- Department of Neurosurgery, Medicana Healthcare Group, Medicana Zincirlikuyu Hospital, Istanbul, Turkey
- Department of Neurosurgery, Acibadem Healthcare Group, Acibadem Altunizade Hospital, Istanbul, Turkey
- Department of Neurosurgery, Istanbul Medeniyet University, Prof. Dr. Suleyman Yalcin City Hospital, Istanbul, Turkey
- Department of Neurosurgery, Istinye University Liv Hospital, Istanbul, Turkey
- Department of Neurosurgery, Sanliurfa Training and Research Hospital, Sanliurfa, Turkey
- Department of Neurosurgery, University of Health Sciences, Prof. Dr. Cemil Tascioglu City Hospital, Istanbul, Turkey
Correspondence Address:
Ece Uysal, Department of Neurosurgery, Cemil Tascioglu State Hospital, Istanbul, Turkey.
DOI:10.25259/SNI_12_2025
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ahmed Yasin Yavuz1, Ece Uysal2, Hidayet Safak Cine3, Selim Seker4, Nazmi Ugur Unlu5, Suat Erol Celik6. Diagnostic efficacy of radionuclide scintigraphy in detecting lumboperitoneal shunt obstructions in idiopathic hydrocephalus and intracranial hypertension. 23-May-2025;16:194
How to cite this URL: Ahmed Yasin Yavuz1, Ece Uysal2, Hidayet Safak Cine3, Selim Seker4, Nazmi Ugur Unlu5, Suat Erol Celik6. Diagnostic efficacy of radionuclide scintigraphy in detecting lumboperitoneal shunt obstructions in idiopathic hydrocephalus and intracranial hypertension. 23-May-2025;16:194. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13575
Abstract
Background: This study aimed to evaluate the diagnostic effectiveness of radionuclide scintigraphy (RS) in detecting lumboperitoneal shunt (LPS) obstructions in patients with idiopathic normal pressure hydrocephalus (iNPH) and idiopathic intracranial hypertension (IIH).
Methods: We conducted a retrospective analysis of 44 patients who underwent LPS surgery between 2010 and 2020. Twenty-one patients were diagnosed with iNPH and 23 with IIH. Clinical symptoms, including gait disturbances, cognitive impairment, and urinary dysfunction for iNPH, and headaches and vision loss for IIH, were evaluated. Preoperative computed tomography/magnetic resonance imaging (MRI) scans assessed hydrocephalus indicators, and cerebrospinal fluid (CSF) opening pressure was measured through lumbar puncture. RS was performed using technetium-99m-diethylenetriaminepentaacetic acid, and findings were compared with surgical outcomes. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and concordance (kappa coefficient) were calculated to evaluate the diagnostic accuracy of RS.
Results: Of the 44 patients, 18 (40.9%) demonstrated total obstruction, 17 (38.6%) showed partial obstruction, and 9 (20.5%) had no obstruction on RS. All patients with total obstruction confirmed by RS had corresponding findings during surgery (PPV 100%). However, 10 of the 19 patients with partial or no obstruction on RS were found to have obstruction during surgery (NPV 47%). The kappa coefficient for total obstruction was 0.467 (P = 0.001), indicating good concordance between RS and surgical outcomes. Patients with lower CSF pressure, particularly those with iNPH, were more likely to experience false-negative RS results.
Conclusion: RS is a reliable tool for detecting total LPS obstructions, but its sensitivity for partial obstructions is limited. Extending imaging periods or integrating additional diagnostic tools such as MRI may improve detection accuracy, particularly in cases with low CSF pressure. Combining RS with clinical evaluations can reduce unnecessary shunt revisions and improve patient outcomes.
Keywords: Idiopathic intracranial hypertension, Lumboperitoneal shunt, Normal pressure hydrocephalus, Obstruction, Radionuclide scintigraphy
INTRODUCTION
Idiopathic intracranial hypertension (IIH) and intracranial hemorrhages, particularly ventricular hemorrhages, both contribute to increased intracranial pressure. Another condition with similar effects is idiopathic normal pressure hydrocephalus (iNPH), which presents with ventricular enlargement. To treat these conditions, cerebrospinal fluid (CSF) diversion shunts such as ventriculoperitoneal shunt (VPS), lumboperitoneal shunt (LPS), ventriculoatrial, or ventriculopleural systems are commonly utilized. Among these, VPS is a widely accepted procedure for managing both iNPH and IIH. In cases of communicating hydrocephalus, LPS offers a minimally invasive alternative by diverting CSF from the subarachnoid space to the peritoneal cavity.[
However, complications such as infection, malposition, or obstruction are common following shunt surgeries, often necessitating revisions. Literature suggests that approximately 25% of shunts require revision within the 1st year, and the lifetime revision rate can reach as high as 85%.[
Patients with iNPH often present with gait disturbances, cognitive decline, and urinary dysfunction due to ventricular enlargement, particularly involving the temporal horns or periventricular edema. In contrast, IIH is characterized by increased intracranial pressure without a clear underlying cause, typically manifesting with symptoms such as headaches, papilledema, and concentric vision loss. Notably, IIH patients exhibit higher CSF opening pressure compared to those with iNPH.[
Accurate identification of shunt malfunction is critical to guide appropriate revision surgery. The primary diagnostic tool is a clinical assessment of the patient’s symptoms. Although imaging modalities such as computed tomography (CT), magnetic resonance imaging (MRI), and shuntographies are commonly used to evaluate malfunction, their diagnostic accuracy is limited, particularly when trying to localize the extent or exact location of an obstruction.
Radionuclide scintigraphy (RS), first introduced by Di Chiro and Grove in 1966, has proven to be an effective and low-radiation diagnostic tool for detecting LPS malfunction. It is especially useful for assessing the degree of obstruction.[
MATERIALS AND METHODS
Study populations
This retrospective study included 44 patients who underwent LPS surgery due to iNPH or IIH between 2010 and 2020. Patients who received LPS for reasons other than iNPH or IIH were excluded from the study. Patients with intracranial tumors, patients under oncologic treatment, or patients with posttraumatic hydrocephalus were not included in the study, as there may be a difference in intracranial pressure. Pediatric cases were also excluded because their head development was not yet complete. The study population consisted of 28 males and 16 females, with a mean age of 51.02 ± 14.97 years (range: 30–79). Of these patients, 21 were diagnosed with iNPH and 23 with IIH. The clinical symptoms for iNPH included gait disturbance, cognitive impairment, and urinary dysfunction, while IIH patients presented with headaches and vision loss. Initial shuntographies were performed to evaluate shunt placement, and shunts with disconnections were excluded from further analysis.
Preoperative MRI and CT scans were performed to detect signs of hydrocephalus or increased intracranial pressure, such as non-progressive or progressive ventriculomegaly (Evans ratio >0.5), transverse sinus stenosis, periventricular edema, perioptic subarachnoid space distension, empty sella, or cerebral atrophy. Before administering the radionuclide, CSF opening pressure was measured through lumbar puncture. Pressures >20 cm H2O were considered elevated, while pressures below this threshold were classified as normal. All patients underwent shunt revision surgery due to clinical deterioration or persistent symptoms suggestive of shunt malfunction, irrespective of their RS findings. No patients were operated on solely for research or validation purposes.
Radionuclide scintigraphy imaging technique
Radionuclide scintigraphy (RS) was performed using Technetium-99m-diethylenetriaminepentaacetic acid as the radiotracer. A dose of 0.5–1 mCi was injected into the lumbar subarachnoid space through lumbar puncture, under sterile conditions. Before injection, CSF opening pressure was measured.
Imaging was performed using a dual-head gamma camera (GE Infinia Hawkeye 4 or Mediso AnyScan SC-SN-3s-60R), with low-energy high-resolution collimators.
Static images of the head, spine, and abdomen were acquired in anterior, posterior, and lateral views at 50,000 counts or 10 min per view, using a 256 × 256 matrix.
Delayed imaging was conducted at 4 and 24 h post-injection in selected cases. Single-photon emission computed tomography/CT was performed if anatomical localization was necessary, using a 128 × 128 matrix, 60 views per rotation, and 30-s acquisition per view. Images were reconstructed with the OSEM algorithm (two iterations, eight subsets) and a Butterworth pre-filter (cutoff frequency 0.320).
The RS results were classified into three categories: no obstruction, partial obstruction, or total obstruction. The presence of radioisotopes in the spinal canal and leakage of radioactivity into the peritoneal cavity indicated no obstruction. Total obstruction was defined as radioactivity ascending into the basal cisterns without radiotracer accumulation at the distal end of the tube, and no radioisotope activity in the abdomen in both early and late images. Partial obstruction was characterized by radiotracer accumulation at the distal tube site with minimal activity in the peritoneal cavity on late images. No patients required urgent shunt revision before undergoing radionuclide scintigraphy, and all patients included in the study had RS results available before surgery.
Outcome assessment and concordance analysis
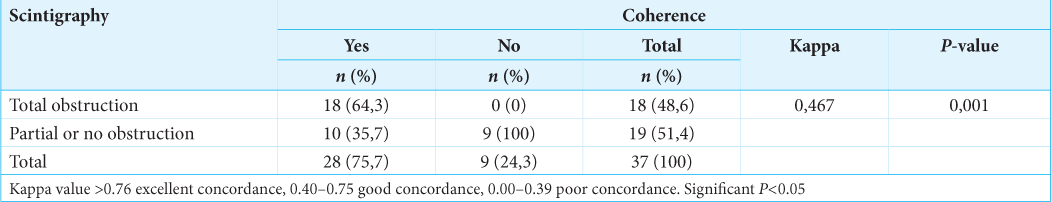
Shunt obstruction was confirmed during surgery. Scintigraphy findings were compared with surgical outcomes, and concordance was evaluated using the kappa coefficient. A kappa value >0.76 indicated excellent concordance, values between 0.40 and 0.75 indicated good concordance, and values below 0.40 indicated poor concordance. In this study, the kappa value for total obstruction was 0.467 (P = 0.001), indicating good concordance beyond chance.[
Statistical analysis
The normality of numerical variables was assessed using the Shapiro–Wilk test. For normally distributed data, differences between groups were compared using the Student’s t-test, while the Mann–Whitney U-test was used for non-normally distributed data. Categorical variables were analyzed using the Chi-squared test or Fisher’s exact test as appropriate.
Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy were calculated to assess the diagnostic performance of RS. Descriptive statistics were presented as mean ± standard deviation (SD) for normally distributed continuous variables, median [minimum–maximum] for non-normally distributed variables, and percentages for categorical variables. Statistical analysis was performed using the Statistical Package for the Social Sciences Windows version 21.0, and P < 0.05 was considered statistically significant.
RESULTS
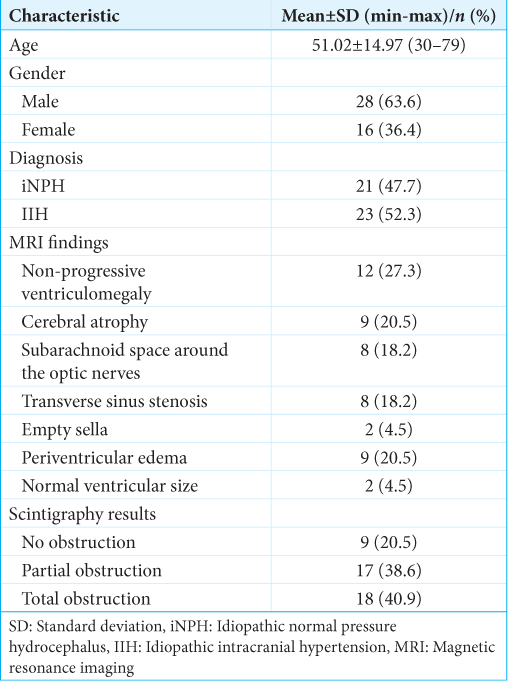
This study included 44 patients who underwent LPS surgery, with 21 (47.7%) patients diagnosed with iNPH and 23 (52.3%) diagnosed with IIH. The mean age of the patients was 51.02 ± 14.97 years, ranging from 30 to 79 years. The gender distribution revealed that 28 patients (63.6%) were male and 16 (36.4%) were female. The most common MRI findings included non-progressive ventriculomegaly in 12 patients (27.3%), cerebral atrophy in 9 patients (20.5%), and periventricular edema in 9 patients (20.5%). In addition, 18 patients (40.9%) showed total obstruction in scintigraphy, while 17 (38.6%) had partial obstruction, and 9 (20.5%) had no obstruction [
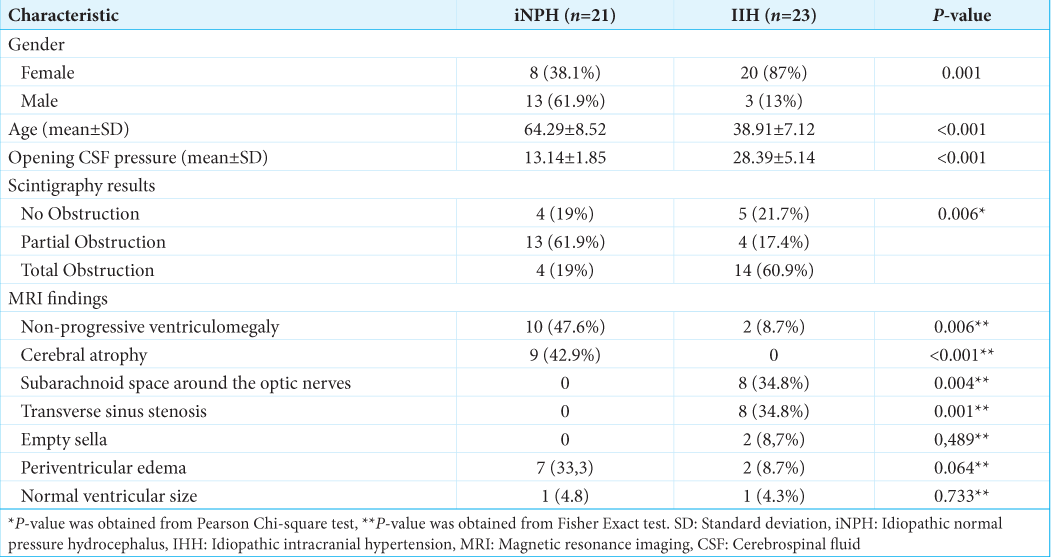
The comparison between the iNPH and IIH groups revealed significant differences in several parameters. The IIH group had a higher proportion of females (87%) compared to the iNPH group, where males were more prevalent (61.9%) (P = 0.001). The patients in the IIH group were significantly younger, with a mean age of 38.91 ± 7.12 years, compared to 64.29 ± 8.52 years in the iNPH group (P < 0.001). The mean opening CSF pressure was also significantly higher in the IIH group (28.39 ± 5.14 cm H2O) than in the iNPH group (13.14 ± 1.85 cm H2O) (P < 0.001). Regarding scintigraphy results, total obstruction was more frequently observed in the IIH group (60.9%) than in the iNPH group (19%), while partial obstruction was more common in the iNPH group (61.9%) (P = 0.006) [
MRI findings also showed notable differences between the two groups. In the iNPH group, non-progressive ventriculomegaly (47.6%) and cerebral atrophy (42.9%) were more frequently observed. On the other hand, patients in the IIH group had higher rates of prominent subarachnoid space around the optic nerves (34.8%) and transverse sinus stenosis (34.8%) (P < 0.05 for both comparisons). Other MRI findings, such as empty sella and periventricular edema, were less common and did not differ significantly between the two groups (P > 0.05) [
The concordance analysis between scintigraphy results and surgical findings showed good agreement for total obstruction cases. Among the 18 patients with total obstruction identified through scintigraphy, all were confirmed to have obstruction during surgery, yielding a PPV of 100%. However, for patients with partial or no obstruction in scintigraphy, obstruction was found in ten of 19 cases during surgery, resulting in a NPV of 47%. The overall concordance between scintigraphy and surgical outcomes was assessed using the kappa coefficient, which was calculated as 0.467 (P = 0.001), indicating good concordance [
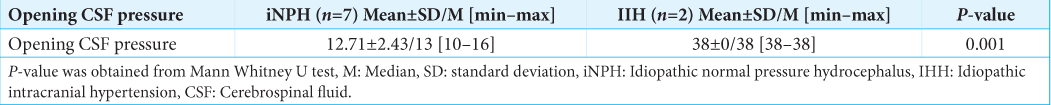
A comparison was made between the CSF opening pressure values of patients in the iNPH and IIH groups whose scintigraphy and surgical results were incompatible. The mean opening CSF pressure in the iNPH group was 12.71 cm H2O, significantly lower than the 38 cm H2O observed in the IIH group (P = 0.001). This suggests that low CSF pressure in iNPH patients may have contributed to false-negative scintigraphy results, which could lead to underdiagnosis of obstruction in these cases [
DISCUSSION
iNPH is a form of communicating hydrocephalus that primarily affects older individuals. It can be managed using LPS, which are also commonly used in the treatment of IIH, a condition characterized by normal or reduced ventricular size.[
Several comparative studies have demonstrated that VPS and LPS provide similar effectiveness and complication rates, with no significant differences between the two techniques.[
To mitigate potential complications, prioritizing safety measures is essential to reduce the risk of new neurological deficits. For patients with IIH who have smaller ventricles, Olivera et al. suggested that navigation-assisted VPS could be a useful approach.[
As an alternative to ventricular access, LPS offers several practical advantages in selected patients. LPS is often recommended due to its simplified insertion procedure, effective CSF drainage, lower incidence of infections, and fewer complications related to brain parenchyma. However, injuries to the brain parenchyma, such as intracranial hemorrhage, contusions, and epilepsy, can still occur if the procedure is not carefully managed.[
Obstruction is a common complication in all shunt procedures, often necessitating revisions.[
Clinical deterioration or the recurrence of symptoms is typically the first sign of shunt dysfunction. In the absence of acute hydrocephalus or elevated intracranial pressure, evaluations rely primarily on patient complaints, making it challenging to go beyond subjective assessments. Diagnosing iNPH can be particularly difficult and time-consuming. Similarly, in IIH, headaches are often evaluated subjectively unless they lead to visual impairment. Ensuring an accurate diagnosis is crucial to avoid unnecessary revision surgeries.
When shunt dysfunction is suspected based on clinical examination, imaging techniques should be used to confirm the diagnosis and guide treatment. CT or MRI scans can reveal key indicators such as non-progressive cerebral atrophy, prominent subarachnoid space around the optic nerves, transverse sinus stenosis, empty sella, or periventricular edema.[
Radionuclide scintigraphy (RS), first described by Di Chiro and Grove in 1966 [
In clinical practice, shunt failure in LPS patients is often suspected based on subjective evaluations such as clinical worsening or an increase in symptoms, especially when imaging results are inconclusive.[
MRI is a valuable diagnostic tool for both iNPH and IIH, although not all participants in our study underwent MRI. In cases where MRI findings are inconclusive, RS can serve as an effective alternative to identify shunt obstructions, potentially preventing unnecessary surgeries.
In our clinic, RS is performed when shunt failure due to obstruction is suspected. We retrospectively evaluated patient data and compared scintigraphy results with surgical findings. Scintigraphy revealed complete obstruction in 18 out of 44 patients. All 18 patients who underwent surgery were confirmed to have obstruction during the operation, with 12 cases of distal obstruction and six cases of proximal obstruction. Shunt revisions were performed accordingly.
Nineteen patients who were diagnosed with partial or no obstruction based on scintigraphy underwent surgery due to clinical deterioration. However, during surgery, obstruction was detected in ten of these patients. Based on our findings, the sensitivity of scintigraphy in detecting obstruction was calculated at 64.3%. Importantly, all patients identified with total obstruction through scintigraphy were confirmed to have obstruction during surgery, yielding a PPV of 100%. Conversely, in nine patients who showed non-obstructive or partial obstruction on scintigraphy, no obstruction was found during surgery, resulting in a NPV of 47%.
To better understand the discrepancies in scintigraphy results, we analyzed patients whose scintigraphy and surgical findings were inconsistent. Seven of these patients had iNPH, and two had IIH. We found that the mean CSF opening pressure in iNPH patients with incompatible scintigraphy results was 12.71 cm H2O. These findings suggest that lower CSF opening pressure may affect the NPV of scintigraphy. In cases of low CSF pressure, resulting in low flow or difficulty delivering the radionuclide, scintigraphy may fail to detect obstruction. In such cases, extending the imaging period to 24 or 48 h may be necessary to confirm the absence of obstruction.
Limitations
The investigation had several limitations. First, it is worth noting that the most commonly used diagnoses for LPS are iNPH and IHH. Our study included two patient groups who received LPS and were monitored. Variations in pathogenesis among these patients may have contributed to the observed variability in our sample. It is worth noting that the difference in heterogeneity for the primary objective of our study was not taken into consideration, as the same treatment strategy with LPS was used in both patient groups. In addition, it is important to mention that our research was conducted with a limited sample size of patients and without the inclusion of a power analysis. Furthermore, we encountered difficulties in replicating scintigraphic imaging within a 24-hour timeframe post-injection, which limited our capacity to showcase progress in cases of low flow.
CONCLUSION
Our study confirms that radionuclide scintigraphy is a reliable diagnostic tool for identifying total shunt obstructions in patients with LPS, particularly in cases of iNPH and IIH. However, its limited sensitivity in detecting partial obstructions highlights the need for caution when relying solely on this method. For patients with CSF pressure or inconclusive RS results, extending the imaging period or integrating other diagnostic tools such as MRI may enhance detection accuracy. Based on our findings, we recommend combining clinical evaluations with advanced imaging modalities to minimize unnecessary shunt revisions and associated risks. This approach can help improve overall patient outcomes by ensuring more accurate diagnoses and targeted interventions.
Ethical approval:
The research/study approved by the Institutional Review Board at Istanbul Health Sciences University Prof Dr Cemil Tascioglu city Hospita, number 458, dated 2024.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship:
Nil.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Abubaker K, Ali Z, Raza K, Bolger C, Rawluk D, O’Brien D. Idiopathic intracranial hypertension: Lumboperitoneal shunts versus ventriculoperitoneal shunts--case series and literature review. Br J Neurosurg. 2011. 25: 94-9
2. Chiewvit S, Nuntaaree S, Kanchaanapiboon P, Chiewvit P. Assessment lumboperitoneal or ventriculoperitoneal shunt patency by radionuclide technique: A review experience cases. World J Nucl Med. 2014. 13: 75-84
3. Chumas PD, Kulkarni AV, Drake JM, Hoffman HJ, Humphreys RP, Rutka JT. Lumboperitoneal shunting: A retrospective study in the pediatric population. Neurosurgery. 1993. 32: 376-83
4. Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960. 20: 37-46
5. De Oliveira AJ, Pinto FC, Teixeira MJ. Comparative study of the effectiveness of lumboperitoneal and ventriculoperitoneal shunting with neuronavigation in the treatment of idiopathic intracranial hypertension. Neurol India. 2020. 68: 1061-4
6. Di Chiro G, Grove AS. Evaluation of surgical and spontaneous cerebrospinal fluid shunts by isotope scanning. J Neurosurg. 1966. 24: 743-8
7. Goto Y, Oka H, Hino A. Lumboperitoneal shunt surgery using valve implantation on the paravertebral spinal muscle. World Neurosurg. 2021. 146: e1092-6
8. Johnston I, Besser M, Morgan MK. Cerebrospinal fluid diversion in the treatment of benign intracranial hypertension. J Neurosurg. 1988. 69: 195-202
9. Khan F, Rehman A, Shamim MS, Bari ME. Factors affecting ventriculoperitoneal shunt survival in adult patients. Surg Neurol Int. 2015. 6: 25
10. Kharkar S, Shuck J, Kapoor S, Batra S, Williams MA, Rigamonti D. Radionuclide shunt patency study for evaluation of suspected ventriculoperitoneal shunt malfunction in adults with normal pressure hydrocephalus. Neurosurgery. 2009. 64: 909-16 discussion 916-8
11. Liu A, Elder BD, Sankey EW, Goodwin CR, Jusué-Torres I, Rigamonti D. The utility of computed tomography in shunted patients with idiopathic intracranial hypertension presenting to the emergency department. World Neurosurg. 2015. 84: 1852-6
12. Nakajima M, Miyajima M, Ogino I, Akiba C, Kawamura K, Kurosawa M. Shunt intervention for possible idiopathic normal pressure hydrocephalus improves patient outcomes: A nationwide hospital-based survey in Japan. Front Neurol. 2018. 9: 421
13. Reddy GK, Bollam P, Caldito G. Long-term outcomes of ventriculoperitoneal shunt surgery in patients with hydrocephalus. World Neurosurg. 2014. 81: 404-10
14. Rosenberg ML, Corbett JJ, Smith C, Goodwin J, Sergott R, Savino P. Cerebrospinal fluid diversion procedures in pseudotumor cerebri. Neurology. 1993. 43: 1071-2
15. Sunderland GJ, Jenkinson MD, Conroy EJ, Gamble C, Mallucci CL. Neurosurgical CSF diversion in idiopathic intracranial hypertension: A narrative review. Life (Basel). 2021. 11: 393
16. Sun T, Yuan Y, Zhang Q, Zhou Y, Li X, Yu H. Establishing a preoperative evaluation system for lumboperitoneal shunt: Approach to attenuate the risk of shunt failure. World Neurosurg. 2018. 117: e308-15
17. Sun T, Li X, Zhang Q, Zhou Y, Guan J. Efficacy and safety of lumboperitoneal shunt in the treatment of all-cause communicating hydrocephalus: Analysis of risk factors of shunt failure. World Neurosurg. 2019. 132: e956-62
18. Thompson EM, Wagner K, Kronfeld K, Selden NR. Using a 2-variable method in radionuclide shuntography to predict shunt patency. J Neurosurg. 2014. 121: 1504-7
19. Tsai SY, Wang SY, Shiau YC, Yang LH, Wu YW. Clinical value of radionuclide shuntography by qualitative methods in hydrocephalic adult patients with suspected ventriculoperitoneal shunt malfunction. Medicine (Baltimore). 2017. 96: e6767
20. Wang VY, Barbaro NM, Lawton MT, Pitts L, Kunwar S, Parsa AT. Complications of lumboperitoneal shunts. Neurosurgery. 2007. 60: 1045-8 discussion 1049
21. Xie D, Chen H, Guo X, Liu Y. Comparative study of lumboperitoneal shunt and ventriculoperitoneal shunt in the treatment of idiopathic normal pressure hydrocephalus. Am J Transl Res. 2021. 13: 11917-24