- Department of Surgery, Section of Neurosurgery, University of Puerto Rico, San Juan, Puerto Rico, United States.
Correspondence Address:
Orlando De Jesus, Department of Surgery, Section of Neurosurgery, University of Puerto Rico, San Juan, Puerto Rico, United States.
DOI:10.25259/SNI_418_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Orlando De Jesus. Descriptive surgical epidemiology of pituitary adenomas for a Hispanic population in Puerto Rico. 16-Jun-2023;14:206
How to cite this URL: Orlando De Jesus. Descriptive surgical epidemiology of pituitary adenomas for a Hispanic population in Puerto Rico. 16-Jun-2023;14:206. Available from: https://surgicalneurologyint.com/surgicalint-articles/12366/
Abstract
Background: Demographics and socioeconomic variables for patients with pituitary adenomas have been reported in the past. However, these studies included operated and nonoperated patients, in addition to microprolactinomas frequently diagnosed in women, revealing an elevated incidence among females. This study aimed to analyze the surgical incidence of pituitary adenomas for an adult Hispanic population in Puerto Rico over 6 years.
Methods: A retrospective and descriptive study was performed to investigate pituitary adenoma surgical incidence (per 100,000 people) among surgically treated pituitary adenomas in an adult (18 years or more) Puerto Rico Hispanic population. All new patients diagnosed with pituitary adenomas who underwent surgery at the Puerto Rico Medical Center between 2017 and 2022 were scrutinized. Inclusion criteria required a histopathological diagnosis of pituitary adenoma. Previously operated cases and non-Hispanic patients were excluded from the study. Patient characteristics were collected, along with the type of surgical treatment, tumor size, and secretory status.
Results: The analysis included 143 patients operated on for pituitary adenomas. Of these, 75 (52%) patients were male, and 68 (48%) were female. The median age of the patients was 56 years (range: 18–85). The average annual surgical incidence of adult Hispanic patients with pituitary adenomas was 0.73 surgeries/100,000 people. About 79% of the patients had non-functioning pituitary adenomas. About 94% of the patients were operated on using transsphenoidal surgery.
Conclusion: There was no sex predominance for surgical-treated pituitary adenomas in Puerto Rico. The surgical incidence for adult pituitary adenoma remained stable between 2017 and 2022.
Keywords: Demographics, Epidemiology, Ethnicity, Hispanic, Incidence, Pituitary adenoma, Race
INTRODUCTION
Pituitary adenomas are one of the most common benign brain tumors. In the US, pituitary adenomas account for 24% of primary benign intracranial neoplasms, with a 1.78 female-to-male ratio.[
In the US, only 42.3% of the patients with a pituitary adenoma diagnosis received histopathological confirmation.[
MATERIALS AND METHODS
A retrospective and descriptive study was performed to investigate pituitary adenoma surgical incidence (per 100,000 people) with respect to age and sex among surgically treated pituitary adenomas in an adult Hispanic population admitted at the major neurosurgical center in Puerto Rico. All new patients diagnosed with a pituitary adenoma who underwent surgery at the Puerto Rico Medical Center between 2017 and 2022 were carefully scrutinized. This medical center is the highest volume center in the country with dedicated neurosurgical facilities. The study utilized the neurosurgery admission database of the University of Puerto Rico, which, for pituitary adenomas, includes the majority of all the cases operated in Puerto Rico. Inclusion criteria required a histopathological diagnosis of pituitary adenoma. Previously operated cases and non-Hispanic patients were excluded from the study. Patients with a pituitary tumor diagnosed only by radiological studies or during a hormonal workup without a histopathological diagnosis were excluded from the study. Patients younger than 18 years were excluded from the study. Patient characteristics, including age, sex, type of surgical treatment, tumor size, and tumor secretory status were collected from the neurosurgery database and the hospital’s electronic health record. The tumor size was classified as microadenomas (<1 cm) or macroadenomas (1 cm or larger). Based on their hormonal secretory activity, pituitary adenomas were classified as functioning or nonfunctioning. The surgical incidence of pituitary adenomas per 100,000 people was calculated using the Puerto Rico population data from the US Census Bureau.[
RESULTS
The analysis included 143 patients operated on for pituitary adenomas. Of these, 75 (52%) patients were male, and 68 (48%) were female. The cohort’s median age was 56 years (range: 18–85). The median age for females was 52 years (range: 18–78), while for males was 56 years (range: 25–85). About 94% of the patients had a macroadenoma. Eight patients presented with symptoms following an acute pituitary apoplexy event. About 79% of the patients had nonfunctioning pituitary adenomas. Based on their hormonal secretory activity and tumor size, 15% of the patients had a functioning macroadenoma and 6% had a functioning microadenoma. The cohort included 14 acromegalic patients (three microadenomas and 11 macroadenomas), nine patients with Cushing disease (six microadenomas and three macroadenomas), six patients with a prolactinoma (all macroadenomas), and one patient presenting acromegaly concurrently with Cushing disease (macroadenoma). The prolactinoma patients were operated on as they did not respond to medical treatment or presented with acute severe apoplexy visual symptoms. These patients were operated on as an emergency without preoperative hormonal results. About 94% of the patients were operated on using transsphenoidal surgery. Results are summarized in
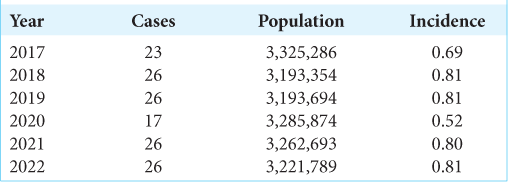
The surgical incidence per 100,000 people varied slightly throughout the study period, with the lowest in 2017 and 2020 [
DISCUSSION
Surgery is the primary treatment option for patients with symptomatic pituitary adenomas in good clinical condition.[
Pituitary adenoma epidemiologic studies that include patients with nonoperated prolactinomas and radiologically diagnosed tumors without histopathological confirmation do not reveal the incidence of adenomas treated with surgery. Epidemiological studies reporting the surgical incidence of particular neurosurgical diseases have been previously documented.[
Incidence according to sex
The most recent report from the CBTRUS documented that the pituitary adenoma incidence in the US/100,000 people was 4.62 overall (operated and nonoperated cases), being significantly higher for females (5.23) than for males (4.09) with a 1.78 female-to-male ratio.[
Incidence according to age
The highest incidence of pituitary adenomas in the US occurs in the 65+ age group.[
Incidence according to ethnicity
Hispanic ethnicity in the US exhibits a higher incidence (4.51 vs. 3.82) of benign pituitary adenomas than non-Hispanics.[
Incidence in Puerto Rico
The Puerto Rico Central Cancer Registry has collected information on cancer cases since 1950 and regularly submits the information to the CBTRUS and other cancer registries.[
Limitations
The main limitation of this study is that it presents a retrospective data analysis with potential selection bias. All the patients in this study underwent surgical resection and were, therefore, subject to surgical selection bias. Each treating neurosurgeon decided which patient should be managed surgically and chose the surgical approach independently. Moreover, some potential surgical cases may have been observed or treated only with radiotherapy if the patient was elderly, had significant comorbidities, or declined surgery. Furthermore, the study analyzed 6 years, limiting the findings’ generalizability to prior and subsequent years. The cohort did not include the entire Hispanic population of Puerto Rico; however, the information was obtained from the largest medical center, which covers approximately 90% of the country’s population for neurosurgical conditions. The data collected in this study did not include postoperative surgical results; therefore, surgical and clinical outcomes could not be analyzed. Finally, this study reports the surgical incidence for a Hispanic population which may not be applied to other ethnic groups.
CONCLUSION
This study showed no sex predominance for surgical-treated pituitary adenomas in Hispanic patients in Puerto Rico. Most patients were managed using transsphenoidal surgery. About 79% of the patients had nonfunctioning pituitary adenomas. The surgical incidence for adult pituitary adenoma remained reasonably stable between 2017 and 2022. The average annual surgical incidence of surgical-treated pituitary adenomas was 0.73 surgeries/100,000 people, with a peak incidence of 0.81 surgeries/100,000 people. Future multicenter research is necessary to increase knowledge of the surgical incidence in patients undergoing pituitary adenoma surgery.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Andereggen L, Frey J, Andres RH, El-Koussy M, Beck J, Seiler RW. 10-year follow-up study comparing primary medical vs. surgical therapy in women with prolactinomas. Endocrine. 2017. 55: 223-30
2. Asemota AO, Gallia GL. Impact of frailty on short-term outcomes in patients undergoing transsphenoidal pituitary surgery. J Neurosurg. 2019. 132: 360-70
3. Buurman H, Saeger W. Subclinical adenomas in postmortem pituitaries: Classification and correlations to clinical data. Eur J Endocrinol. 2006. 154: 753-8
4. Cancer in North America 2015-2019. Available from: https://www.naaccr.org/wp-content/uploads/2022/06/CiNA.2015-2019.v2.incidence.pdf [Last accessed on 2023 Jan 08].
5. Castellanos LE, Gutierrez C, Smith T, Laws ER, Iorgulescu JB. Epidemiology of common and uncommon adult pituitary tumors in the U.S. according to the 2017 World Health Organization classification. Pituitary. 2022. 25: 201-9
6. Chanson P, Maiter D. The epidemiology, diagnosis and treatment of Prolactinomas: The old and the new. Best Pract Res Clin Endocrinol Metab. 2019. 33: 101290
7. Ciccarelli A, Daly AF, Beckers A. The epidemiology of prolactinomas. Pituitary. 2005. 8: 3-6
8. Cote DJ, Ruzevick JJ, Kang KM, Pangal DJ, Bove I, Carmichael JD. Association between socioeconomic status and presenting characteristics and extent of disease in patients with surgically resected nonfunctioning pituitary adenoma. J Neurosurg. 2022. 137: 1699-706
9. Daly AF, Beckers A. The epidemiology of pituitary adenomas. Endocrinol Metab Clin North Am. 2020. 49: 347-55
10. Day PF, Loto MG, Glerean M, Picasso MF, Lovazzano S, Giunta DH. Incidence and prevalence of clinically relevant pituitary adenomas: retrospective cohort study in a health management organization in Buenos Aires, Argentina. Arch Endocrinol Metab. 2016. 60: 554-61
11. Ezzat S, Asa SL, Couldwell WT, Barr CE, Dodge WE, Vance ML. The prevalence of pituitary adenomas: A systematic review. Cancer. 2004. 101: 613-9
12. Ghaffari-Rafi A, Mehdizadeh R, Ghaffari-Rafi S, Castillo JA, Rodriguez-Beato FY, Leon-Rojas J. Demographic and socioeconomic disparities of pituitary adenomas and carcinomas in the United States. J Clin Neurosci. 2022. 98: 96-103
13. Gittleman H, Ostrom QT, Farah PD, Ondracek A, Chen Y, Wolinsky Y. Descriptive epidemiology of pituitary tumors in the United States, 2004-2009. J Neurosurg. 2014. 121: 527-35
14. Gruppetta M, Mercieca C, Vassallo J. Prevalence and incidence of pituitary adenomas: A population-based study in Malta. Pituitary. 2013. 16: 545-53
15. Guerra Velázquez GR. Hurricane María and public health in Puerto Rico: Lessons learned to increase resiliency and prepare for future disasters. Ann Glob Health. 2022. 88: 82
16. Hamidi O, Van Gompel J, Gruber L, Kittah NE, Donegan D, Philbrick KA. Management and outcomes of giant prolactinoma: A series of 71 patients. Endocr Pract. 2019. 25: 340-52
17. Hemminki K, Försti A, Ji J. Incidence and familial risks in pituitary adenoma and associated tumors. Endocr Relat Cancer. 2007. 14: 103-9
18. Khalid MU, Shah MM, Bajwa MH, Nathani KR, Laghari AA, Raghib MF. Schwannoma: A surgical epidemiology. J Pak Med Assoc. 2022. 72: S40-5
19. Lagerbäck T, Fritzell P, Hägg O, Nordvall D, Lønne G, Solberg TK. Effectiveness of surgery for sciatica with disc herniation is not substantially affected by differences in surgical incidences among three countries: Results from the Danish, Swedish and Norwegian spine registries. Eur Spine J. 2019. 28: 2562-71
20. Lania A, Beck-Peccoz P. Pituitary incidentalomas. Best Pract Res Clin Endocrinol Metab. 2012. 26: 395-403
21. Löfgren D, Valachis A, Olivecrona M. Older meningioma patients: A retrospective population-based study of risk factors for morbidity and mortality after neurosurgery. Acta Neurochir (Wien). 2022. 164: 2987-97
22. McDowell BD, Wallace RB, Carnahan RM, Chrischilles EA, Lynch CF, Schlechte JA. Demographic differences in incidence for pituitary adenoma. Pituitary. 2011. 14: 23-30
23. Melmed S, Casanueva FF, Hoffman AR, Kleinberg DL, Montori VM, Schlechte JA. Diagnosis and treatment of hyperprolactinemia: An Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011. 96: 273-88
24. Molitch ME. Diagnosis and treatment of pituitary adenomas: A review. JAMA. 2017. 317: 516-24
25. Mukherjee D, Zaidi HA, Kosztowski T, Chaichana KL, Salvatori R, Chang DC. Predictors of access to pituitary tumor resection in the United States, 1988-2005. Eur J Endocrinol. 2009. 161: 259-65
26. Murray G, Jiménez L, Báez F, Colón-Castillo LE, Brau RH. Descriptive profile of surgically-confirmed adult central nervous system tumors in Puerto Rico. P R Health Sci J. 2009. 28: 317-28
27. Orija IB, Weil RJ, Hamrahian AH. Pituitary incidentaloma. Best Pract Res Clin Endocrinol Metab. 2012. 26: 47-68
28. Ostrom QT, Price M, Neff C, Cioffi G, Waite KA, Kruchko C. CBTRUS statistical report: Primary brain and other central nervous system tumors diagnosed in the United States in 2015-2019. Neuro Oncol. 2022. 24: v1-95
29. Raappana A, Koivukangas J, Ebeling T, Pirilä T. Incidence of pituitary adenomas in Northern Finland in 1992-2007. J Clin Endocrinol Metab. 2010. 95: 4268-75
30. Rodríguez-Madera SL, Varas-Díaz N, Padilla M, Grove K, Rivera-Bustelo K, Ramos J. The impact of Hurricane Maria on Puerto Rico’s health system: Post-disaster perceptions and experiences of health care providers and administrators. Glob Health Res Policy. 2021. 6: 44
31. Serhal D, Weil RJ, Hamrahian AH. Evaluation and management of pituitary incidentalomas. Cleve Clin J Med. 2008. 75: 793-801
32. Shah MM, Bajwa MH, Khalid MU, Jooma R, Anis SB, Laghari AA. Prioritizing pituitary adenoma care in Pakistan: Analysis from an epidemiological study. J Pak Med Assoc. 2022. 72: S56-60
33. Shah MM, Khalid MU, Bajwa MH, Mirza FA, Anis SB, Akhunzada NZ. Gender disparities in brain tumours: A Pakistan brain tumour epidemiology study analysis. J Pak Med Assoc. 2022. 72: S79-84
34. Sundström N, Malm J, Laurell K, Lundin F, Kahlon B, Cesarini KG. Incidence and outcome of surgery for adult hydrocephalus patients in Sweden. Br J Neurosurg. 2017. 31: 21-7
35. Torres-Cintrón CR, Alvarado-Ortiz M, Román-Ruiz Y, OrtizOrtiz KJ, Zavala-Zegarra D, Tortolero-Luna G, editors. Cancer in Puerto Rico 2014-2018. San Juan, PR: Puerto Rico Central Cancer Registry; 2021. p. Available from: http://rcpr.org [Last accessed on 2023 Jan 02]
36. US Census Bureau. Available from: https://www.census.gov [Last accessed on 2023 Jan 02].
37. Villwock JA, Villwock MR, Goyal P, Deshaies EM. Current trends in surgical approach and outcomes following pituitary tumor resection. Laryngoscope. 2015. 125: 1307-12
38. Vroonen L, Daly AF, Beckers A. Epidemiology and management challenges in prolactinomas. Neuroendocrinology. 2019. 109: 20-7