- Department of Neurosurgery, Desert Regional Medical Center, Palm Springs, California, United States.
- Grossman School of Medicine, New York University, New York, United States.
- Department of Neurology, University of Washington, Main Hospital, Seattle, Washington State, United States.
- Department of Molecular and Integrative Physiology, University of Michigan, Ann Arbor, Michigan, United States.
- Department of Neurobiology, University of California Davis, Davis, California, United States.
- Medical School, University of Medicine and Health Sciences, New York, United States.
- College of Osteopathic Medicine, Western University of Health Sciences, Pomona, California, United States.
- School of Medicine, University of New Mexico, Albuquerque, New Mexico, United States.
Correspondence Address:
Brian Fiani
School of Medicine, University of New Mexico, Albuquerque, New Mexico, United States.
DOI:10.25259/SNI_154_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Brian Fiani1, Marisol Soula2, Kasra Sarhadi3, Daniel Nikolaidis4, Neha Gautam5, Nicholas J. Fiani6, Ryne Jenkins7, Alexander Rose8. Direct N-butyl-2-cyanoacrylate injections to the head and neck for percutaneous embolized devascularization. 30-Mar-2021;12:131
How to cite this URL: Brian Fiani1, Marisol Soula2, Kasra Sarhadi3, Daniel Nikolaidis4, Neha Gautam5, Nicholas J. Fiani6, Ryne Jenkins7, Alexander Rose8. Direct N-butyl-2-cyanoacrylate injections to the head and neck for percutaneous embolized devascularization. 30-Mar-2021;12:131. Available from: https://surgicalneurologyint.com/surgicalint-articles/10678/
Abstract
Background: N-butyl-2-cyanoacrylate (NBCA) has been used for vascular malformations since the 1980s; however, few studies have looked at applications, procedural techniques, and outcome throughout many institutions. Herein, we review applications, procedural techniques, previous literature, and outcomes for the use of NBCA specifically through percutaneous technique in treating head and neck vascular pathology.
Methods: An extensive literature review using PubMed database with published literature containing “N-butyl-2-cyanoacrylate embolization,” was performed. No date restrictions were used. Cross-checking of articles was conducted to exclude duplicate articles. The articles were screened for their full text and English language availability. We finalized those articles pertaining to the topic.
Results: The search yielded 1124 related articles. When comparing surgical resection to embolization with NBCA for cerebral AVMs, complications were similar in both groups and included hemorrhage (15%), residual AVM (6%), and cerebrospinal fluid leak (3%). Their mortality rate was 3% in both groups. Preoperative percutaneous embolization does show improved surgical outcomes.
Conclusion: NBCA is a fast-acting liquid embolic material used in the treatment of a variety of vascular malformations and lesions of the head and neck. Investigations surrounding the use of NBCA injections as a new alternative embolic agent began in the 1980’s. Administration of NBCA has been shown to be useful in minimizing intraoperative blood loss and controlling acute hemorrhage. Performing percutaneous embolization with NBCA provides a successful alternative for surgeons when transcatheter embolization techniques may prove to be too difficult to perform. Embolization using NBCA will continue to play in integral role in the treatment of malignant lesions and vascular malformations. Continued research is warranted to improve safety, outcomes, and further develop clinical applications of NBCA.
Keywords: Arteriovenous malformation, Embolization, N-butyl-2-cyanoacrylate, Obliteration
INTRODUCTION
Cyanoacrylate glues are liquid alkyl-2-cyanoacrylae monomers that have the ability to form flexible polymers to soft tissues. N-butyl-2-cyanoacrylate (NBCA) is a class of cyanoacrylates which is a group of adhesives that are fast-acting, due to their ability to form low viscosity fluids in a monomer state and polymerize instantly on contact with ionic substances. NBCA’s are the most widely used liquid embolic material in the world. They are useful for a variety of brain and neck pathology such as arteriovenous malformations (AVMs).[
Isobutyl-2-cyanoacrylate (IBCA) was initially used, but then it was replaced by N-butyl 2-cyanoacrylate (NBCA) in the mid-1980s.[
While many different treatment options are utilized in treating patients, knowing the effectiveness of this treatment is quite important. Herein, we will assess the applications for NBCA’s, procedural techniques, and patient outcomes when using NBCA embolization.
PATIENT SELECTION
Percutaneous embolization of arterial and/or venous malformations, pseudoaneurysms, and other aberrant vasculature with NBCA has demonstrated high degrees of success for a variety of pathologies across a diverse population of patients.[
Although studies directly evaluating the use of NBCA in head and neck pathologies are limited in number, various prospective cohort studies and retrospective analyses have determined vascular lesion characteristics and criteria that favor successful outcomes of NBCA embolization therapy.[
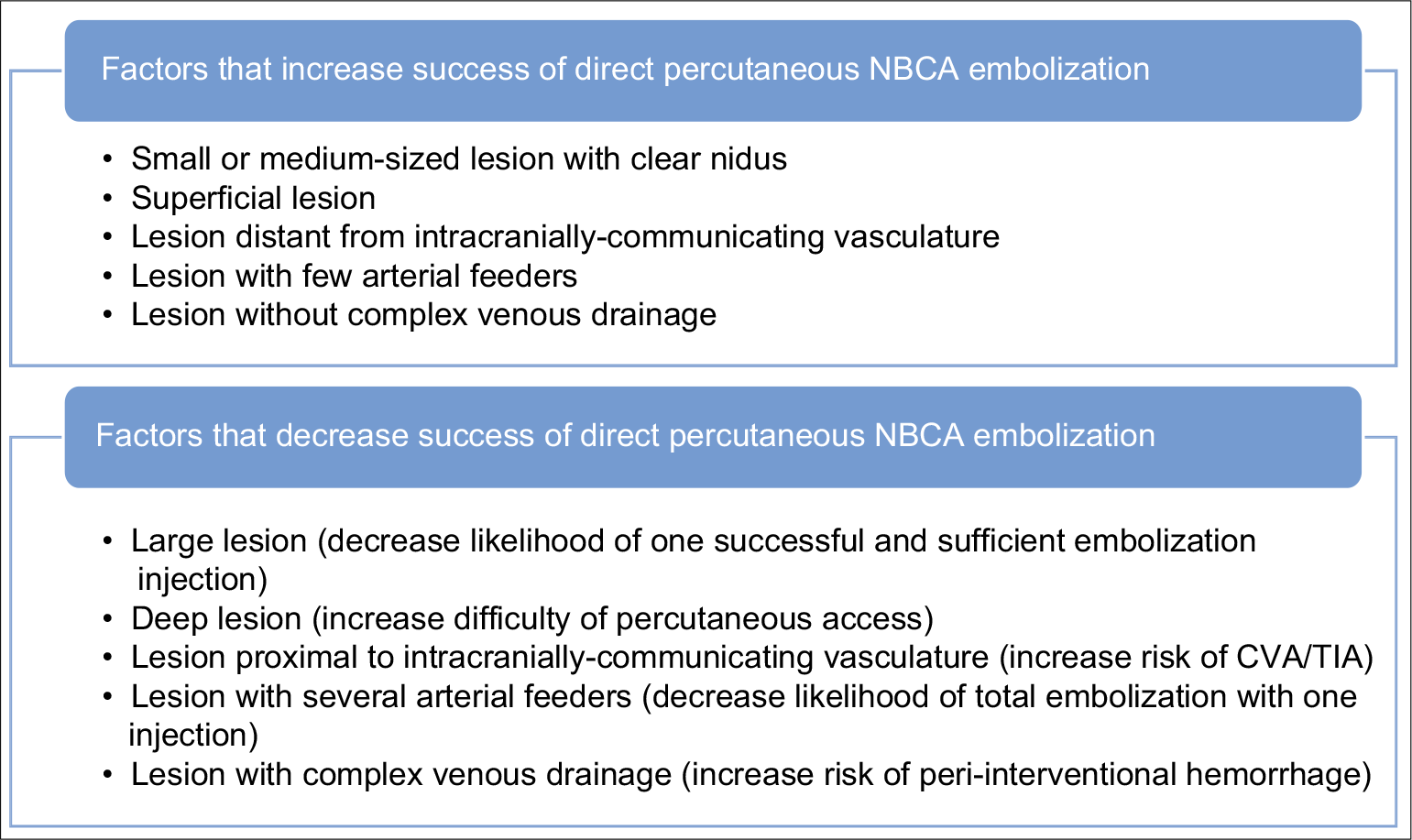
Absolute indications or contraindications aside, appropriateness of NBCA percutaneous embolization therapy for head and neck lesions may be determined by considering a wide variety of lesion characteristics that contribute to the anticipated degree of intervention success [
Small to medium-sized vascular lesion with clearly demarcated nidus Superficial lesion easily accessible with a percutaneous approach The lesion is not in direct contact with or extension to arteries such as the ICA or ECA with intracranial communication that would carry high risk of intracranial embolization of sclerosant material Lesions with few arterial feeders that allow for adequate reflux of NBCA along feeder vessels to block blood flow to the lesion Lesions without complex venous drainage to minimize post injection hemorrhage risk.
The decision to pursue direct percutaneous NBCA embolization of head and neck lesions is typically made when transcatheter approaches are impractical and surgical resection alone carries too high of a perioperative hemorrhage risk. A patient’s comorbidities and the lesion’s vascular characteristics as explained above must be thoroughly evaluated in great detail to determine the safety and likelihood of success of this type of intervention.
BRIEF OVERVIEW OF TECHNIQUES
NBCA is the most commonly used liquid embolic agent that due to its low viscosity can be percutaneous injected through a needle. NBCA is composed of liquid alkyl-2-cyanoacrylate monomers that rapidly polymerize on contact with ionic substances such as blood or water.[
Direct percutaneous injection of NBCA is used when transarterial catherization is not feasible or dangerous to perform, for example, with cases of tortuous vasculature or vessels with atherosclerotic plaques.[
TRIALS, OUTCOMES, AND EFFECTIVENESS
Investigations surrounding the use of NBCA injections as a new alternative embolic agent began in the 1980’s. Early work from interventional neuroradiologist concluded that clinically and biologically NBCA was an acceptable alternative to IBCA.[
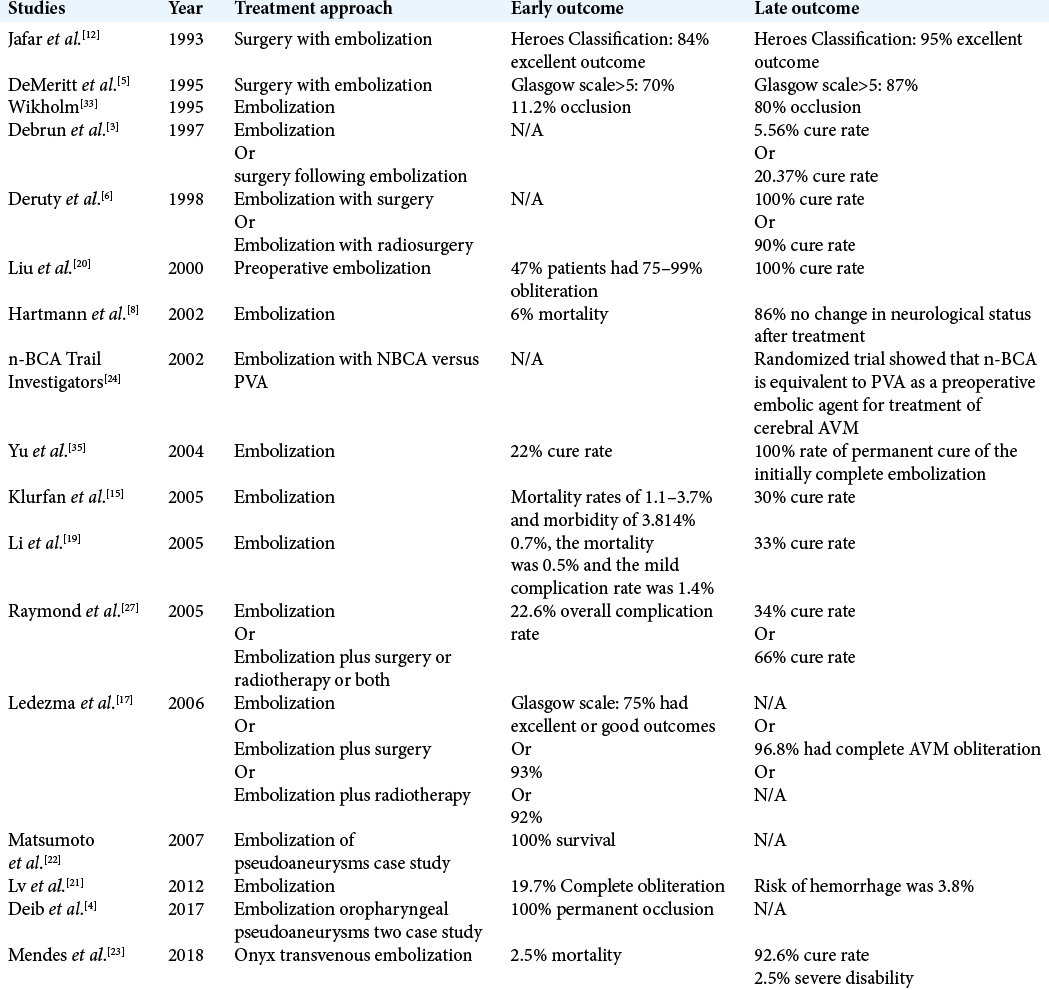
Studies of embolization treatment with NBCA in head and neck lesions, specifically AVM, began in 1993 by Jafar et al. [
With an increase in the use of NBCA, there was a parallel increase in conversations surrounding the safety of NBCA embolization. For the last decade, the efficacy and risks of NBCA were the focus of many clinical researchers. The results of several clinical papers suggest that NBCA in combination with surgery can lead to a 100% cure rate. However, the risk of NBCA embolization is not negligible and should only be used as a reductive technique only when it is absolutely necessary to allow for complete cure of the AVM.[
CONCLUSION
Embolization through direct percutaneous delivery of NBCA provides promising outcomes in the treatment of vascular malformations and lesions. As our treatment of vascular malformations of the head and neck continues to evolve, NBCA will continue to play a helpful roll in minimizing intraoperative bleeding of malignant lesions and assisting surgeons where traditional transcatheter embolization approaches face challenges. Although this procedure is not without risk of significant complication, performing the procedure in the guidance of trained surgeons provides favorable outcomes.
Over two decades later, we have extensive research on the use and outcomes of NBCA. Its expansion from abdominal to head and neck lesions has proven to reduce morbidity and mortality rates in AVM patients as well as cancer patients with hemorrhagic lesions, such as, ruptured pseudoaneurysms.[
Continual research directly assessing NBCA’s outcomes of vascular disorders and lesions will provide increasingly beneficial data to solidify NBCA outcomes. Further technical guidance and modifications may help improve the safety and success of percutaneous embolized devascularization with NBCA. In addition, future studies further developing applications for the use of NBCA injections may be of benefit in the clinical setting.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abud DG, Mounayer C, Benndorf G, Piotin M, Spelle L, Moret J. Intratumoral injection of cyanoacrylate glue in head and neck paragangliomas. AJNR Am J Neuroradiol. 2004. 25: 1457-62
2. Brothers MF, Kaufmann JC, Fox AJ, Deveikis JP. n-Butyl 2-cyanoacrylate--substitute for IBCA in interventional neuroradiology: Histopathologic and polymerization time studies. AJNR Am J Neuroradiol. 1989. 10: 777-86
3. Debrun GM, Aletich V, Ausman JI, Charbel F, Dujovny M. Embolization of the nidus of brain arteriovenous malformations with n-butyl cyanoacrylate. Neurosurgery. 1997. 40: 112-20
4. Deib G, El Mekabaty A, Gailloud P, Pearl MS. Treatment of hemorrhagic head and neck lesions by direct puncture and nBCA embolization. BMJ Case Rep. 2017. 2017: bcr2017013335
5. DeMeritt JS, Pile-Spellman J, Mast H, Moohan N, Lu DC, Young WL. Outcome analysis of preoperative embolization with N-butyl cyanoacrylate in cerebral arteriovenous malformations. AJNR Am J Neuroradiol. 1995. 16: 1801-7
6. Deruty R, Pelissou-Guyotat I, Morel C, Bascoulergue Y, Turjman F. Reflections on the management of cerebral arteriovenous malformations. Surg Neurol. 1998. 50: 245-55
7. Gordhan A. Intra-operative N-butyl cyanoacrylate embolization arrest of uncontrollable hemorrhage during meningioma resection. J Clin Neurosci. 2016. 23: 142-5
8. Hartmann A, Pile-Spellman J, Stapf C, Sciacca RR, Faulstich A, Mohr JP. Risk of endovascular treatment of brain arteriovenous malformations. Stroke. 2002. 33: 1816-20
9. Higashino N, Sonomura T, Fukuda K, Ikoma A, Okuhira R, Ueda S. Feasibility and safety of n-butyl cyanoacrylatelipiodol-iopamidol as an alternative liquid embolic material. Cardiovasc Intervent Radiol. 2020. 44: 482-8
10. Hill H, Chick JF, Hage A, Srinivasa RN. N-butyl cyanoacrylate embolotherapy: Techniques, complications, and management. Diagn Interv Radiol. 2018. 24: 98-103
11. Ierardi AM. Glue or onyx: A guide to choice–tips and techniques. J Endovasc Resusc Trauma Manage. 2020. 4: 33-9
12. Jafar JJ, Davis AJ, Berenstein A, Choi IS, Kupersmith MJ. The effect of embolization with N-butyl cyanoacrylate prior to surgical resection of cerebral arteriovenous malformations. J Neurosurg. 1993. 78: 60-9
13. Keller FS, Rosch J, Baur GM, Taylor LM, Dotter CT, Porter JM. Percutaneous angiographic embolization: A procedure of increasing usefulness: Review of a decade of experience. Am J Surg. 1981. 142: 5-13
14. Kish JW, Katz MD, Marx MV, Harrell DS, Hanks SE. N-butyl cyanoacrylate embolization for control of acute arterial hemorrhage. J Vasc Interv Radiol. 2004. 15: 689-95
15. Klurfan P, Gunnarsson T, Haw C, Ter Brugge KG. Endovascular treatment of brain arteriovenous malformations: The toronto experience. Interv Neuroradiol. 2005. 11: 51-6
16. Krishnamoorthy T, Gupta AK, Rajan JE, Thomas B. Stroke from delayed embolization of polymerized glue following percutaneous direct injection of a carotid body tumor. Korean J Radiol. 2007. 8: 249-53
17. Ledezma CJ, Hoh BL, Carter BS, Pryor JC, Putman CM, Ogilvy CS. Complications of cerebral arteriovenous malformation embolization: Multivariate analysis of predictive factors. Neurosurgery. 2006. 58: 602-11
18. Lee BB, Bergan JJ. Advanced management of congenital vascular malformations: A multidisciplinary approach. Cardiovasc Surg. 2002. 10: 523-33
19. Li TL, Fang B, He XY, Duan CZ, Wang QJ, Zhao QP. Complication analysis of 469 brain arteriovenous malformations treated with N-butyl cyanoacrylate. Interv Neuroradiol. 2005. 11: 141-8
20. Liu HM, Huang YC, Wang YH. Embolization of cerebral arteriovenous malformations with n-butyl-2-cyanoacrylate. J Formos Med Assoc. 2000. 99: 906-13
21. Lv X, Wu Z, Li Y, Yang X, Jiang C. Hemorrhage risk after partial endovascular NBCA and ONYX embolization for brain arteriovenous malformation. Neurol Res. 2012. 34: 552-6
22. Matsumoto T, Yamagami T, Kato T, Hirota T, Yoshimatsu R, Nishimura T. Transcatheter arterial embolisation of a ruptured pseudoaneurysm of the lingual artery with n-butyl cyanoacrylate. Br J Radiol. 2007. 80: e54-7
23. Mendes GA, Kalani MY, Iosif C, Lucena AF, Carvalho R, Saleme S. Transvenous curative embolization of cerebral arteriovenous malformations: A prospective cohort study. Neurosurgery. 2018. 83: 957-64
24. . N-butyl cyanoacrylate embolization of cerebral arteriovenous malformations: Results of a prospective, randomized, multi-center trial. AJNR Am J Neuroradiol. 2002. 23: 748-55
25. Nichols DA, Rufenacht DA, Jack CR, Forbes GS. Embolization of spinal dural arteriovenous fistula with polyvinyl alcohol particles: Experience in 14 patients. AJNR Am J Neuroradiol. 1992. 13: 933-40
26. Ozyer U, Harman A, Yildirim E, Aytekin C, Akay TH, Boyvat F. Devascularization of head and neck paragangliomas by direct percutaneous embolization. Cardiovasc Intervent Radiol. 2010. 33: 967-75
27. Raymond J, Iancu D, Weill A, Guilbert F, Bahary JP, Bojanowski M. Embolization as one modality in a combined strategy for the management of cerebral arteriovenous malformations. Interv Neuroradiol. 2005. 11: 57-62
28. Takao H, Abe O. Triple-balloon-assisted n-butyl-2-cyanoacrylate embolization of a cirsoid renal arteriovenous malformation. Vasa. 2020. 49: 147-50
29. Takao H, Shibata E, Amemiya S, Abe O. Double-balloon-assisted N-butyl-2-cyanoacrylate embolization of nontumorous intrahepatic arterioportal shunts. J Vasc Interv Radiol. 2019. 30: 1210-4
30. Takeuchi Y, Morishita H, Sato Y, Hamaguchi S, Sakamoto N, Tokue H.editors. Guidelines for the use of NBCA in vascular embolization devised by the Committee of Practice Guidelines of the Japanese Society of Interventional Radiology (CGJSIR), 2012 edition. Jpn J Radiol. 2014. 32: 500-17
31. Vaidya S, Tozer KR, Chen J. An overview of embolic agents. Semin Intervent Radiol. 2008. 25: 204-15
32. Valavanis A. Preoperative embolization of the head and neck: Indications, patient selection, goals, and precautions. AJNR Am J Neuroradiol. 1986. 7: 943-52
33. Wikholm G. Occlusion of cerebral arteriovenous malformations with N-butyl cyano-acrylate is permanent. AJNR Am J Neuroradiol. 1995. 16: 479-82
34. Yoshida RY, Kariya S, Nakatani M, Komemushi A, Kono Y, Tanigawa N. Direct puncture embolization using N-butyl cyanoacrylate for a hepatic artery pseudoaneurysm. Minim Invasive Ther Allied Technol. 2014. 23: 110-4
35. Yu SC, Chan MS, Lam JM, Tam PH, Poon WS. Complete obliteration of intracranial arteriovenous malformation with endovascular cyanoacrylate embolization: Initial success and rate of permanent cure. AJNR Am J Neuroradiol. 2004. 25: 1139-43
36. Zaki Ghali MG, Kan P, Britz GW. Curative embolization of arteriovenous malformations. World Neurosurg. 2019. 129: 467-86