Conjoined nerve root, epidural varicose vein, and extruded lumbar disc: Triad of refractory sciatica
- Department of Neurosurgery, Ibrahim Cardiac Hospital and Research Institute (A Centre for Cardiovascular, Neuroscience and Organ Transplant Units), Dhaka, Bangladesh
- Department of Orthopedic Surgery, Bangladesh Medical University, Dhaka, Bangladesh
Correspondence Address:
Nazmin Ahmed, Assistant Professor and Associate Consultant, Department of Neurosurgery, Ibrahim Cardiac Hospital and Research Institute (A Centre for Cardiovascular, Neuroscience and Organ Transplant Units), Dhaka, Bangladesh.
DOI:10.25259/SNI_371_2025
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nazmin Ahmed1, Mohammad Nazrul Hossain1, Shahidul Islam Khan2, Raad Kazi1. Conjoined nerve root, epidural varicose vein, and extruded lumbar disc: Triad of refractory sciatica. 23-May-2025;16:200
How to cite this URL: Nazmin Ahmed1, Mohammad Nazrul Hossain1, Shahidul Islam Khan2, Raad Kazi1. Conjoined nerve root, epidural varicose vein, and extruded lumbar disc: Triad of refractory sciatica. 23-May-2025;16:200. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13570
Abstract
Background: A patient presented with sciatica attributed to a conjoined lumbosacral nerve root, an extruded disc herniation, and epidural varicose veins.
Case Description: A 60-year-old male presented with 5 months of sciatica (4/5 motor deficit). The lumbosacral magnetic resonance showed a right paracentral disc herniation causing thecal sac/L5-S1 nerve root compression. Intraoperatively, the patient had an L5-S1 conjoined nerve root, an extruded disc herniation, and type C epidural varicose veins. A wide fenestration and foraminotomy were performed to facilitate the removal of the extruded disc and partial coagulation of the epidural varicose veins. Surgery resulted in complete symptom resolution within the 1st postoperative month.
Conclusion: A patient with intractable right-sided sciatic was found at surgery to have an L5-S1 conjoined nerve root, a herniated disc, and marked epidural varicosities. Following a wide fenestration/foraminal decompression, the patient’s symptoms fully resolved within the 1st postoperative month.
Keywords: Conjoined nerve root, Epidural varicose vein, Extruded disc
INTRODUCTION
Conjoined nerve root and epidural varicose vein can mimic disc herniation both clinically and radiologically which possesses a diagnostic and management challenge to a Spine surgeon. Therefore, a detail neurological examination and correlation with neuroimaging feature plays a pivotal role to choose appropriate management strategy. Herein, this is the world’s first reported case of it’s kind with presence of Conjoined lumbosacral nerve root anomalies, accompanied by extruded disc herniation and epidural varicose vein, resulting in refractory lumbago-sciatica. We have highlighted the misleading imaging features and management challenges of this rare entity and briefly reviewed the pertinent literature.
IMAGE REPORT
A 60-year-old male presented with 5 months of sciatica that had exacerbated over the past 2 weeks. On examination, straight leg raising was positive on the right at 40°, and he had 4/5 motor strength in the L5/S1 distributions. The lumbosacral magnetic resonance imaging (MRI) showed a right L5/S1 paracentral disc herniation causing thecal sac/nerve root compression and marked varicosities (i.e. prominent flow voids) [
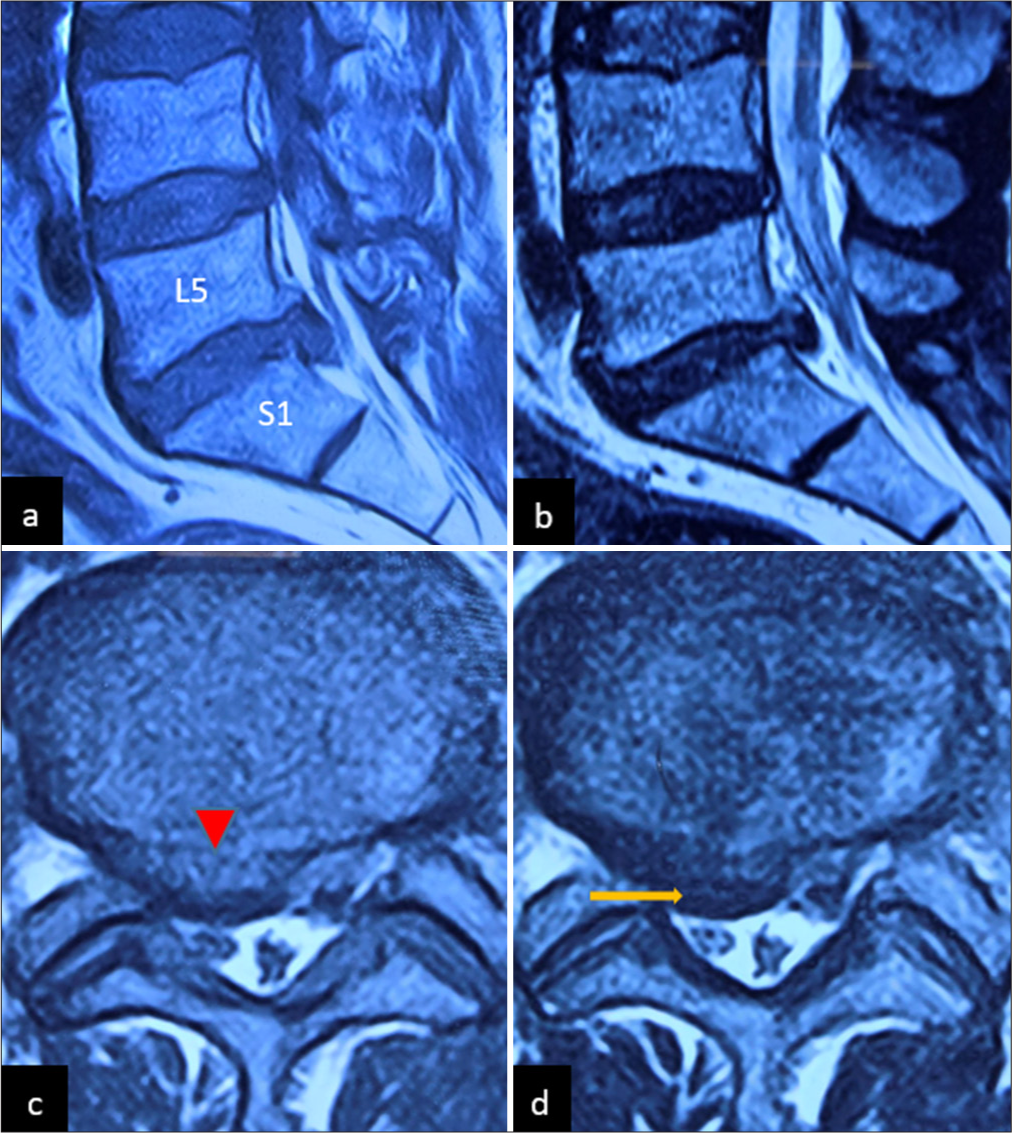
Figure 1:
MRI of L/S spine, (a) T1WI sagittal and (b) T2WI sagittal section demonstrated LDH at L5/S1 level, causing thecal sac indentation and compression of the nerve roots. (c) T1WI axial section showed right paracentral LDH (marked by red arrowhead) with obliteration of lateral recess on both sides. (d) There was the presence of a flow void, capping the herniated disc material (marked by a yellow arrow) with significant displacement of the right exiting nerve root. Here, MRI: Magnetic resonance imaging, T1WI: T1-weighted image, T2WI: T2-weighted image, LDH: Lumbar disc herniation.
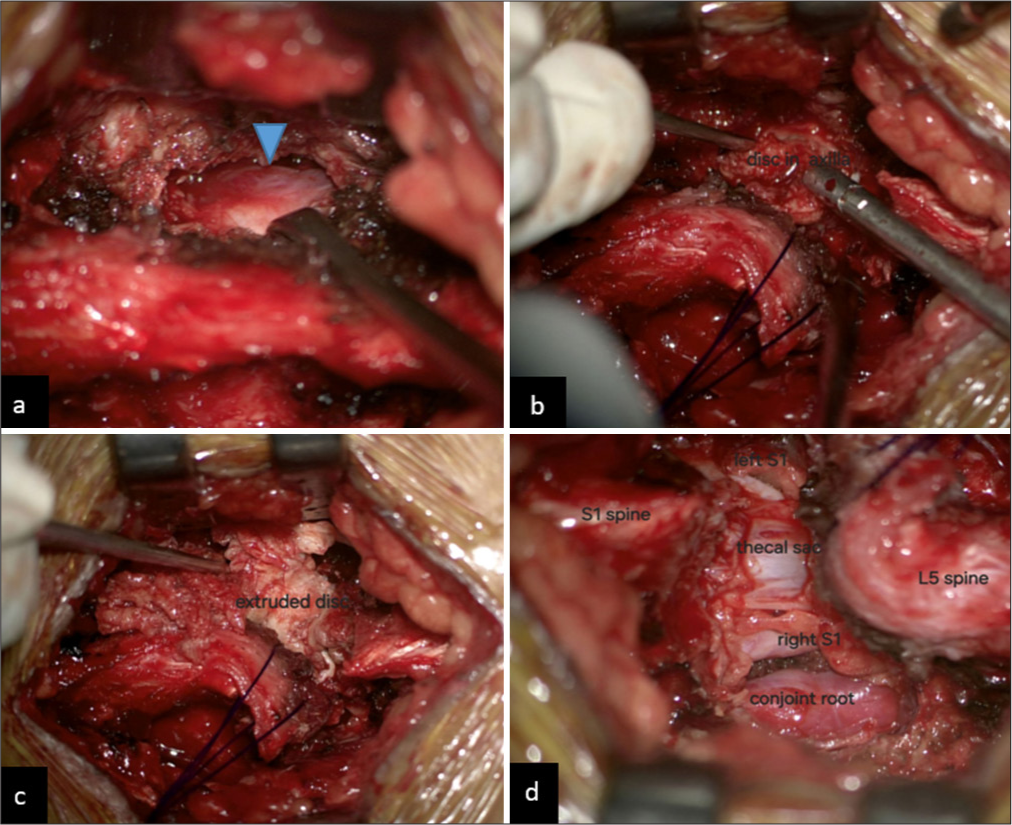
Figure 2:
Intraoperative photograph demonstrated. (a) Type C varicose vein, densely adhered and encircled the exiting nerve root (marked by blue arrowhead). (b) Wide fenestration and cranial mobilization of supraspinous and interspinous ligaments were done to facilitate HD removal. (c) An exceptionally large extruded disc with a downward migratory component removed in between the thecal sac and nerve root axilla. (d) Intraoperative microscopic appearance of the conjoined nerve root, densely adhered with type C varicose vein and thecal sac labeled. Here, HD: Herniated disc.
DISCUSSION
Conjoined nerve roots and epidural varicose veins can both clinically and radiographically mimic lumbar disc herniations.[
CONCLUSION
Meticulous clinico-radiological evaluation is mandatory to predict the radiological mimics of lumbar disc herniation. In the era of minimally invasive spine surgery, microscopic decompression of the neural elements is better to achieve a favourable neurological outcome.
Ethical approval:
Institutional Review Board approval is not required.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship:
Nil.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Kang CH, Shin MJ, Kim SM, Lee SH, Kim HK, Ryu JA. Conjoined lumbosacral nerve roots compromised by disk herniation: Sagittal shoulder sign for the preoperative diagnosis. Skeletal Radiol. 2008. 37: 225-31
2. Raut VK, Khan AH, Ahmad M, Barua S, Ahmed N, Khan SI. Spinal epidural varicosity resembling prolapsed intervertebral disc on MRI: A diagnostic dilemma for lumbar canal stenosis. J Neurol Stroke. 2021. 11: 23-5
3. Trakolis L, Petridis AK. Contralateral discectomy as a novel approach for disc herniation compressing a conjoined nerve root: Illustrative case. J Neurosurg Case Lessons. 2024. 8: CASE24301