- Department of Neurosurgery, Professor of Clinical Neurosurgery, School of Medicine, State University of NY at Stony Brook, NY, USA, and Editor-in-Chief Surgical Neurology International
- Assistant Clinical Professor of Orthopedics, NYU Langone Hospital, Long Island, Long Island, NY, USA.1122 Franklin Avenue, Suite 106, Garden City, NY 11530, USA
Correspondence Address:
Nancy E. Epstein, M.D., F.A.C.S Department of Neurosurgery, Professor of Clinical Neurosurgery, School of Medicine, State University of NY at Stony Brook, NY, USA, and Editor-in-Chief Surgical Neurology International.
DOI:10.25259/SNI_135_2025
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein1, Marc A. Agulnick2. Do drains alter the frequency of postoperative spinal epidural hematomas (SpEH) and surgical site infections (SSI) in predominantly lumbar spine surgery? Short review/perspective. 07-Mar-2025;16:85
How to cite this URL: Nancy E. Epstein1, Marc A. Agulnick2. Do drains alter the frequency of postoperative spinal epidural hematomas (SpEH) and surgical site infections (SSI) in predominantly lumbar spine surgery? Short review/perspective. 07-Mar-2025;16:85. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13427
Abstract
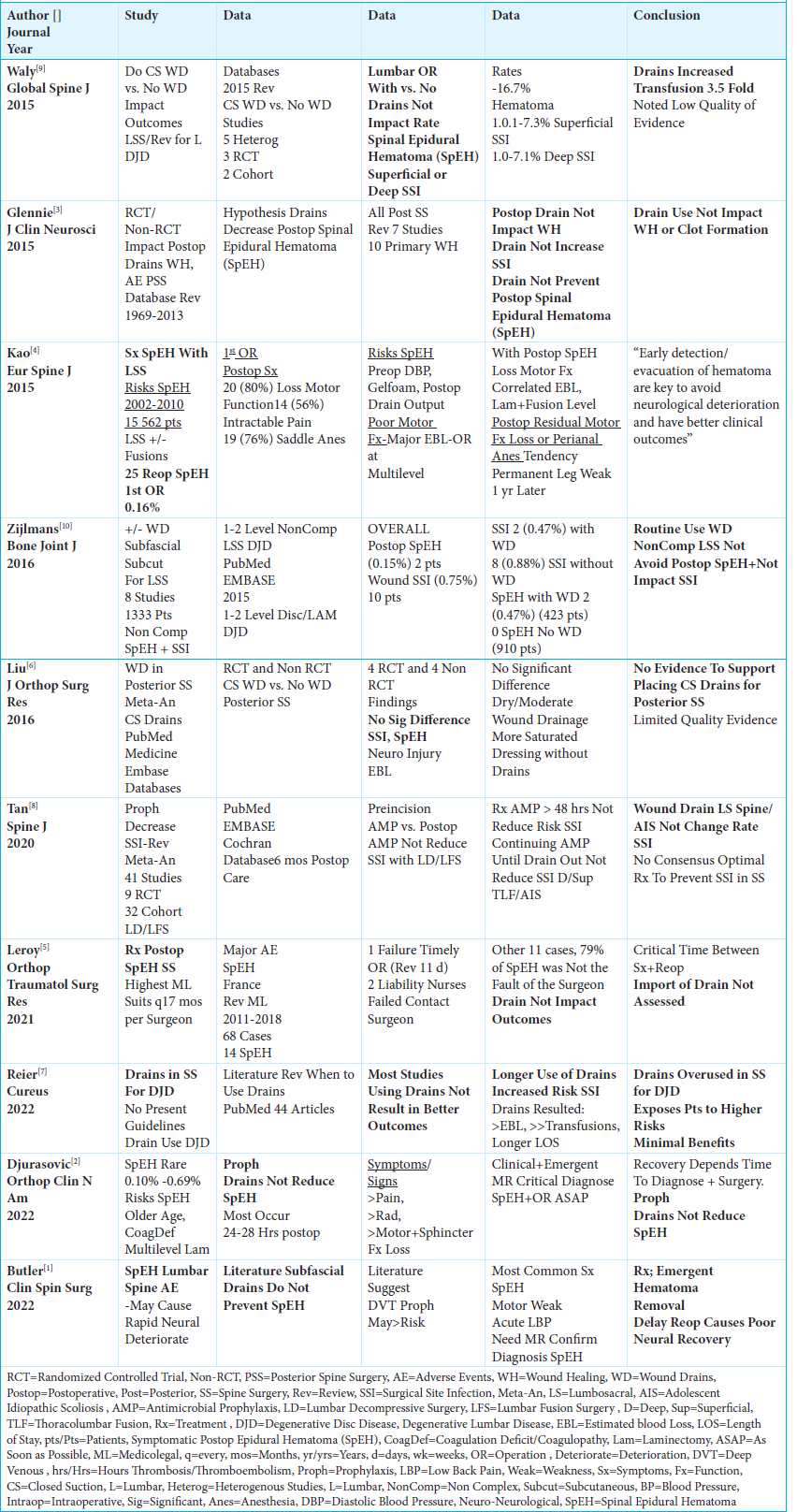
BackgroundIn this short review/perspective, we asked what the frequencies would be for both postoperative spinal epidural hematomas (SpEH) and postoperative surgical site infections (SSI) in predominantly posterior lumbar procedures performed with or without the placement of wound drains?
MethodsMany spine surgeons are trained to use wound drains to decrease the risk of postoperative SpEH, despite the potential increased risk of SSI. Alternatively, avoiding drains may increase the risk of SpEH but likely decrease the potential for SSI.
ResultsPerforming predominantly posterior lumbar procedures with or without wound drains resulted in largely comparable frequencies of postoperative spinal epidural hematomas (SpEH; range of 0.10%-0.69%) and postoperative surgical site infections (SSI: range of 0.75%-7.3%). Notably, however, two studies documented that drains increased transfusion requirements, with one study showing a prolongation of the in-hospital length of stay. Critically, these series emphasized the importance of early/emergent diagnosis (i.e., with MR) and surgical treatment of SpEH to minimize residual neurological deficits.
ConclusionHere, we showed that patients undergoing predominantly lumbar spine surgery performed with or without wound drains demonstrated comparable frequencies of postoperative SpEH and SSI. Nevertheless, spine surgeons must assess on a case-by-case basis whether, based on their education, training, and experience, placing a wound drain is appropriate for their particular patient.
Keywords: Drain Placement, Frequency of Infection, Impact of Drains, Incidence Postoperative Spinal Epidural Hematomas (SpEH), Lumbar Spine Surgery, Morbidity, No Drains, Predominant, SSI: Surgical Site Infection, Wound Drain
INTRODUCTION
A question typically raised in spine surgery is whether or not to place a wound drain. Many spine surgeons are taught that drains likely reduce the incidence of postoperative spinal epidural hematomas (SpEH), but potentially increase the risk for surgical site infections (SSI). Alternatively, without a drain, although SSI’s should typically decrease, the incidence of SpEH’s could increase. In this short review/perspective, we asked whether placing or avoiding wound drains would result in different frequencies of SpEH and SSI for patients undergoing predominantly lumbar spine surgery [
Similar Rates of Postoperative Spinal Epidural Hematomas (SpEH) and Surgical Site Infections (SSI) With or Without Drains For Predominantly Posterior Lumbar Surgery
Irrespective of whether wound drains were used, multiple series of predominantly posterior lumbar spine operations showed similar frequencies of postoperative spinal epidural hematomas (SpEH: range 0.10%-0.69%) and surgical site infections (SSI: range 0.75% - 7.3%) [
Symptom Onset and Factors Causing/Contributing to Postoperative SpEH
Two studies identified early symptomatic complaints and risk factors causing/contributing to postoperative SpEH [
Wound Drains in 2 Spine Series Increase Estimated Blood Loss (EBL)/Transfusion Requirements, and In One Study, Prolonged the Length-of-Stay
Two studies highlighted that placing wound drains for spinal procedures increased estimated blood loss, and transfusion requirements [
With SpEH, Early Diagnosis (i.e., with MR) and Emergent Treatment Critical to Minimize Residual Neurological Deficits
Multiple studies documented that early diagnosis of SpEH with MR scans and emergent treatment were critical to minimize residual neurological deficits/maximize recoveries [
Postoperative Use of Drains for Spinal Surgery for Did Not Decrease Incidence of SSI
Two series highlighted that placing wound drains for lumbar spine procedures did not impact or alter the risk of SSI [
CONCLUSION
In this short review/perspective, we showed that, with or without wound drains, patients undergoing predominantly lumbar spine surgery demonstrated similar frequencies of postoperative SpEH and SSI [
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Butler AJ, Donnally CJ, Goz V, Basques BA, Vaccaro AR, Schroeder GD. Symptomatic postoperative epidural hematoma in the lumbar spine. Clin Spine Surg. 2022. 35: 354-62
2. Djurasovic M, Campion C, Dimar 2nd JR, Glassman SD, Gum JL. Postoperative epidural hematoma. Orthop Clin North Am. 2022. 53: 113-21
3. Glennie RA, Dea N, Street JT. Dressings and drains in posterior spine surgery and their effect on wound complications. J Clin Neurosci. 2015. 22: 1081-7
4. Kao FC, Tsai TT, Chen LH, Lai PL, Fu TS, Niu CC. Symptomatic epidural hematoma after lumbar decompression surgery. Eur Spine J. 2015. 24: 348-57
5. Leroy HA, Portella T, Amouyel T, Bougeard R, Assaker R, Mourier KL. Management of symptomatic postoperative epidural hematoma in spine surgery: Medicolegal implications. Orthop Traumatol Surg Res. 2021. 107: 103024
6. Liu Y, Li Y, Miao J. Wound drains in posterior spinal surgery: A meta-analysis. J Orthop Surg Res. 2016. 11: 16
7. Reier L, Fowler JB, Arshad M, Siddiqi J. Drains in spine surgery for degenerative disc diseases: A literature review to determine its usage. Cureus. 2022. 14: e23129
8. Tan T, Lee H, Huang MS, Rutges J, Marion TE, Mathew J. Prophylactic postoperative measures to minimize surgical site infections in spine surgery: Systematic review and evidence summary. Spine J. 2020. 20: 435-47
9. Waly F, Alzahrani MM, Abduljabbar FH, Landry T, Oellet J, Moran K. The outcome of using closed suction wound drains in patients undergoing lumbar spine surgery: A systematic review. Global Spine J. 2015. 5: 479-85
10. Zijlmans JL, Buis DR, Verbaan D, Vandertop WP. Wound drains in non-complex lumbar surgery: A systematic review. Bone Joint J. 2016. 98: 984-9