- Department of Otolaryngology Head and Neck Surgery, Loma Linda University Health, California, United States
- Loma Linda University School of Medicine, Loma Linda, California, United States
- Department of Neurological Surgery, Childrens Hospital of Orange County, Orange, California, United States
Correspondence Address:
Max Feng, Department of Otolaryngology Head and Neck Surgery, Loma Linda University Health, Loma Linda, California, United States.
DOI:10.25259/SNI_674_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Max Feng1, Alexandra Vacaru2, Vikrum Thimmappa1, Brian Hanak3. Drainage of middle cranial fossa epidural abscess through mastoidectomy: Our experience and review of the literature. 25-Oct-2024;15:389
How to cite this URL: Max Feng1, Alexandra Vacaru2, Vikrum Thimmappa1, Brian Hanak3. Drainage of middle cranial fossa epidural abscess through mastoidectomy: Our experience and review of the literature. 25-Oct-2024;15:389. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13158
Abstract
Background:Otitis media (OM) can uncommonly lead to intracranial complications. Epidural abscesses represent a large proportion of cases; however, literature regarding the optimal surgical management of otogenic epidural abscesses is sparse. Favorably located epidural abscesses may be amenable to drainage through a transmastoid approach because the tegmen mastoideum lies immediately inferior to the middle cranial fossa (MCF).
Case Description:We report 3 pediatric patients with OM complicated by epidural abscesses of the MCF. The ages ranged from 3 to 6 years old, with 2 females and 1 male. All 3 patients had acute mastoiditis with an abscess of the MCF ranging from 1.6 cm to 6.3 cm at the largest dimension. All patients underwent canal wall-up mastoidectomy with the evacuation of the MCF abscess through a small window, 0.7 × 0.7 cm or less, created in the tegmen mastoideum. All patients were successfully treated through this approach and had complete resolution of their infection on follow-up imaging. There were no postoperative temporal lobe encephaloceles.
Conclusion:This is one of the few descriptions of the treatment of an otogenic epidural abscess of the MCF through a transmastoid approach. Collaboration with neurosurgery is vital because their familiarity with the intracranial space helped to guide the accurate direction of dissection. This highlights the importance of a multidisciplinary approach in the treatment of epidural intracranial abscess of the MCF through this approach. The risk of postoperative temporal lobe encephalocele was minimized due to the small tegmen defect size.
Keywords: Epidural abscess, Mastoidectomy, Middle cranial fossa, Otogenic abscess
INTRODUCTION
Otitis media (OM) can lead to both intratemporal and intracranial complications. Common intratemporal complications include mastoiditis, subperiosteal abscess, and facial nerve palsy.[
Within this subset of OM with intracranial complications, epidural abscesses represent a large proportion of cases. In a review of 33 patients with intracranial complications of OM over 8 years, 16 (48.5%) patients presented with epidural abscess. Literature regarding the optimal surgical management of otogenic epidural abscesses is sparse. The most common otologic surgical management involves canal wall up or canal wall down mastoidectomy with or without tympanostomy tube placement.[
Favorably located epidural abscesses may be amenable to drainage through a transmastoid approach, as the tegmen mastoideum lies immediately inferior to the middle cranial fossa (MCF). There are case reports of drainage of MCF, and posterior cranial fossa abscesses through violation of the tegmen mastoideum and the bony sigmoid plate during mastoidectomy, respectively.[
We report three cases of pediatric OM complicated by MCF epidural abscesses. All three patients were successfully treated with the performance of a canal wall-up mastoidectomy with abscess evacuation through a small opening in the tegmen mastoideum.
CASE PRESENTATIONS
Patient 1
History and presentation
A 3-year-old male with a history of autism, cerebral palsy, and neonatal hemiplegic seizure due to left hemispheric stroke presented with complaints of worsening left otalgia, fever, and emesis. There was no associated otorrhea, tinnitus, hearing loss, disequilibrium, loss of consciousness, or seizures.
Clinical findings and diagnostic assessment
Computed tomography imaging of the temporal bone was performed, which showed acute left otomastoiditis with a 1.6 cm epidural abscess along the left MCF and a small subperiosteal/scalp abscess. Contrast-enhanced magnetic resonance imaging (MRI) showed a 1.6 × 0.9 cm rim-enhancing epidural fluid collection within the left posterior MCF, along with a 1.0 cm rim-enhancing fluid collection within the left postauricular soft tissues [
Figure 1:
Left to right. (a) Axial T1+ magnetic resonance imaging (MRI) brain demonstrating a left middle cranial fossa epidural collection with associated regional dural enhancement. (b) Axial T1+ MRI brain on postoperative day 1 demonstrating resolution of left middle cranial fossa fluid collection with residual dural enhancement.
Therapeutic intervention and outcome
The patient was started on ceftriaxone, vancomycin, and metronidazole. They underwent canal wall-up mastoidectomy and left tympanostomy tube placement. A postauricular Palva flap was raised. The subperiosteal abscess was drained. A canal wall-up mastoidectomy was then performed, and the antrum was widely opened. Next, with neurosurgical assistance, the tegmen mastoideum was progressively thinned down with a diamond burr until the temporal dura was exposed. A small tegmen window, measuring <0.7 × 0.7 cm, was created. Blunt dissection was carried out along the floor of the MCF with a freer elevator until purulence was encountered. After evacuation and irrigation of the abscess, a Penrose drain was placed in the mastoid cavity.
A repeat brain MRI obtained the day after surgery showed near-complete abscess evacuation [
Patient 2
History and presentation
A 6-year-old female presented with fevers, ear pain, headaches, and altered mental status with cough and rhinorrhea for 6 days. She was seen at an outside clinic and prescribed Tamiflu, azithromycin, and amoxicillin. She had taken these medications for 2 days before presenting to our institution in the setting of progressive gait unsteadiness, mild confusion, emesis, diarrhea, right-sided neurologic deficits, and decreased interaction.
She was started on levetiracetam and fosphenytoin for possible seizures, as well as ceftriaxone, vancomycin, and acyclovir.
Clinical findings and diagnostic assessment
MRI Brain showed left mastoiditis with a left temporal epidural abscess measuring 4.0 × 1.6 × 3.7 cm, causing mass effect and vasogenic edema. Cerebritis of the adjacent left temporal lobe was also noted. Several smaller collections of fluid were also seen along the inferior temporal lobe and cerebellar hemisphere adjacent to the mastoid cavity [
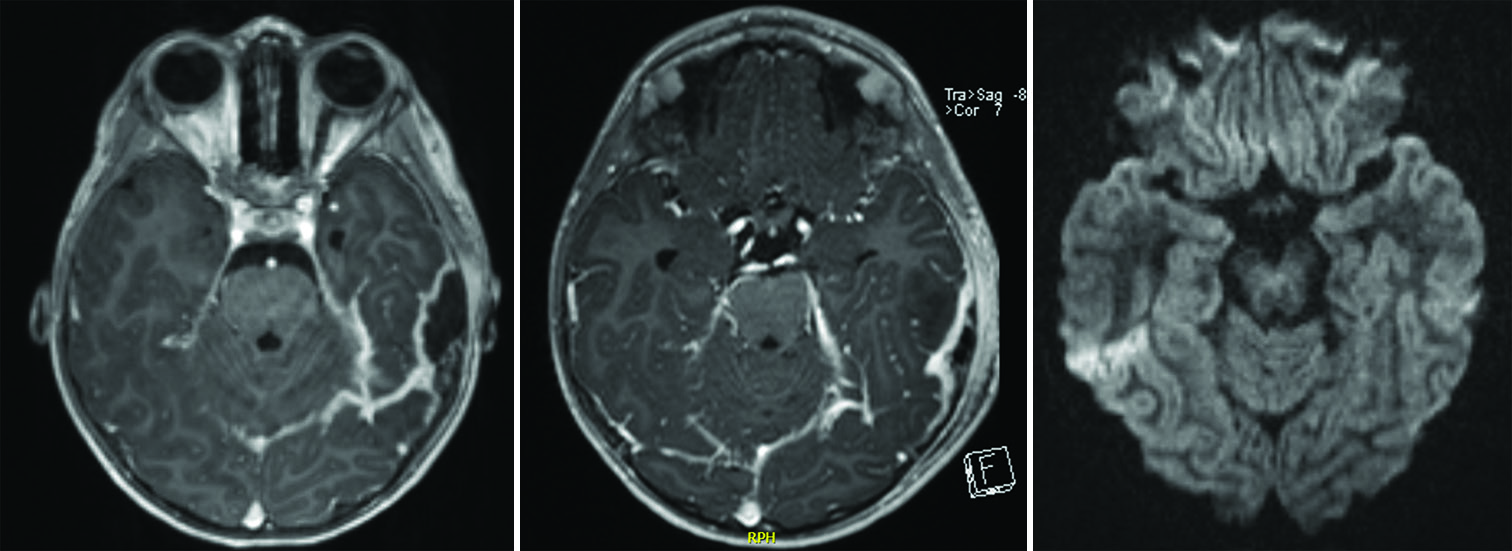
Figure 2:
Left to right. (a) Axial T1+ magnetic resonance imaging (MRI) brain demonstrating a large left epidural abscess within the middle cranial fossa. (b) Axial T1+ MRI brain on postoperative day 2 showing near-complete resolution of the left middle cranial fossa epidural fluid collection. (c) Axial diffusion-weighted imaging at 6 week postoperatively demonstrating an absence of fluid restriction at the site of the previously seen epidural fluid collection.
Therapeutic intervention and outcome
The patient underwent drainage of epidural abscess, canal wall-up mastoidectomy, and tympanostomy tube placement. A canal wall-up mastoidectomy was performed, and the antrum was widely opened. Significant granulation tissue was encountered and removed. The anterior tegmen was unroofed and widened using a curette, resulting in the discharge of a small amount of thin, purulent fluid. The neurosurgical team then bluntly explored the MCF anteriorly through the tegmen window using a number 4 Penfield. The space was irrigated with vancomycin irrigation until no purulence returned. Surgicel and a non-sutured Duragen patch were placed in the defect. Myringotomy was subsequently performed. Significant thick purulence was suctioned, and the middle ear was irrigated with vancomycin irrigation. A tympanostomy tube was placed, and ciprodex was instilled into the middle ear.
Repeat MRI on postoperative day 2 showed an interval decrease in the size of the epidural abscess to 0.8 cm [
Patient 3
History and presentation
A 3-year-old female with a history of anemia, obesity, and development delay.
She presented with right-sided facial swelling, right-ear drainage, and fever after a head injury 2 days prior and an ear infection 1-month prior that was previously treated with a 10-day course of amoxicillin.
Clinical findings and diagnostic assessment
During the initial physical examination, the patient was noted to have swelling on the right side of the face and drainage and tenderness at the right ear. MRI brain with contrast showed right OM with mastoiditis, right osteomyelitis, a small subperiosteal abscess, and an epidural abscess measuring up to 6.3 cm, occupying the middle and posterior cranial fossae [
Figure 3:
Left to right. (a) Axial T1+ magnetic resonance imaging (MRI) brain demonstrating a right epidural abscess within the middle cranial fossa. (b) Axial T1+ MRI brain on postoperative day 5 showing complete evacuation of the epidural fluid collection with expected persistent regional dural enhancement. (c) Axial T1+ MRI brain obtained 9 weeks postoperatively showed near-complete resolution of the previously seen dural enhancement and no evidence of epidural fluid collection.
Therapeutic intervention and outcome
The patient underwent canal wall-up mastoidectomy, tympanostomy tube placement, incision and drainage of subperiosteal abscess, and drainage of epidural abscess. A tympanostomy tube was first placed, with the middle ear purulent effusion evacuated. A canal wall-up mastoidectomy was performed, and the antrum was widely opened. Significant granulation tissue was removed during the mastoidectomy. A bony dehiscence was present over the right sigmoid sinus with purulence draining from the area. The opening was enlarged using a size 3 diamond burr to enhance access into the posterior fossa epidural fluid collection. The posterior fossa was then irrigated with saline. The tegmen mastoideum was thinned with a diamond burr to expose the dura. This tegmen defect was subsequently widened to slightly <0.7 × 0.7 cm in diameter. Blunt dissection was carried out in all directions toward the petrous ridge and lateral squamous temporal bone. Significant purulent material was evacuated. The middle fossa was then irrigated with saline. A quarter-inch Penrose drain was placed in the mastoid cavity.
Postoperative MRI showed decreased mass effect upon the right temporal lobe with overlying scalp cellulitis/myositis and residual small subperiosteal/scalp fluid collection [
DISCUSSION
Intracranial infections encompass a rare but challenging complication of OM. In a review of 33 patients with intracranial complications secondary to OM, the most common complications were epidural abscess (30.3%) and sigmoid sinus thrombosis (27.3%).[
The most common location of abscess formation was the epidural space. A large portion of epidural abscesses develop adjacent to the sigmoid sinus. In one study, the majority of epidural abscesses, 13 of 16 (81.2%), developed adjacent to the sigmoid sinus, followed by the MCF.[
There are scattered case reports in the literature regarding transtemporal drainage of MCF and posterior cranial fossa epidural abscesses, as opposed to the standard craniotomy or burr-hole approach. One case report described drainage of a posterior fossa abscess by drilling the posterosuperior portion of the tegmen mastoideum and entering the abscess cavity through the defect. The final size of the defect was 0.5 cm2. A residual cerebellar abscess was drained during the 3rd week through a craniotomy.[
Our study is among the few to report a transmastoid approach to drainage of an otogenic epidural abscess in discontinuity with the mastoid cavity. Each presentation arose as a sequela of advanced OM and mastoiditis. In each of our cases, the patients were young, with ages ranging from 3 to 6 years old. The size of each abscess was over 1 cm, located within the epidural space of the MCF. A canal-wall up mastoidectomy was performed, and a standard antrostomy was performed to establish communication between the mastoid cavity and the middle ear. As the lateral aspect MCF directly overlies the tegmen mastoideum, the bony plate was thinned using a coarse diamond drill burr or curette, and the middle fossa dura was encountered. In each case, the size of the tegmen defect did not exceed 0.7 × 0.7 cm. From the tegmen approach, the abscess pocket could be reached with blunt dissection. The neurosurgical team was present intraoperatively to provide assistance or to perform the dissection. We chose not to close the tegmen defect so as to allow for continued drainage of the middle fossa into the mastoid cavity. Each patient also completed a 6-week course of intravenous antibiotic therapy. All three cases were treated successfully with a single-stage approach without the need for further drainage or evidence of recurrent abscess. There were no complications noted at 6 weeks postoperatively.
The trans-mastoid approach to otogenic MCF abscesses offers an alternative approach to traditional craniotomy or burr-hole drainage in select patients. The benefits include decreased overall morbidity of surgery due to decreased operative time, single postauricular incision, and lack of need for pinning of the head. Furthermore, the establishment of communication between the mastoid and middle fossa epidural space allows for gravity-dependent egress of any residual fluid and potentially reduces the risk of abscess recurrence. We pursued surgical intervention in abscesses over 1 cm in size. It is unclear regarding the maximal size of the abscess drainable through the tegmen, though the largest abscess drained measured 6.3 cm in size. We also recommend the close involvement of pediatric neurosurgery colleagues, as their familiarity with the intracranial space helped to guide accurate direction of dissection towards the abscess cavity.
We recommend that the transmastoid approach should be limited to cases where the fluid collection is located in the MCF epidural space. A careful review of imaging should be performed to select cases in which dissection towards the fluid collection is relatively straightforward and limited. In cases in which difficult access through a <1 × 1 cm tegmen window is anticipated, we advise against this approach to limit the risk of dural perforation or venous bleeding. For small abscesses, <1 cm or multi-loculated abscesses, intraoperative neuronavigation may be considered, although this was not used in any of our cases.
Limitations of this approach include the increased risk of development of delayed temporal lobe encephalocele with leaving an open tegmen defect. These are rare. Between 1950 and 1998, there were only 177 reported cases of meningocele and meningoencephalocele, with the majority following mastoidectomy. In a six-patient case series of patients with delayed temporal lobe encephaloceles following trauma, mastoidectomy, or cholesteatoma, five out of six of the bony defects were 1.0 × 1.0 cm or greater.[
A potential limitation of accessing the intracranial space through a small tegmen window is suboptimal exposure of the MCF and difficult access to the area of infection. However, epidural abscesses are confined within spaces of dural adherence to suture lines and can be successfully managed with limited exposure techniques compared to deeper infections, such as subdural empyema.[
Author’s contributions
MF was responsible for project design, manuscript preparation, and manuscript editing. AV was responsible for manuscript preparation and manuscript editing. BH was responsible for project design and manuscript editing. VT was responsible for project design and manuscript editing.
CONCLUSION
A transmastoid approach through the tegmen provides an alternative approach to otogenic epidural abscesses of the MCF. Collaboration between pediatric otolaryngology and neurosurgery can allow for a single-stage surgery without the need for craniotomy or burr-hole drainage that is both safe and efficacious.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Block SL, Harrison CJ, Hedrick JA, Tyler RD, Smith RA, Keegan E. Penicillin-resistant Streptococcus pneumoniae in acute otitis media: risk factors, susceptibility patterns and antimicrobial management. Pediatr Infect Dis J. 1995. 14: 751-9
2. Duygu E, Şevik Eliçora S. Our experience on the management of acute mastoiditis in pediatric acute otitis media patients. Int J Pediatr Otorhinolaryngol. 2020. 138: 110372
3. Go C, Bernstein JM, de Jong AL, Sulek M, Friedman EM. Intracranial complications of acute mastoiditis. Int J Pediatr Otorhinolaryngol. 2000. 52: 143-8
4. Goldstein NA, Casselbrant ML, Bluestone CD, Kurs-Lasky M. Intratemporal complications of acute otitis media in infants and children. Otolaryngol Head Neck Surg. 1998. 119: 444-54
5. Hafidh MA, Keogh I, Walsh RM, Walsh M, Rawluk D. Otogenic intracranial complications. A 7-year retrospective review. Am J Otolaryngol. 2006. 27: 390-5
6. Heran NS, Steinbok P, Cochrane DD. Conservative neurosurgical management of intracranial epidural abscesses in children. Neurosurgery. 2003. 53: 893-7
7. Hlavin ML, Kaminski HJ, Fenstermaker RA, White RJ. Intracranial suppuration: A modern decade of postoperative subdural empyema and epidural abscess. Neurosurgery. 1994. 34: 974-80
8. Isaacson B, Mirabal C, Kutz JW, Lee KH, Roland PS. Pediatric otogenic intracranial abscesses. Otolaryngol Head Neck Surg. 2010. 142: 434-7
9. Kangsanarak J, Fooanant S, Ruckphaopunt K, Navacharoen N, Teotrakul S. Extracranial and intracranial complications of suppurative otitis media. Report of 102 cases. J Laryngol Otol. 1993. 107: 999-1004
10. Lundy P, Kaufman C, Garcia D, Partington MD, Grabb PA. Intracranial subdural empyemas and epidural abscesses in children. J Neurosurg Pediatr. 2019. 24: 14-21
11. Mattos JL, Colman KL, Casselbrant ML, Chi DH. Intratemporal and intracranial complications of acute otitis media in a pediatric population. Int J Pediatr Otorhinolaryngol. 2014. 78: 2161-4
12. Migirov L, Duvdevani S, Kronenberg J. Otogenic intracranial complications: A review of 28 cases. Acta Otolaryngol. 2005. 125: 819-22
13. Morwani KP, Jayashankar N. Single stage, transmastoid approach for otogenic intracranial abscess. J Laryngol Otol. 2009. 123: 1216-20
14. Park H, Jang H, Shim D, Shin H, Ahn J, Shin J. Surgical management of acute mastoiditis with epidural abscess. Acta Otolaryngol. 2006. 126: 782-4
15. Penido NO, Borin A, Iha LC, Suguri VM, Onishi E, Fukuda Y. Intracranial complications of otitis media: 15 years of experience in 33 patients. Otolaryngol Head Neck Surg. 2005. 132: 37-42
16. Sexton GP, Nae A, Cleere EF, O’Riordan I, O’Neill JP, Lacy PD. Concurrent management of suppurative intracranial complications of sinusitis and acute otitis media in children. Int J Pediatr Otorhinolaryngol. 2022. 156: 111093
17. Souliere CR, Langman AW. Combined mastoid/middle cranial fossa repair of temporal bone encephalocele. Skull Base Surg. 1998. 8: 185-9
18. Sun J, Sun J. Intracranial complications of chronic otitis media. Eur Arch Otorhinolaryngol. 2014. 271: 2923-6
19. Van der Poel NA, van Spronsen E, Dietz de Loos DA, Ebbens FA. Early signs and symptoms of intracranial complications of otitis media in pediatric and adult patients: A different presentation?. Int J Pediatr Otorhinolaryngol. 2017. 102: 56-60
20. Voudouris C, Psarommatis I, Nikas I, Kafouris D, Chrysouli K. Pediatric masked mastoiditis associated with multiple intracranial complications. Case Rep Otolaryngol. 2015. 2015: 897239
21. Wanna GB, Dharamsi LM, Moss JR, Bennett ML, Thompson RC, Haynes DS. Contemporary management of intracranial complications of otitis media. Otol Neurotol. 2010. 31: 111-7
22. Zapalac JS, Billings KR, Schwade ND, Roland PS. Suppurative complications of acute otitis media in the era of antibiotic resistance. Arch Otolaryngol Head Neck Surg. 2002. 128: 660-3
23. Zevallos JP, Vrabec JT, Williamson RA, Giannoni C, Larrier D, Sulek M. Advanced pediatric mastoiditis with and without intracranial complications. Laryngoscope. 2009. 119: 1610-5