- Department of Neurosurgery, Educational-Surgical Clinic by the Medical University of Azerbaijan, Azerbaijan, Iraq,
- Department of Neurosurgery, Medical University of Azerbaijan, Baku, Azerbaijan, Iraq,
- Department of Neurosurgery, University of Baghdad, College of Medicine, Baghdad, Iraq,
- Department of Neurosurgery, University of Cincinnati, Cincinnati, United States.
Correspondence Address:
Samer S. Hoz, Department of Neurosurgery, University of Cincinnati, Cincinnati, United States.
DOI:10.25259/SNI_658_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Rauf Sadiqo1, Alkawthar M. Abdulsada2, Mustafa Ismail3, Samer S. Hoz4. Ectopic schwannoma of the sellar region in a 1-year-old child: A case report and review of literature. 23-Sep-2022;13:438
How to cite this URL: Rauf Sadiqo1, Alkawthar M. Abdulsada2, Mustafa Ismail3, Samer S. Hoz4. Ectopic schwannoma of the sellar region in a 1-year-old child: A case report and review of literature. 23-Sep-2022;13:438. Available from: https://surgicalneurologyint.com/surgicalint-articles/11880/
Abstract
Background: Schwannomas are cranial and spinal nerves’ sheath tumors accounting for up to 8% of all intracranial neoplasms. Although typical intracranial schwannomas originate from Schwann cells surrounding cranial nerves, ectopic schwannomas are not associated with a known cranial nerve or have an unknown origin. The location of schwannomas may impose clinical challenges. Sellar region schwannomas are rare whether it is ectopic or not. Herein, we report a pediatric case of a 1-year-old female with ectopic, intra-supra sellar with a literature review. We report the first case of juvenile ectopic schwannoma in the sellar region.
Methods: A PubMed Medline database search was performed by the following combined formula of medical subject headings (MESH) terms and keywords: ((sella turcica [MeSH Terms]) OR (sella*[Title/Abstract]) OR (ectopic [Title/Abstract]) AND ((neurilemmoma [MeSH Terms]) OR (schwannoma [Title/Abstract]) OR (neuroma [Title/Abstract]) OR (neurinoma [Title/Abstract])).
Results: Total results of 206 articles were obtained. In exclusion of intraparenchymal and intraventricular schwannomas, only 34 articles remained. Thirty-nine cases were included in 34 articles. According to the reported cases, intrasellar schwannomas are more common in elderly individuals in an average of 49.5 years (range: 19– 79 years). They have a good prognosis and affect males to females equally (20:19).
Conclusion: Ectopic schwannoma sited in the sellar region is rare. It is the first case to be reported in the pediatric age group with a literature review. This lesion should be highlighted and included in the differential diagnosis of sellar mass.
Keywords: Ectopic schwannoma, Neuroma, Pediatric, Sellar tumors
INTRODUCTION
Schwannomas are common cranial and spinal nerves’ sheath tumors representing up to 8% of all intracranial neoplasms.[
Herein, we report a pediatric case of a 1-year-old female with ectopic, intra-supra sellar, relatively large schwannoma associated with severe visual impairments, weakness, and endocrine disturbances. She was treated with a subtotal tumorectomy and followed up for 1 year. Good prognosis and noticed improvement of visual and endocrine states proved by postoperative examination. In addition, we conducted a review of all sellar schwannomas reported in the literature.
CASE SCENARIO
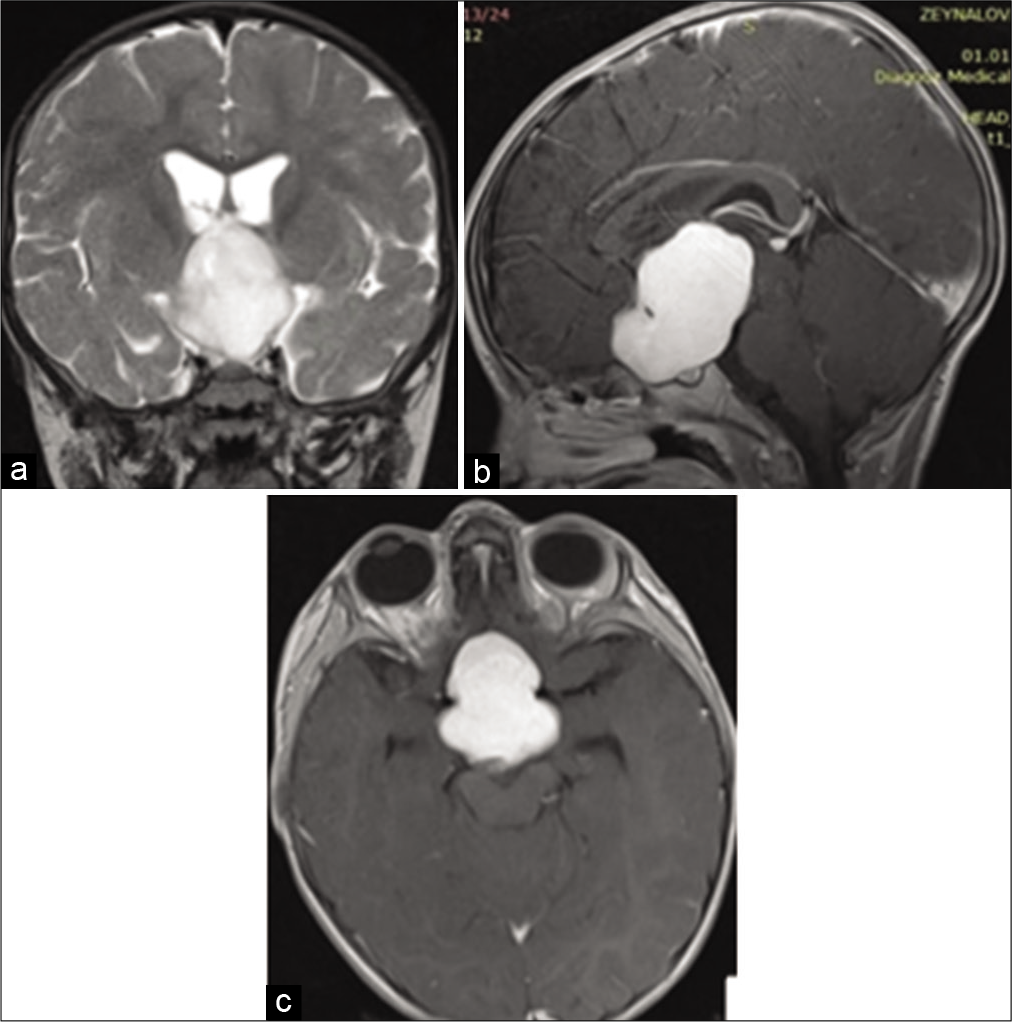
A 1-year-old female was admitted to our hospital with complaints of severe visual impairments in both eyes, strabismus, weakness, and vomiting. She also had endocrinal disturbances, including hyperthyroidism (Free thyroxine: 26.08 pmol/L and free triiodothyronine: 8.08 pmol/L). Preoperative Magnetic Resonance Imaging (MRI) [
Figure 1:
Preoperative magnetic resonance image: (a) T2-weighted image (coronal section) demonstrates hyperintense mass localized in the sella and extending to the suprasellar area, compressing the third ventricle. (b) T1-weighted image (B: sagittal), a contrast-enhanced image of the brain showing homogenous enhancement of the lesion. (c) T1-weighted image (axial section), contrast-enhanced image showing homogenous enhancement of the mass.
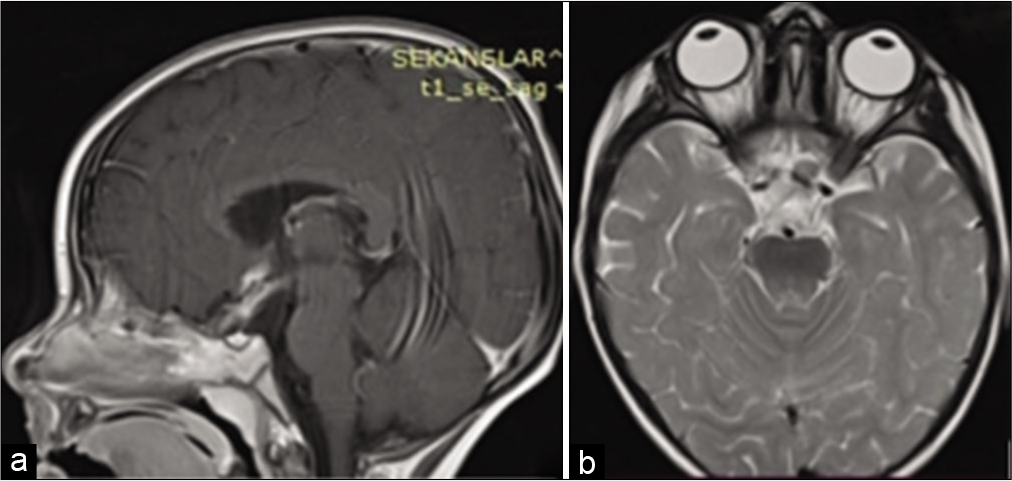
The patient underwent transcranial tumorectomy with a right-sided pterional approach. Subtotal removal of a rubbery high vascularized mass was achieved, and no postoperative complications were exacerbated. She had gradual improvement of vision and endocrine function postoperatively and regained full vision within 1 year of follow-up [
Figure 2:
One-year follow-up magnetic resonance image: (a) T1-weighted image (sagittal section), affirm successful tumorectomy and decompression of optic chiasm with normal ventricular volume. (b) T2-weighted image (axial section), confirm successful tumorectomy and decompression of optic chiasm with no dilatation of the ventricles.
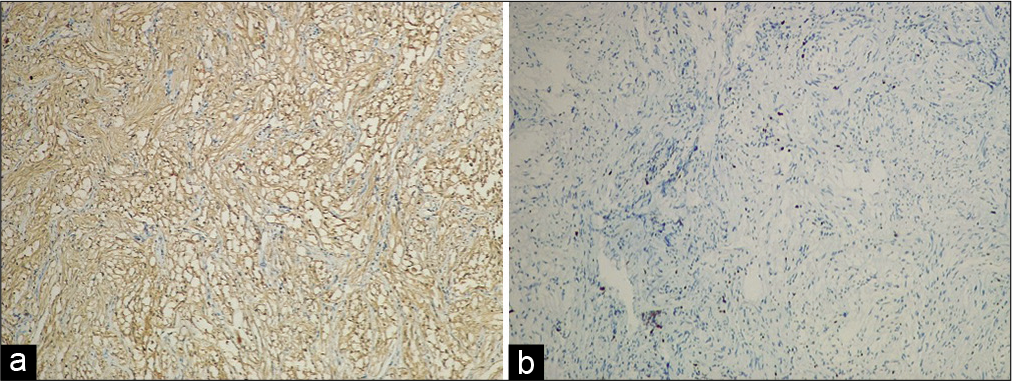
Figure 3:
(a) A histopathological image shows spindle cells with immunostaining that is positive staining for S-100 protein and negative for glial fibrillary acidic protein and epithelial membrane antigen. It is consistent with Schwannoma, the WHO Grade 1. (b) A histopathological image of Schwannoma with nuclear expression of Ki67 proliferation index was observed in approximately 2–3% of cells.
METHODS
We conducted a PubMed Medline database search by the following combined formula of medical subject headings (MESH) terms and keywords: ((sella turcica [MeSH Terms]) OR (sella*[Title/Abstract]) OR (ectopic [Title/Abstract]) AND ((neurilemmoma [MeSH Terms]) OR (schwannoma [Title/Abstract]) OR (neuroma [Title/Abstract]) OR (neurinoma [Title/Abstract])).
RESULTS
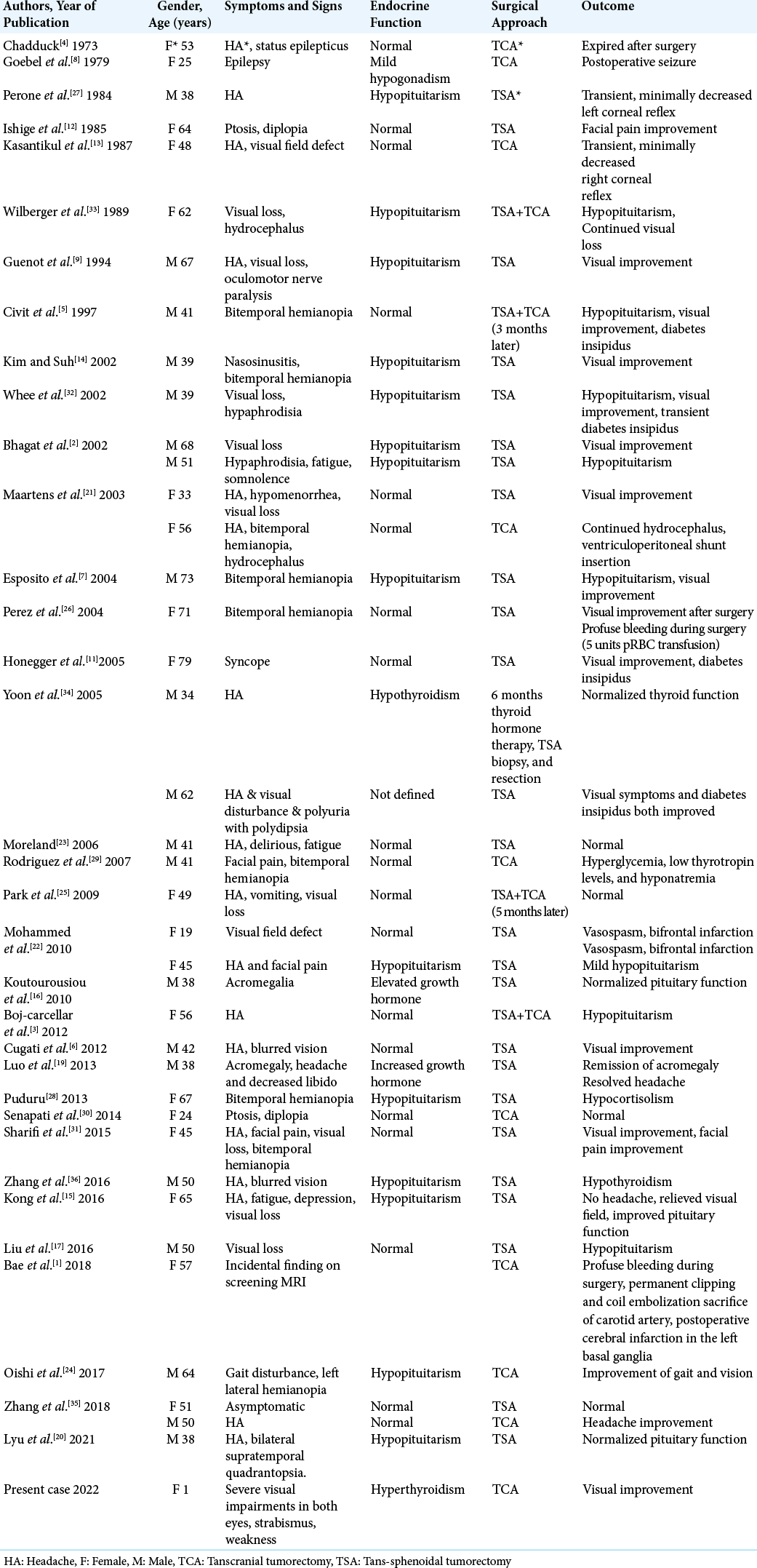
A total of 206 results were obtained, and by the exclusion of intraparenchymal and intraventricular schwannomas, only 34 articles remained. Thirty-nine cases were included in 34 articles. According to the reported cases [
DISCUSSION
The significant preponderance of sellar lesions is for PAs. Other nonadenomatous sellar lesions include neoplastic, cystic, and inflammatory lesions.[
The clinical presentation of sellar schwannomas is represented by the triad: headache, visual disturbances, and endocrinal dysfunction; most commonly hypopituitarism which is believed to be a result of pituitary stalk and portal vessels compression.[
Although schwannomas are benign tumors of children and adults, sellar schwannomas have not been reported in pediatrics yet. Our case is the first juvenile intra-suprasellar schwannoma, and the clinical presentation is the same with adults, in addition to weakness and vomiting.
According to their origin, schwannomas are peripheral nervous system tumors arising from Schwann cells ensheathing peripheral axons of all cranial nerves except the optic nerve (CN II). Their most common sites are associated with the vestibulocochlear nerve (CN VIII) in acoustic neuroma, second with the trigeminal nerve (CN V).[
In our literature review, Chadduck, in 1973, first reported the case of a 53-year-old female who presented with a headache; then, she developed an attack of status epilepticus. Her management included transcranial tumorectomy (TCA); nevertheless, she expired postoperatively. Thirty-eight cases then were followed in the reporting of this pathology. None of the reported cases were within the pediatric age group, and the youngest person was 19-year-old, and the case was reported by Mohammed et al. 2010. The current case is the first to be reported as an infant and within the pediatric age group.
In summary, a 53-year-old female presented with visional impairment and vomiting. Her imaging showed a mass in the sellar region. The surgery was considered, and a TCA was performed. In the follow-up period, the patient fully recovered in the vision and endocrine function in 1 year. This case is unique and solo as it is the first juvenile ectopic schwannoma.
CONCLUSION
Ectopic schwannoma located in the sellar region is rare. It is the first case to be reported in the pediatric age group with a literature review. This pathology should be included in the differential diagnosis of the mass in the sellar region, particularly when the radiological features of the mass are suspicious.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bae S, Ahn SS, Chang JH, Kim SH. Intra-suprasellar schwannoma presumably originating from the internal carotid artery wall. Clin Neuroradiol. 2018. 28: 127-35
2. Bhagat S, Smith C, Teasdale GM, McFadzean RM. Nerve sheath tumors of the sellar region. J Neuroophthalmol. 2002. 22: 275-8
3. Carceller DB, Gamboa RA, Sanz GV, Arregui SV, Alegret RA. Intrasellar schwannoma: A rare case of pituitary incidentaloma. Endocrinol Nutr. 2012. 59: 336-8
4. Chadduck WM. Unusual lesions involving the sella turcica. South Med J. 1973. 66: 948-55
5. Civit T, Pinelli C, Klein M, Auque J, Baylac F, Hepner H. Intrasellar schwannoma. Acta Neurochir. 1997. 139: 160-1
6. Cugati G, Singh M, Symss NP, Pande A, Yasha TC, Vasudevan MC. Primary intrasellar schwannoma. J Clin Neurosci. 2012. 19: 1584-5
7. Esposito F, Cappabianca P, De Caro MD, Cavallo LM, Rinaldi C, De Divitiis E. Endoscopic endonasal transsphenoidal removal of an intra-suprasellar schwannoma mimicking a pituitary adenoma. Minim Invasiv Neurosurg. 2004. 47: 230-4
8. Goebel HH, Shimokawa K, Schaake TH, Kremp A. Schwannoma of the sellar region. Acta Neurochir. 1979. 48: 191-7
9. Guenot M, Bataille B, Wager M. Intrasellar neurinoma. Apropos of a case and review of the literature. Neurochir. 1994. 40: 263-6
10. Hilton DA, Hanemann CO. Schwannomas and their pathogenesis. Brain Pathol. 2014. 24: 205-20
11. Honegger J, Koerbel A, Psaras T, Petrick M, Mueller K. Primary intrasellar schwannoma: Clinical, aetiopathological and surgical considerations. Br J Neurosurg. 2005. 19: 432-8
12. Ishige N, Ito C, Saeki N, Oka N. Neurinoma with intrasellar extension: A case report. No Shinkei Geka Neurol Surg. 1985. 13: 79-84
13. Kasantikul V, Shuangshoti S, Preechayudh P, Wangsuphachart S. A combined neurilemmoma and angioma of the parasellar region: Case report. J Neurosurg. 1987. 67: 307-11
14. Kim NR, Suh YL. Primary intrasellar schwannoma: A case report. Korean J Pathol. 2002. 36: 274-7
15. Kong X, Wu H, Ma W, Li Y, Yang Y, Xing B. Schwannoma in sellar region mimics invasive pituitary macroadenoma: Literature review with one case report. Medicine (Baltimore). 2016. 95: e2931
16. Koutourousiou M, Kontogeorgos G, Wesseling P, Grotenhuis AJ, Seretis A. Collision sellar lesions: Experience with eight cases and review of the literature. Pituitary. 2010. 13: 8-17
17. Liu M, Ouyang YU, Lv F. Computed tomography and magnetic resonance imaging findings of intrasellar schwannoma: A case report and literature review. Oncol Lett. 2016. 11: 2315-9
18. Liu X, Deng J, Xue C, Li S, Zhou J. Ectopic schwannoma of the lateral ventricle: Case report and review of the literature. Acta Neurol Belg. 2021. 121: 801-5
19. Luo W, Ren X, Chen S, Liu H, Sui D, Lin S. Intracranial intraparenchymal and intraventricular schwannomas: Report of 18 cases. Clin Neurol Neurosurg. 2013. 115: 1052-7
20. Lyu J, Quan Y, Wang JB, Gong SP. Primary intrasellar schwannoma with intratumoral hemorrhage mimicking pituitary apoplexy: A case report. Neurochirurgie. 2021. 67: 491-4
21. Maartens NF, Ellegala DB, Vance ML, Lopes MB, Laws ER. Intrasellar schwannomas: Report of two cases. Neurosurgery. 2003. 52: 1200-6
22. Mohammed S, Kovacs K, Munoz D, Cusimano MD. A short illustrated review of sellar region schwannomas. Acta Neurochir (Wien). 2010. 152: 885-91
23. Moreland DB. Intrasellar pituitary schwannoma. J Clin Neurosci. 2006. 13: 771-4
24. Oishi T, Takehara S, Yamamura Y, Tomida M, Ito S, Kuriki K. “Pure” suprasellar schwannoma presented with communicating hydrocephalus: A case report. NMC Case Rep J. 2017. 4: 83-7
25. Park HW, Jung S, Jung TY, Moon KS. Intra-suprasellar schwannoma originating from the diaphragma sellae. J Korean Neurosurg Soc. 2009. 45: 375-7
26. Perez MT, Farkas J, Padron S, Changus JE, Webster EL. Intrasellar and parasellar cellular schwannoma. Ann Diagn Pathol. 2004. 8: 142-50
27. Perone TP, Robinson B, Holmes SM. Intrasellar schwannoma: Case report. Neurosurgery. 1984. 14: 71-3
28. Puduru SS. Intrasellar schwannoma mimicking pituitary adenoma. Indian J Neurosurg. 2013. 2: 213-5
29. Rodriguez FJ, Atkinson JL, Giannini C. Massive sellar and parasellar schwannoma. Arch Neurol. 2007. 64: 1198-9
30. Senapati SB, Mishra SS, Das S, Parida DK. Giant oculomotor nerve schwannoma presenting as a sellar and suprasellar mass with parasellar extension. Neurol India. 2014. 62: 548-9
31. Sharifi G, Bakhtevari MH, Alghasi M, Saberi M, Dehghan M, Bidari F. Hard calcified intrasellar schwannoma mimicking pituitary adenoma: A case report and review of the literature. Clin Neurol Neurosurg. 2015. 137: 38-43
32. Whee SM, Lee JI, Kim JH. Intrasellar schwannoma mimicking pituitary adenoma: A case report. J Korean Med Sci. 2002. 17: 147-50
33. Wilberger JE. Primary intrasellar schwannoma: Case report. Surg Neurol. 1989. 32: 156-8
34. Yoon WS, Park IS, Baik MW. Intrasellar schwannomas. J Korean Neurosurg Soc. 2005. 37: 157-9
35. Zhang C, Li G, Sun Y, Huang H. Case report schwannoma in sellar region: Report of two cases and a literature review. Int J Clin Exp Med. 2018. 11: 8733-40
36. Zhang J, Xu S, Liu Q, Li X, Jia D, Li G. Intrasellar and suprasellar schwannoma misdiagnosed as pituitary macroadenoma: A case report and review of the literature. World Neurosur. 2016. 96: 612.e1-7