- Department of Neurological Surgery, Indiana University School of Medicine, Indianapolis, Indiana, United States.
Correspondence Address:
Laurie L. Ackerman, Department of Neurological Surgery, Indiana University Riley Hospital for Children, 705 Riley Hospital Drive #1601C, Indianapolis, Indiana, United States.
DOI:10.25259/SNI_263_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Josue D. Ordaz, Nicolas W. Villelli, Bradley N. Bohsntedt, Laurie L. Ackerman. Delayed presentation of a traumatic scalp arteriovenous fistula. 25-May-2021;12:238
How to cite this URL: Josue D. Ordaz, Nicolas W. Villelli, Bradley N. Bohsntedt, Laurie L. Ackerman. Delayed presentation of a traumatic scalp arteriovenous fistula. 25-May-2021;12:238. Available from: https://surgicalneurologyint.com/surgicalint-articles/10823/
Abstract
Background: Arteriovenous (AV) fistulas of the scalp are extracranial vascular malformations commonly caused by trauma and typically present within 3 years. Although they follow a benign course, they can be esthetically displeasing.
Case Description: We present an atypical onset of scalp AV fistula in a patient with a 1-year history of the left-sided pulsatile tinnitus and scalp swelling 7 years after a traumatic epidural hematoma evacuation. Our patient was found to have an 8 mm AV fistula supplied by the deep temporal artery. Endovascular embolization was performed using eight coils. There was no complication from the procedure, and the patient’s pulsatile tinnitus and swelling resolved immediately after embolization. Follow-up angiogram demonstrated complete obliteration of the AV fistula.
Conclusion: Delayed presentation of traumatic scalp AV fistula is very rare, and it is important to keep this in the differential in patients with scalp swelling after head trauma.
Keywords: Arteriovenous fistula, Head trauma, Iatrogenic fistula, Neuroendovascular
INTRODUCTION
Subcutaneous scalp arteriovenous (AV) fistulae are uncommon vascular lesions that occur spontaneously, iatrogenically, or following trauma. These lesions typically do not pose life-threatening risks to the patient. However, they can be cosmetically disfiguring and cause significant distress. The common presentations are headache, pulsatile mass, and pulsatile tinnitus.[
CASE PRESENTATION
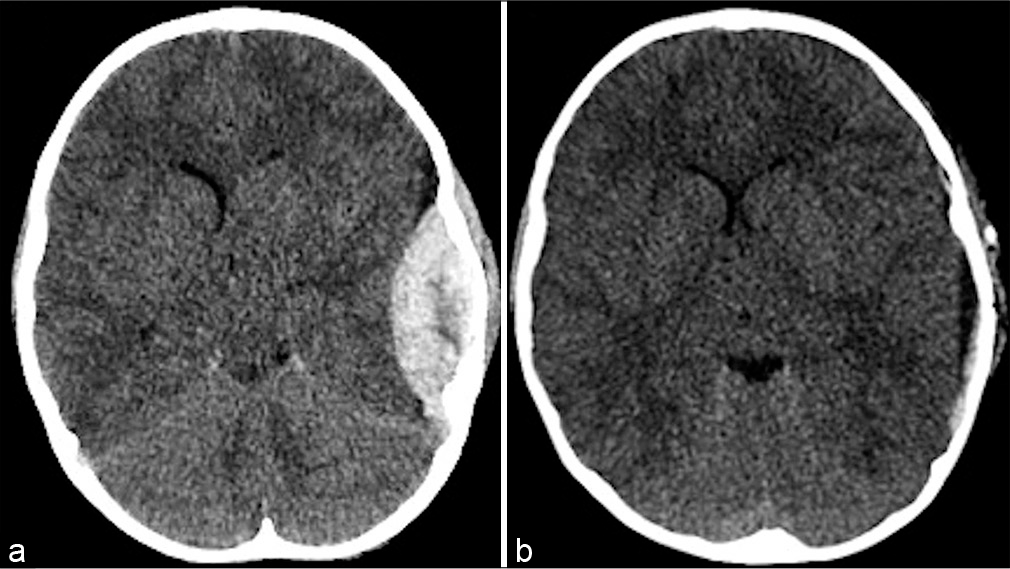
Our patient is a 16-year-old male who presented to the neurosurgery clinic with a 1-year history of progressive left scalp swelling and tinnitus. He had a history of trauma 7 years prior resulting in a left 2.5 cm temporal epidural hematoma [
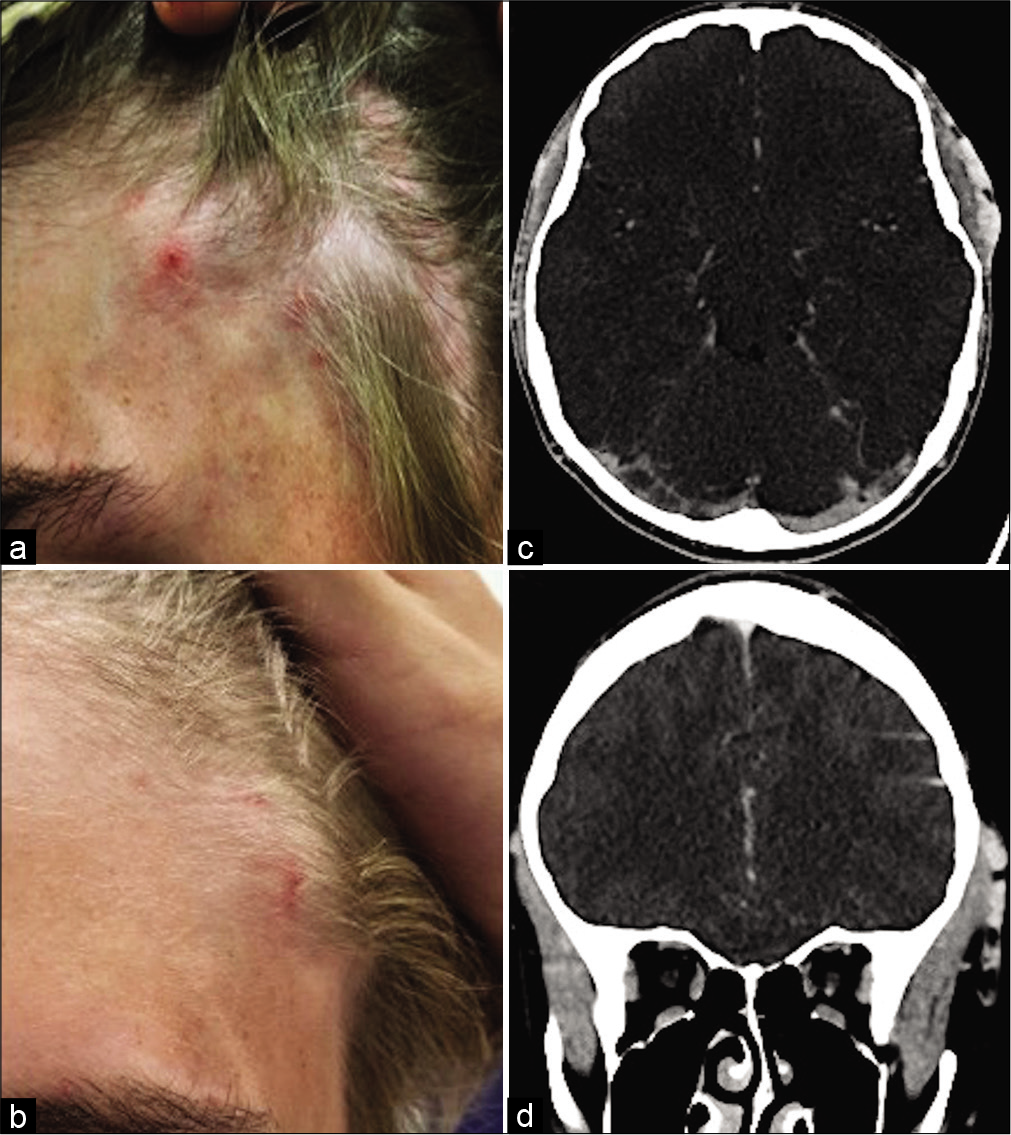
On presentation, our patient had an intact neurological examination including cranial nerve and motor and sensory systems. There was no papilledema. Fullness was noted over the left forehead and temporal area. A tortuous vein was seen over the lateral aspect of the left eyebrow [
A computed tomography angiography (CTA) of the head was obtained that demonstrated numerous dilated scalp veins overlaying the temporalis muscle and extending into the face [
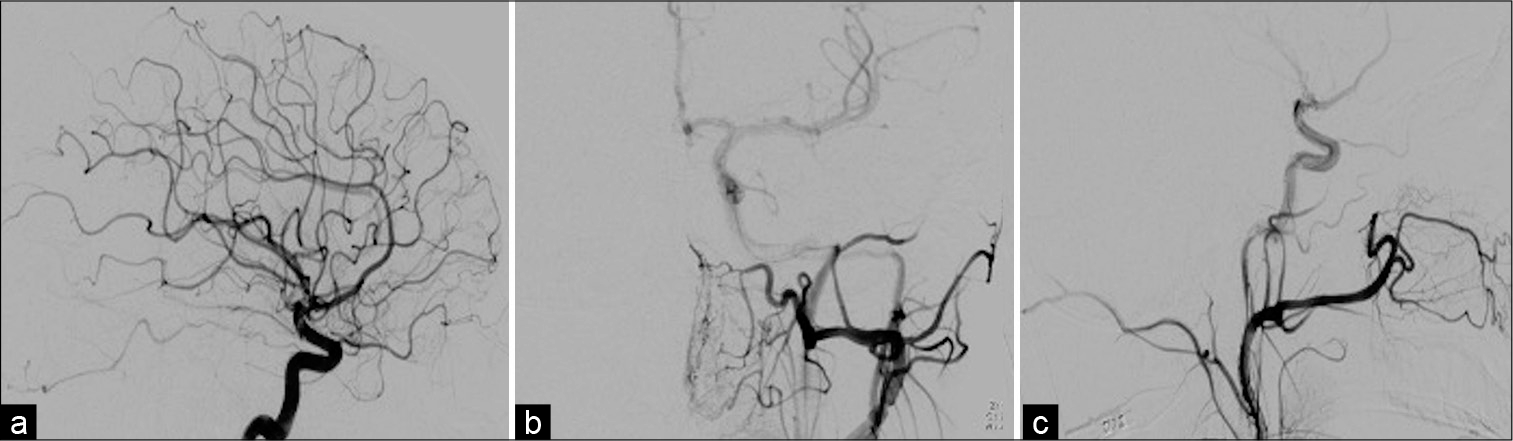
The AV fistula was embolized using a total of eight Penumbra smart coils® (Penumbra, Inc.; Alameda, CA). Four coils were deployed inside of venous pouch. One traveled distally into the venous pouch and three landed proximally. After deployment of these coils, there was good distal occlusion in the venous pouch. The microcatheter was then pulled back slightly until it landed at the fistula site. An additional four coils were deployed at this site. Follow-up angiogram showed no residual filling of the fistula [
The postoperative course was unremarkable without complications from the coil embolization procedure. The engorged facial veins were no longer visible. At 1-month follow-up, the patient denied any tinnitus, headaches, blurry, or double vision. No engorged facial veins were visible at the time. A 6-month postoperative angiogram was performed that demonstrated successful obliteration of the scalp AV fistula [
DISCUSSION
There are two proposed mechanisms for traumatic AV fistulae. The laceration theory describes direct communication of a lacerated artery and venous pouch that developed from the incident.[
Our case presents a unique situation because of the delayed presentation 7 years after initial trauma and prior surgery in the region of the AV fistula. The delay in presentation was likely due to the relatively smaller size of deep temporal arteries compared to the superficial temporal and occipital arteries, which are more common feeders. We predict that this would result in slower reconstruction, enlargement, and development of swelling from the AV fistula.
Diagnostic workup is critical to define the management of AV fistula. Recent systematic reviews have developed diagnostic and treatment algorithms for these vascular pathologies depending on size and arterial feeders.[
We performed endovascular embolization, because surgery carried increased risk for wound healing and infection since there is poorer vascular supply from prior surgery. Paradoxically, other literature reports endovascular treatment carries a higher risk of scalp necrosis.[
CONCLUSION
This report highlights that traumatic scalp AV fistulas may present years after the initial injury, and it is incumbent on the treating physician to include this in the differential diagnosis. Typical presenting symptoms include headache, scalp swelling, pulsatile tinnitus, chemosis, and proptosis. Angiography is the gold standard for diagnoses. Endovascular embolization is a safe and effective treatment of these lesions. We recommend it for small lesions in a previously operated area to reduce wound healing problems. Moreover, deploying the coils or other embolization material at the pathology will reduce the risk of scalp necrosis. One of the limitations of this report is that not all of published case reports/series include the time to onset of symptoms from the inciting event and some report time of symptom duration before presenting for treatment. This could be from limited resources, symptom tolerance, or misdiagnoses.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Berenstein A, Scott J, Choi IS, Persky M. Percutaneous embolization of arteriovenous fistulas of the external carotid artery. AJNR Am J Neuroradiol. 1986. 7: 937-42
2. Fisher-Jeffes ND, Domingo Z, Madden M, de Villiers JC. Arteriovenous malformations of the scalp. Neurosurgery. 1995. 36: 656-60
3. Gurkanlar D, Gonul M, Solmaz I, Gonul E. Cirsoid aneurysms of the scalp. Neurosurg Rev. 2006. 29: 208-12
4. Leke B, Peter R. Traumatic arteriovenous fistula of the scalp. J Neurosurg. 1987. 66: 773-4
5. Luessenhop A. Cirsoid aneurysms of the scalp. J Neurosurg. 1991. 75: 167
6. Moran AM, Aleman TS, Gausas RE, Fogt F. Traumatic arteriovenous fistula of the superficial temporal artery: A histopathologic report. Ophthalmic Plast Reconstr Surg. 2013. 29: e126-8
7. Morioka T, Nishio S, Hikita T. Traumatic arteriovenous fistulae of the scalp at the area of previous craniotomy. Surg Neurol. 1988. 30: 406-7
8. Sofela A, Osunronbi T, Hettige S. Scalp cirsoid aneurysms: Case illustration and systematic review of literature. Neurosurgery. 2019. 86: E98-107
9. Sousa LH, Gatto LA, Demartini Z, Koppe GL. Scalp cirsoid aneurysm: An updated systematic literature review and an illustrative case report. World Neurosurg. 2018. 119: 416-27