- Loma Linda University School of Medicine, Loma Linda, United States
- Department of General Surgery, Division of Pediatric Surgery, Loma Linda University Health, Loma Linda, United States
- Department of Neurosurgery, Division of Pediatric Neurosurgery, Loma Linda University Health, Loma Linda, United States
Correspondence Address:
Tanya Minasian, Associate Professor of Neurosurgery, Department of Neurosurgery, Division of Pediatric Neurosurgery, Loma Linda University Health, Loma Linda, United States.
DOI:10.25259/SNI_717_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jessica Sawaya1, Joyce J. L. H. McRae2, Georgi Mladenov2, Joseph Michael Larson1, Andrei Radulescu2, Tanya Minasian3. Effect of COVID-19 on pediatric gunshot wounds to the head at a level 1 trauma center. 08-Nov-2024;15:405
How to cite this URL: Jessica Sawaya1, Joyce J. L. H. McRae2, Georgi Mladenov2, Joseph Michael Larson1, Andrei Radulescu2, Tanya Minasian3. Effect of COVID-19 on pediatric gunshot wounds to the head at a level 1 trauma center. 08-Nov-2024;15:405. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13210
Abstract
Background: The United States (US) has one of the highest rates of gunshot-related incidents in the world. Gunshot wounds to the head (GSWH) in the pediatric population are also common, with high morbidity and mortality rates.
Methods: We performed a retrospective study to analyze if there was a notable change in trends in pediatric GSWH at our Level 1 Pediatric Trauma Center due to the COVID-19 pandemic. A retrospective study was conducted including patients under the age of 18 presenting with GSWH from January 2014 to May 2023. Variables assessed included demographics, interventions, and outcomes. Data from the county’s Child Death Review Team Annual Report on mortality related to gunshot-related deaths from January 2014 to June 2023 were analyzed.
Results: In total, thirty-five patients were evaluated at our institution for GSWH. Nineteen patients were treated during the 6 years before the pandemic and sixteen during the 3-year pandemic. Nine patients died at the hospital, with an overall increase during the pandemic. In the county, seventy-two children were killed from gun violence, with 58% (42) from GSWH. Death from GSWH increased in the county cohort during the pandemic.
Conclusion: The pandemic affected the outcomes of patients with GSWH at our institution with an overall increase in rates of self-inflicted and drive-by shootings, a doubling of neurosurgical interventions, an increase in acuity of care for long-term disposition, and an increase in mortality. At a county level, there was an increase in overall deaths from GSWHs, the majority of which were nonaccidental.
Keywords: COVID-19 pandemic, Gunshot wound to the head, Pediatric trauma
INTRODUCTION
The United States (US) has the highest rate of gunshot-related deaths in all age groups among high-income countries.[
The COVID-19 pandemic was a new major stressor that had a negative impact on children and may have amplified firearm-related injuries. Stay-at-home mandates and school closures precipitated feelings of loneliness, anxiety, depression, and increased tension at home.[
The pandemic proved to be especially burdensome to low-income and violence-prone communities. San Bernardino County is a diverse geographic and socioeconomic landscape that includes populations of low socioeconomic status (SES), remote living conditions, and poor healthcare access.[
MATERIALS AND METHODS
Following Institutional Review Board approval [IRB# 5230304], we identified and analyzed the cases of children up to 18 years of age who presented to our hospital with GSWH between January 2014 and May 2023. Patient data collection included demographics, prehospital course, presentation, resuscitation efforts, incident details, interventions, length of hospital stay, mortality, and organ donation in those who died.
To understand the greater problem in our county, we also obtained data from the Children’s Network Child Death Review Team Annual Report regarding all GSW-related pediatric mortalities from January 2014 to June 2023 in San Bernardino County. Variables available through this data include the date of the accident, the age of the victim, the location of GSW on the body, and whether the context of the GSW was an accident, homicide, or suicide. We isolated GSWHs from this data and analyzed the total number of pediatric GSWH deaths and their patterns in relation to the COVID-19 pandemic.
RESULTS
Hospital cohort overview
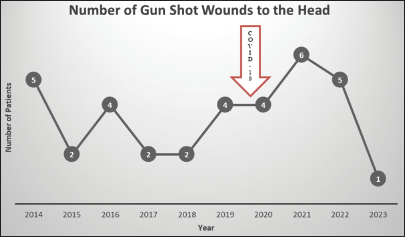
Our total hospital cohort of pediatric patients with GSWH was 35. Nineteen patients were cared for in the 6 years before the pandemic, from January 2014 to December 2019. Sixteen were treated from January 2020 to May 2023 [
Hospital cohort demographics
The average age of our patients was 13 years, with a range of 2–17. The average age increased from 13.1 before the pandemic to 14.7 during the pandemic. We found that most patients were male: 82.8%. As for insurance status, two patients did not have health insurance, two had private insurance, twenty-five had Medicaid or Medical, and six had a Health Maintenance Organization.
Hospital cohort incident location and timing
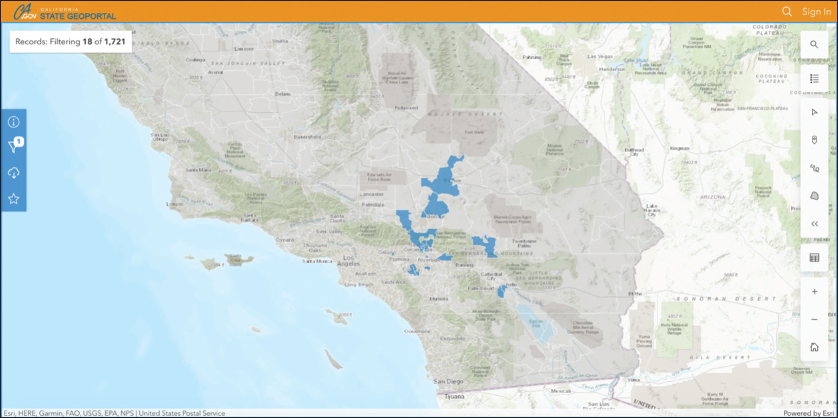
The site of the incident occurred at 18 different zip codes, spanning three counties [
Before the pandemic, 74% of incidents occurred between the hours of 6 pm and midnight. During the pandemic, this increased to 80%.
Hospital cohort incident intention and background
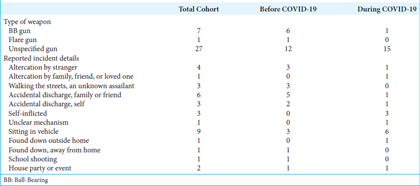
From patient, family, or social work reports, information regarding the details of the shooting was abstracted. Before the pandemic, 31% (6) of GSWH were from Ball-Bearing (BB) guns. In addition, 37% (7) of shootings were accidental during this time, with 5 occurring from accidental discharges by family or friends and 2 due to accidental discharge by self. One patient was shot during a school shooting. Other common causes were an altercation with a stranger (3), an unknown assailant on the street (3), and an unknown assailant while in a car (3). There were no self-inflicted GSWHs in the prepandemic cohort.
During the pandemic, the total amount of accidental shootings decreased, with 13% (2) of all patients presenting after accidents. Most incidents during the pandemic, or 38% (6), were related to assault by an unknown assailant while sitting in a vehicle. The percentage of self-inflicted incidents was 19% (3). The number of GSWH while sitting in a vehicle doubled from three to six, while being shot outside on the street by an unknown assailant predominantly occurred before the pandemic with three victims [
Hospital cohort means of arrival
Nearly 60% (21) of our patients were transferred from outside hospitals. Before the pandemic, 63% (12) of patients were transferred, with only a slight decrease to 56% (9) of patients during the pandemic [
Hospital cohort arrival Glasgow Coma Scale (GCS)
Prepandemic, 21% (4) of patients arrived with an initial GCS of 3 and 53% (10) with a GCS of 15. During the pandemic, 50% (8) of patients arrived with a GCS of 3 and 19% (3) with a GCS of 15. In summary, there was an overall decrease in the number of patients presenting with a GCS of 15 between the cohorts, and there was an increase in patients with a GCS of 3, suggesting an increase in injury severity [
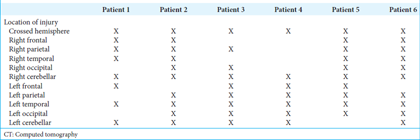
Hospital computed tomography review
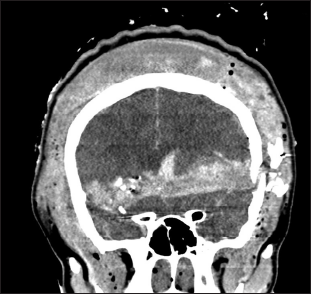
For the majority of patients who arrived, 77% (27) underwent computed tomography of the head (CTH). Of the patients who eventually died as a result of their injuries, only 67% (6) underwent a CTH [
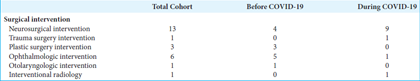
Hospital surgical intervention
Neurosurgical intervention was required in 37% (13) of the total cohort. Before the pandemic, 21% (4) of patients required a neurosurgical intervention, which more than doubled to 56% (9) of patients during the pandemic. Ophthalmology and plastic surgery interventions primarily occurred before the pandemic [
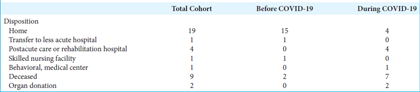
Hospital length of stay and disposition
Before the pandemic, the majority, or 79% (15) of patients’ length of stay was <1 week. Prolonged stays of up to 1 month occurred in ~11% (2) and >1 month in 5% (1). During the pandemic, the rate of prolonged hospital stays increased. Just over half of patients, or 56% (9), were admitted for less than a week, while 25% (4) stayed for up to 1 month and 13% (2) for over 1 month.
There was a notable change in disposition between cohorts. For GSWH before the pandemic, 79% (15) of patients were discharged home. This decreased to only 25% (4) of patients during the pandemic. In addition, 25% (4) were discharged to a postacute care rehabilitation hospital and 6% (1) to a behavioral medical center. The remainder of the pandemic cohort, or 44% (7), died from their injuries. Of the seven patients who died, two became organ donors. During the pandemic, the rate of mortality from GSWH more than tripled [
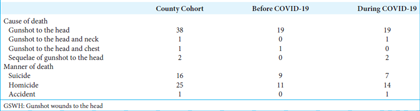
County cohort data
During the 9 years from January 2014 to June 2023, 72 children were killed by all forms of gun violence in the county of San Bernardino. Of the 72 deaths, 42 deaths, or 58%, resulted from GSWH. Twenty deaths occurred over the 6 years from January 2014 to December 2019, and twenty-two deaths occurred over the 3.5 years from January 2020 to June 2023. Overall, 38% (16) of GSWH deaths were a result of self-inflicted injury, and 60% (25) were classified as homicide.
Before the pandemic, 45% (9) of children were killed by self-infliction, while during the pandemic, that decreased to 32% (6) of deaths. Homicide accounted for 55% (11) of deaths before the pandemic and 64% (14) of deaths after. One patient was killed during the pandemic because of an accident [
DISCUSSION
In the US, unintentional injury is the number one cause of death in the pediatric population and the fourth cause of death in those under 1 year old.[
Our hospital’s data reveal an exacerbation in the prevalence and severity of pediatric GSWH during the COVID-19 pandemic. Multiple studies have reported increased rates of firearm-related injuries, child-involved shootings, and firearm homicides during the same period.[
The demographic patterns examined in this study resemble national patterns associated with GSW violence. Of those treated for GSWH at our hospital, 83% were male. In addition, 71% of patients had Medicaid or Medi-Cal coverage, suggesting lower SES. These patterns are consistent with nationwide firearm violence reports citing >83% male involvement accompanied by high rates of government-funded insurance plans.[
The negative impacts exerted by COVID-19 on the general population were pronounced in children and may explain the rise in GSWH in this age group. Stay-at-home mandates introduced feelings of loneliness, fear, and worry surrounding personal safety and well-being, including economic concerns and financial stress that impacted the entire household.[
Aside from mental and physical health, additional challenges may have contributed to the heightened prevalence of GSWH during the pandemic. Increased use of psychoactive or illicit substances coupled with limited access to detoxification centers added to rising psychological distress, ultimately leading to more deviant and violent behavior.[
GSW injuries contribute to the burden of communities beyond mortality alone. Consequences include disabilities involving premature physeal arrest, long-term bullet retention, paralysis, survivor’s guilt, and mental illness.[
Increased stress experienced during the pandemic, compounded by increased firearm purchases and 1st-time gun ownership rates, may explain the rise in pediatric GSWH during this period. Efforts to combat this growing problem have focused on legislative reform, as states with stronger gun laws demonstrate decreased child-involved shooting incidents compared to states with weaker laws.[
However, because multiple factors such as mental health, socioeconomic challenges, drug abuse, and firearm safety contribute to the prevalence of gun violence, targeting each of these issues are necessary to decrease gun-related injuries in children in our community.
CONCLUSION
There was a notable effect of the COVID-19 pandemic on GSWH in our hospital cohort, with an increase in self-inflicted and drive-by shootings, a doubling of neurosurgical interventions, an increase in acuity of care for long-term disposition, and an increase in mortality. At a county level, there was an increase in overall deaths from GSWHs during the pandemic, the vast majority of which were nonaccidental. Our goal in this research is twofold: (1) to bring awareness to the reality that gun violence has claimed 72 children’s lives in our county over the past 9 years and (2) to encourage action to better support the mental and social health of our patients and communities with increased discourse about gun access and reform because seventy-two is seventy-two too many.
Ethical approval
The research/study was approved by the Institutional Review Board at Loma Linda University, number 5230304, dated July 13, 2023.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgments
We would like to thank our hospital’s Pediatric Trauma Service Support Team for their contributions to data acquisition.
References
1. Bernardino CoS. Crime statistics - 2023. City of San Bernardino. Available from: https://www.sbcity.org/city_hall/police_department/crime_statistics/about_ucr_statistics/crime_statistics/crime_statistics_-_2023 [Last accessed on 2024 Aug 15].
2. Bureau USC. Quick facts: San Bernardino County. Available from: https://www.census.gov/quickfacts/fact/table/sanbernardinocitycalifornia,US/RHI725223 [Last accessed on 2024 Aug 15].
3. Carter CW, Sharkey MS, Fishman F. Firearm-related musculoskeletal injuries in children and adolescents. J Am Acad Orthop Surg. 2017. 25: 169-78
4. Cohen JS, Donnelly K, Patel SJ, Badolato GM, Boyle MD, McCarter R. Firearms injuries involving young children in the United States during the COVID-19 pandemic. Pediatrics. 2021. 148: e2020042697
5. County SB. 2020 Community health status data report. San Bernardino County. Available from: https://www.sbcounty.gov/uploads/DPH/Documents/2021/04/SBCCVS__OCVS_Report20_v5.1.pdf [Last accessed on 2024 Aug 15].
6. DeCuypere M, Muhlbauer MS, Boop FA, Klimo P. Pediatric intracranial gunshot wounds: The Memphis experience. J Neurosurg Pediatr. 2016. 17: 595-601
7. Deng H, Yue JK, Winkler EA, Dhall SS, Manley GT, Tarapore PE. Pediatric firearm-related traumatic brain injury in United States trauma centers. J Neurosurg Pediatr. 2019. 24: 498-508
8. DiScala C, Sege R. Outcomes in children and young adults who are hospitalized for firearms-related injuries. Pediatrics. 2004. 113: 1306-12
9. Donnelly MR, Grigorian A, Swentek L, Arora J, Kuza CM, Inaba K. Firearm violence against children in the United States: Trends in the wake of the COVID-19 pandemic. J Trauma Acute Care Surg. 2022. 92: 65-8
10. Goel R, Zhu X, Makhani S, Petersen MR, Josephson CD, Katz LM. Blood transfusions in gunshot-wound-related emergency department visits and hospitalizations in the United States. Transfusion. 2021. 61: 2277-89
11. Hossain MM, Tasnim S, Sultana A, Faizah F, Mazumder H, Zou L. Epidemiology of mental health problems in COVID-19: A review. F1000Res. 2020. 9: 636
12. Hughes BD, Cummins CB, Shan Y, Mehta HB, Radhakrishnan RS, Bowen-Jallow KA. Pediatric firearm injuries: Racial disparities and predictors of healthcare outcomes. J Pediatr Surg. 2020. 55: 1596-603
13. Indicators SBCC. Crime rate. San Bernardino County Community Indicators. Available from: https://indicators.sbcounty.gov/safety/crime-rate [Last accessed on 2024 Aug 15].
14. Indicators SBCC. Substance abuse. San Bernardino County Community Indicators. Available from: https://indicators.sbcounty.gov/wellness/substance-abuse [Last accessed on 2024 Aug 15].
15. Luijten MA, van Muilekom MM, Teela L, Polderman TJ, Terwee CB, Zijlmans J. The impact of lockdown during the COVID-19 pandemic on mental and social health of children and adolescents. Qual Life Res. 2021. 30: 2795-804
16. Orantes C, Chan HK, Walter D, Chavez S, Ugalde IT. Pediatric firearm injury epidemiology at a level 1 trauma center from 2019 to 2021: Including time of the COVID-19 pandemic. Inj Epidemiol. 2023. 10: 41
17. Orlas CP, Thomas A, Herrera-Escobar JP, Price MA, Haider AH, Bulger EM. Long-term outcomes of firearm injury survivors in the United States: The national trauma research action plan scoping review. Ann Surg. 2021. 274: 962-70
18. Program FUCR. Federal Bureau of investigation crime data explorer. Available from: https://cde.ucr.cjis.gov/LATEST/webapp/#/pages/explorer/crime/crime-trend [Last accessed on 2024 Aug 15].
19. Pulcini CD, Goyal MK, Hall M, Gruhler De Souza H, Chaudhary S, Alpern ER. Nonfatal firearm injuries: Utilization and expenditures for children pre-and postinjury. Acad Emerg Med. 2021. 28: 840-7
20. Rodrigues M, Silva R, Franco M. COVID-19: Financial stress and well-being in families. J Fam Issues. 2023. 44: 1254-75
21. Sakran JV, Nance M, Riall T, Asmar S, Chehab M, Joseph B. Pediatric firearm injuries and fatalities: Do racial disparities exist?. Ann Surg. 2020. 272: 556-61
22. Schaechter J, Alvarez PG. Growing up-or not-with gun violence. Pediatr Clin North Am. 2016. 63: 813-26
23. Statistics NCfH. All injuries U.S Department of Health and Human Services. Available from: https://www.cdc.gov/nchs/fastats/injury.htm [Last accessed on 2024 Aug 15].
24. Vella MA, Warshauer A, Tortorello G, Fernandez-Moure J, Giacolone J, Chen B. Long-term functional, psychological, emotional, and social outcomes in survivors of firearm injuries. JAMA Surg. 2020. 155: 51-9
25. Wang G, Zhang Y, Zhao J, Zhang J, Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020. 395: 945-7
26. Wilson RF, Mintz S, Blair JM, Betz CJ, Collier A, Fowler KA. Unintentional firearm injury deaths among children and adolescents aged 0-17 years-National Violent Death Reporting system, United States, 2003-2021. MMWR Morb Mortal Wkly Rep. 2023. 72: 1338-45
27. Woodruff G, Palmer L, Fontane E, Kalynych C, Hendry P, Thomas AC. Nine years of pediatric gunshot wounds: A descriptive analysis. Prev Med Rep. 2022. 28: 101890
28. Zaami S, Marinelli E, Varì MR. New trends of substance abuse during COVID-19 pandemic: An international perspective. Front Psychiatry. 2020. 11: 700