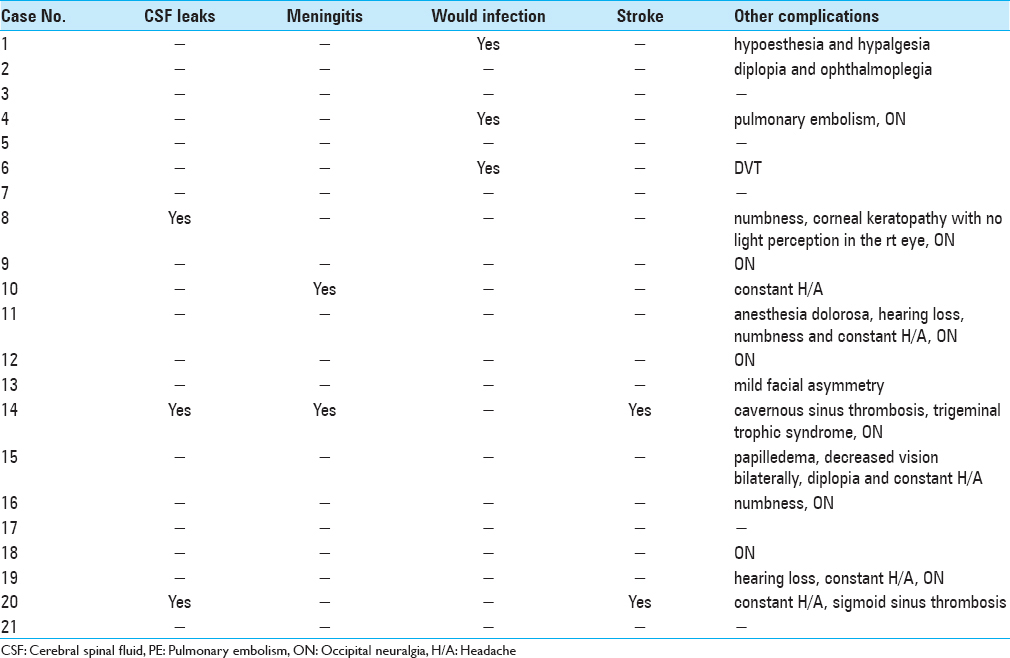
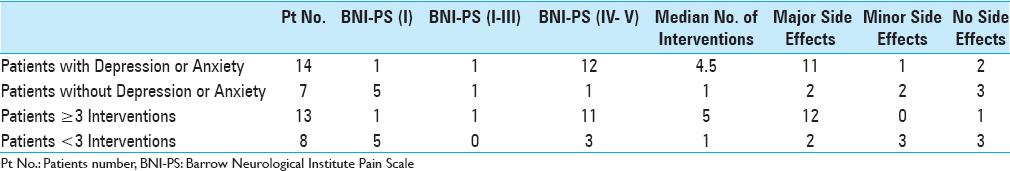
Fourteen patients initially responded to MVD with a median of 17 months of pain relief. Among the 14 patients with initial pain relief, 9 patients underwent additional interventions for management of pain recurrence, which was successful in 3 patients. At a median of 81-months follow-up, 8 patients were pain free. Thirteen patients suffered from side effects to interventions. While 2 patients had to leave college, another 4 had to stop their occupations due to intolerable pain. Furthermore, one patient was found dead in his apartment for an undisclosed reason 11 months after his last MVD. There were no statistically significance correlations between patients’ pain type, number of surgical interventions, and pain outcomes. Surgical outcomes and complications of patients are presented in Tables
Effect of additional depression and anxiety disorders in pain control
Reviewing the medical records, aside from facial pain, 17 patients were diagnosed with additional major depressive disorder (MDD), anxiety disorders, or somatic pain disorders (DSM IV-TR). Nine patients had concomitant MDD, of which 7 were on antidepressant medications. Eleven patients had other anxiety disorders, of which 8 were on antianxiety medications. Four patients were diagnosed with fibromyalgia, and 3 patients reported severe migraine prior to initial surgery.
Patients with concomitant MDD and GAD underwent a median of 4.5 versus 1 invasive intervention for patients without comorbid psychiatric disorder (P = 0.038, Fisher's exact test). TN was relieved with and without medication in only 2 of the 14 patients with such disorders; however, in 6 out of the 7 patients without known MDD or GAD, TN was relieved with or without medication (P = 0.0005, Fisher's exact test). Presence of depression or other anxiety disorders was also associated with higher rate of surgical induced complications (P = 0.026, Fisher's exact test). Pain intensity score in relation to number of therapeutic interventions in association with other somatic pain syndromes, MDD, GAD, and complications are summarized in
DISCUSSION
This report provides additional evidence that MVD and further surgical procedures failed to provide pain relief in a majority of younger patients diagnosed with TN. Similar results have been reported elsewhere.[
In 1947 and 1951, McElin and Horton followed by Engel, respectively, suggested that atypical facial pain was a secondary manifestation of primary psychiatric disturbances in two separate studies.[
The exacerbatory effects of depression on the severity of painful stimuli may be of particular importance for patients with TN.[
Study limitations
While our results demonstrate an important concept in the management of young patients with TN, this study did not have a nonintervention control group. However, the absence of a nonintervention control group was unavoidable due to ethical considerations. More important, because our study was cross-sectional and our analyses correlational, we cannot address causality, whether MDD or GAD onset occurred before, after, or concurrently with TN onset in our patient population. In addition, our patients’ population due to rare incidence of TN in young individuals was small. Furthermore, due to separation of two primary surgeons from the University, it is not clear whether some of these patients were misdiagnosed with TN, while they might have actually suffered from atypical facial pain.
CONCLUSION
Our results suggest that in the presence of MDD and anxiety disorders younger patients with TN seek multiple invasive procedures in different institutions with limited benefit. Therefore, management of these patients should include an initial psychiatric evaluation and appropriate treatment, if needed, before initial surgery is recommended.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. .editorsAmerican Psychiatric Association, American Psychiatric Association. Task Force on DSM-IV. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, DC: American Psychiatric Association; 2000. p.
2. Bahgat D, Ray DK, Raslan AM, McCartney S, Burchiel KJ. Trigeminal neuralgia in young adults. J Neurosurg. 2011. 114: 1306-11
3. Barker FG, Jannetta PJ, Bissonette DJ, Larkins MV, Jho HD. The long-term outcome of microvascular decompression for trigeminal neuralgia. N Engl J Med. 1996. 334: 1077-83
4. Betrus PA, Elmore SK, Hamilton PA. Women and somatization: Unrecognized depression. Health Care Women Int. 1995. 16: 287-97
5. Broggi G, Ferroli P, Franzini A, Servello D, Dones I. Microvascular decompression for trigeminal neuralgia: Comments on a series of 250 cases, including 10 patients with multiple sclerosis. J Neurol Neurosurg Psychiatry. 2000. 68: 59-64
6. Burchiel KJ. A new classification for facial pain. Neurosurgery. 2003. 53: 1164-6
7. Burton AK, Tillotson KM, Main CJ, Hollis S. Psychosocial predictors of outcome in acute and subchronic low back trouble. Spine. 1995. 20: 722-8
8. Engel GL. Primary atypical facial neuralgia; an hysterical conversion symptom. Psychosom Med. 1951. 13: 375-96
9. Feinmann C, Harris M, Cawley R. Psychogenic facial pain: Presentation and treatment. Br Med J. 1984. 288: 436-8
10. First MB. Diagnostic and statistical manual of mental disorders, 5 th edition, and clinical utility. J Nerv Ment Dis. 2013. 201: 727-9
11. Gureje O, Simon GE, Von Korff M. A cross-national study of the course of persistent pain in primary care. Pain. 2001. 92: 195-200
12. Holroyd KA, Stensland M, Lipchik GL, Hill KR, O’Donnell FS, Cordingley G. Psychosocial correlates and impact of chronic tension-type headaches. Headache. 2000. 40: 3-16
13. Janjigian ER. Report of three cases of trigeminal neuralgia apparently cured by electroshock therapy. Am J Psychiatry. 1949. 106: 143-
14. Jollant F, Bellivier F, Leboyer M, Astruc B, Torres S, Verdier R. Impaired decision making in suicide attempters. Am J Psychiatry. 2005. 162: 304-10
15. Katon W, Ries RK, Kleinman A. A prospective DSM-III study of 100 consecutive somatization patients. Compr Psychiatry. 1984. 25: 305-14
16. Lamb SE, Guralnik JM, Buchner DM, Ferrucci LM, Hochberg MC, Simonsick EM. Factors that modify the association between knee pain and mobility limitation in older women: The Women's Health and Aging Study. Ann Rheum Dis. 2000. 59: 331-7
17. Lascelles RG. Atypical facial pain and depression. Br J Psychiatry. 1966. 112: 651-9
18. Leino P, Magni G. Depressive and distress symptoms as predictors of low back pain, neck-shoulder pain, and other musculoskeletal morbidity: A 10-year follow-up of metal industry employees. Pain. 1993. 53: 89-94
19. Lunsford LD. Treatment of tic douloureux by percutaneous retrogasserian glycerol injection. JAMA. 1982. 248: 449-53
20. Mc ET, Horton BT. Atypical face pain; a statistical consideration of 66 cases. Ann Intern Med. 1947. 27: 749-68
21. Mousavi SH, Niranjan A, Huang MJ, Laghari FJ, Shin SS, Mindlin JL. Early radiosurgery provides superior pain relief for trigeminal neuralgia patients. Neurology. 2015. 85: 2159-65
22. Mullan S, Lichtor T. Percutaneous microcompression of the trigeminal ganglion for trigeminal neuralgia. J Neurosurg. 1983. 59: 1007-12
23. Rainville P, Duncan GH, Price DD, Carrier B, Bushnell MC. Pain affect encoded in human anterior cingulate but not somatosensory cortex. Science. 1997. 277: 968-71
24. Resnick DK, Levy EI, Jannetta PJ. Microvascular decompression for pediatric onset trigeminal neuralgia. Neurosurgery. 1998. 43: 804-7
25. Sekula RF, Marchan EM, Fletcher LH, Casey KF, Jannetta PJ. Microvascular decompression for trigeminal neuralgia in elderly patients. J Neurosurg. 2008. 108: 689-91
26. Simon GE, VonKorff M, Piccinelli M, Fullerton C, Ormel J. An international study of the relation between somatic symptoms and depression. N Engl J Med. 1999. 341: 1329-35
27. Sweet WH. Controlled thermocoagulation of trigeminal ganglion and rootlets for differential destruction of pain fibers: Facial pain other than trigeminal neuralgia. Clin Neurosurg. 1976. 23: 96-102
28. Taenzer P, Melzack R, Jeans ME. Influence of psychological factors on postoperative pain, mood and analgesic requirements. Pain. 1986. 24: 331-42
29. Terry EL, DelVentura JL, Bartley EJ, Vincent AL, Rhudy JL. Emotional modulation of pain and spinal nociception in persons with major depressive disorder (MDD). Pain. 2013. 154: 2759-68
30. Verdejo-Garcia A, Lopez-Torrecillas F, Calandre EP, Delgado-Rodriguez A, Bechara A. Executive function and decision-making in women with fibromyalgia. Arch Clin Neuropsychol. 2009. 24: 113-22
31. Von Korff M, Le Resche L, Dworkin SF. First onset of common pain symptoms: A prospective study of depression as a risk factor. Pain. 1993. 55: 251-8
32. Wells KB, Golding JM, Burnam MA. Affective, substance use, and anxiety disorders in persons with arthritis, diabetes, heart disease, high blood pressure, or chronic lung conditions. Gen Hosp Psychiatry. 1989. 11: 320-7
33. Wilson DR, Widmer RB, Cadoret RJ, Judiesch K. Somatic symptoms. A major feature of depression in a family practice. J Affect Disord. 1983. 5: 199-207
34. Wu TH, Hu LY, Lu T, Chen PM, Chen HJ, Shen CC. Risk of psychiatric disorders following trigeminal neuralgia: A nationwide population-based retrospective cohort study. J Headache Pain. 2015. 16: 64-
35. Zakrzewska JM, Linskey ME. Trigeminal neuralgia. BMJ. 2015. 350: h1238-