- Department of Neurosurgery, Japanese Redcross Shizuoka Hospital, Shizuoka, Japan
- Department of Neurosurgery, Hamamatsu University School of Medicine, Hamamatsu, Japan
Correspondence Address:
Hiroaki Neki, Department of Neurosurgery, Hamamatsu University School of Medicine, Hamamatsu, Japan.
DOI:10.25259/SNI_827_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yuki Shiraishi1, Hiroaki Neki2, Gakuji Maruyama1, Yuko Nonaka1, Tsutomu Tokuyama1, Hiroshi Tenjin1, Osamu Saito1, Kazuhiko Kurozumi2. Effectiveness of super-selective digital subtraction angiography and 3D rotational digital subtraction venography for a developmental venous anomaly with an arteriovenous malformation: A case report and literature review. 15-Nov-2024;15:422
How to cite this URL: Yuki Shiraishi1, Hiroaki Neki2, Gakuji Maruyama1, Yuko Nonaka1, Tsutomu Tokuyama1, Hiroshi Tenjin1, Osamu Saito1, Kazuhiko Kurozumi2. Effectiveness of super-selective digital subtraction angiography and 3D rotational digital subtraction venography for a developmental venous anomaly with an arteriovenous malformation: A case report and literature review. 15-Nov-2024;15:422. Available from: https://surgicalneurologyint.com/surgicalint-articles/13222/
Abstract
Background: Arteriovenous malformation (AVM) and developmental venous anomaly (DVA) rarely coexist. Developing a surgical strategy to treat this co-occurrence is difficult due to the unclear pathogenesis. We report the use of super-selective digital subtraction angiography (DSA) and Three-dimensional (3D) rotational digital subtraction venography (DSV) to develop a surgical strategy for complex AVM draining into a DVA.
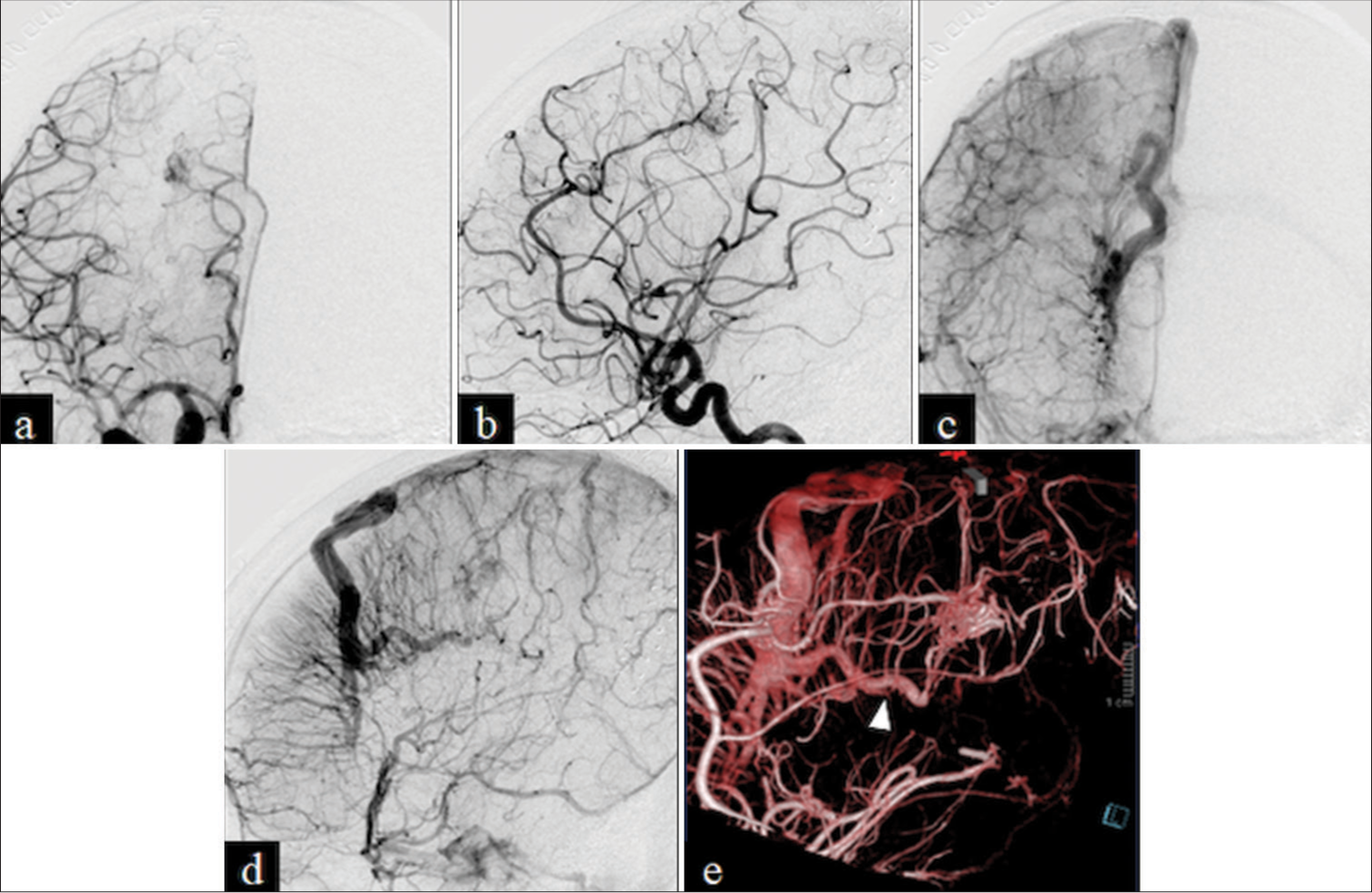
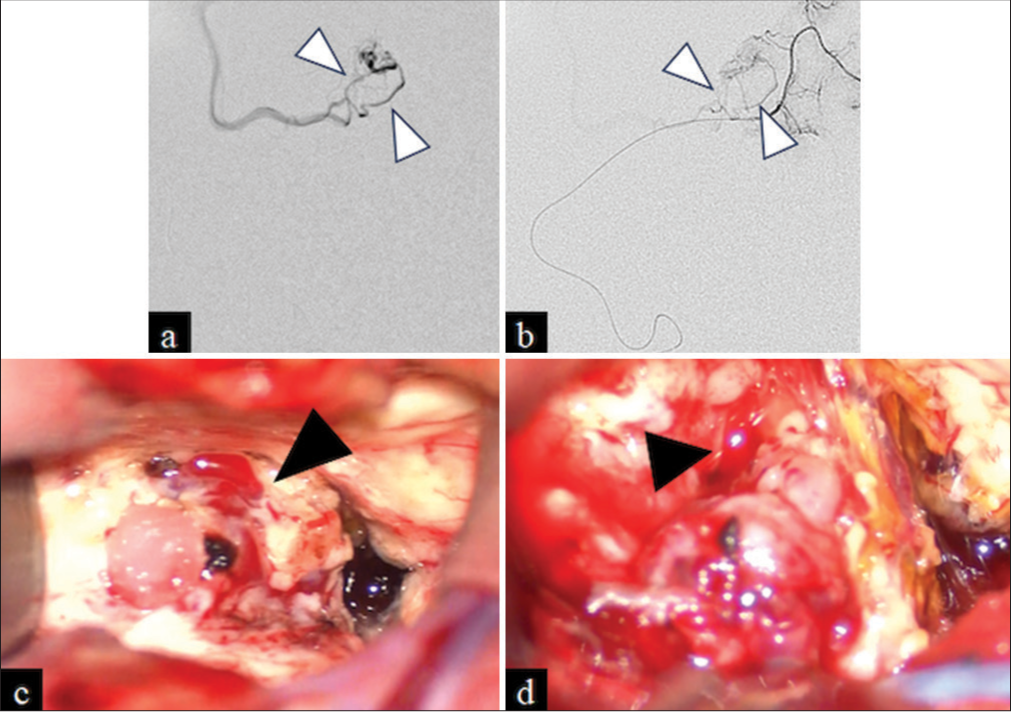
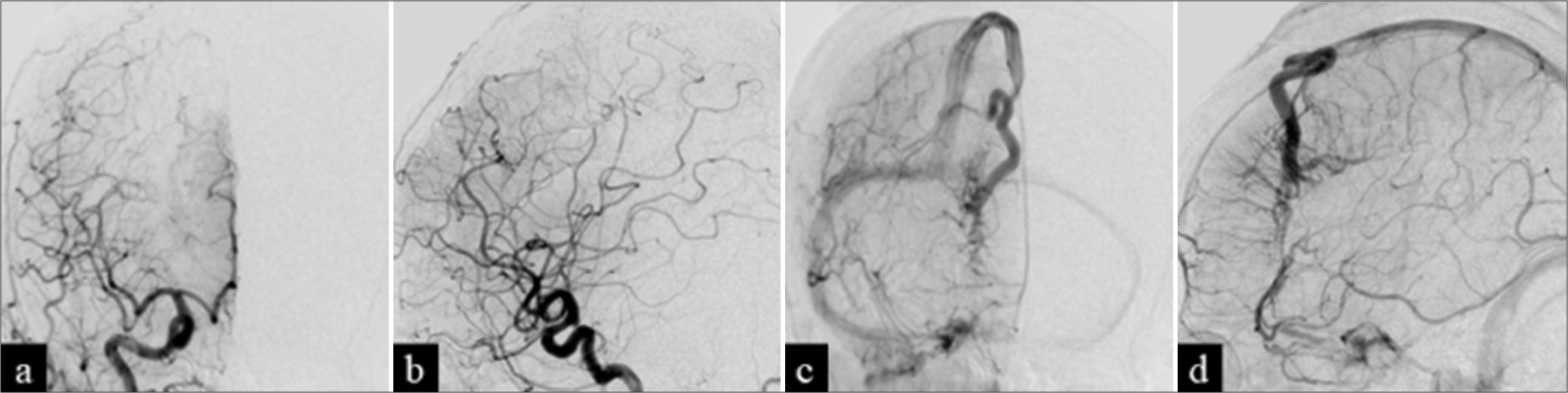
Case Description: A 58-year-old woman presented with left hemiparesis and unconsciousness. Plain and contrast computed tomography showed a right frontal subcortical hematoma and a heterogeneous contrast lesion anterior to the hematoma, leading to a dilated vessel. The hematoma was removed due to worsening unconsciousness. DSA revealed a right frontal AVM of Spetzler-Martin grade 2 with superficial drainage into a DVA, and 3D-DSV revealed that the intermediate part of the DVA involved normal parenchyma. Interventional transarterial embolization and surgical nidus removal were planned. Preoperative super-selective DSA showed two medullary veins draining from the AVM into the DVA. Thus, we decided to separate the two medullary veins from the nidus. Postoperative angiography revealed complete removal of the AVM and preservation of the DVA.
Conclusion: Treating a complex AVM draining into a DVA is challenging; surgeons have to remove only the AVM portion and preserve the DVA. Super-selective DSA and 3D rotational DSV were performed to develop the surgical strategy.
Keywords: Three-dimensional-rotational digital subtraction venography, Arteriovenous malformation, Developmental venous anomaly, Digital subtraction angiography, Super-selective digital subtraction angiography
INTRODUCTION
Developmental venous anomaly (DVA) is a variation of normal medullary veins and the most common brain vascular malformation, with an incidence of approximately 2.6%.[
A DVA coexisting with an AVM is rare, with only about 30 reported cases, and the pathogenesis of this co-occurrence is unclear, making the development of a treatment strategy difficult. Several treatments were developed in previous reports, including surgical resection, transarterial embolization, stereotactic radiosurgery, and a combination of these techniques.[
CASE PRESENTATION
A 58-year-old woman with no notable past medical or family history visited our hospital due to left hemiparesis and unconsciousness. Plain and contrast computed tomography (CT) revealed a right frontal subcortical hematoma and a heterogeneous contrast lesion anterior to the hematoma, leading to a dilated vessel [
The patient was diagnosed with subcortical hemorrhage due to a ruptured AVM, and surgical treatment for the AVM was planned. Transarterial embolization of the two arteries was performed to reduce the flow of the AVM 36 days after the hemorrhage. Super-selective DSA revealed the AVM draining into an intermediate part of the DVA through two medullary veins [
DISCUSSION
DVAs are considered benign cerebrovascular variants. However, when coexisting with other cerebrovascular malformations, DVAs may cause symptomatic hemorrhaging.[
To address the higher bleeding risk, Pereira et al. suggested preventive treatment even for asymptomatic patients with a true AVM draining into a DVA.[
DSA and 3D rotational DSA are standard imaging tools for evaluating complex vascular lesions. These tools are useful for neurosurgery, endovascular treatment, and radiosurgery.[
In our case, 3D-DSV and super-selective DSA showed the angioarchitectures of the coexisting AVM and DVA; 3D-DSV revealed that the intermediate DVA collected the medullary veins and should be preserved. In addition, super-selective DSA revealed that the AVM drained into the intermediate part of DVA through two medullary veins. Thus, we preoperatively decided to detach the two medullary veins and preserve the intermediate part of the DVA.
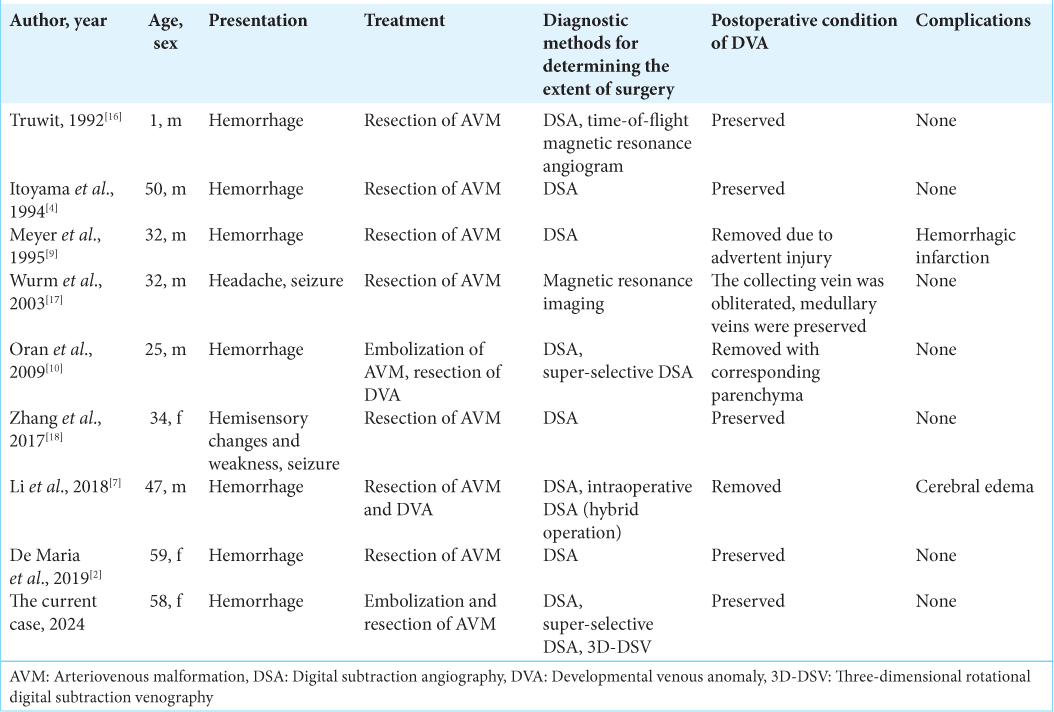
We performed a literature search using PubMed to identify other surgical cases of AVMs draining into DVAs and identified 9 surgical cases [
CONCLUSION
A hemorrhagic case of a true AVM directly draining into a DVA is described. Preventive treatment for this complex lesion was recommended due to the hemorrhagic presentation; however, surgeries for these deformities are challenging with high complication rates. Therefore, 3D-DSV and super-selective DSA were employed to obtain detailed angioarchitectures, which were useful for developing a safe surgical approach.
Ethical approval
The research/study was approved by the Institutional Review Board at Japanese Redcross Shizuoka Hospital, number 2024-15, dated September 19, 2024.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Aoki R, Srivatanakul K. Developmental venous anomaly: Benign or not benign. Neurol Med Chir (Tokyo). 2016. 56: 534-43
2. De Maria L, Lanzino G, Flemming KD, Brinjikji W. Transitional venous anomalies and DVAs draining brain AVMs: A single-institution case series and review of the literature. J Clin Neurosci. 2019. 66: 165-77
3. Holmes OE, Szanto J, Abitbul VT, Al Mansoori T, Al-Qahtani H, Sinclair J. Selective and super-selective C-arm based cone beam CT angiography (CBCTA) with DynaCT for CyberKnife radiosurgery planning of intracranial Arteriovenous Malformations (AVMs). J Radiosurg SBRT. 2018. 5: 305-13
4. Itoyama Y, Kitano I, Fujioka S, Takagi S, Morioka M, Yano T. Mixed angioma of the brain: Report of two cases. No Shinkei Geka. 1994. 22: 465-9
5. Kurita H, Sasaki T, Tago M, Kaneko Y, Kirino T. Successful radiosurgical treatment of arteriovenous malformation accompanied by venous malformation. AJNR Am J Neuroradiol. 1999. 20: 482-5
6. Lasjaunias P, Burrows P, Planet C. Developmental Venous Anomalies (DVA): The so-called venous angioma. Neurosurg Rev. 1986. 9: 233-42
7. Li K, Guo Y, Qu L, Xu B, Xu K, Yu J. Hybrid surgery for an arteriovenous malformation fed by an accessory middle cerebral artery and drained by a developmental venous anomaly: A case report and literature review. Exp Ther Med. 2018. 16: 1994-2000
8. Ma L, Hoz SS, Grossberg JA, Lang MJ, Gross BA. Developmental venous anomalies. Neurosurg Clin N Am. 2024. 35: 355-61
9. Meyer B, Stangl AP, Schramm J. Association of venous and true arteriovenous malformation: A rare entity among mixed vascular malformations of the brain. Case report. J Neurosurg. 1995. 83: 141-4
10. Oran I, Kiroglu Y, Yurt A, Ozer FD, Acar F, Dalbasti T. Developmental Venous Anomaly (DVA) with arterial component: A rare cause of intracranial haemorrhage. Neuroradiology. 2009. 51: 25-32
11. Pereira VM, Geibprasert S, Krings T, Aurboonyawat T, Ozanne A, Toulgoat F. Pathomechanisms of symptomatic developmental venous anomalies. Stroke. 2008. 39: 3201-15
12. Picart T, Dumot C, Guyotat J, Eker O, Berhouma M, Pelissou-Guyotat I. Arteriovenous malformation drained into a developmental venous anomaly: A case report and up-dated literature review. Neurochirurgie. 2020. 66: 471-6
13. Rammos SK, Maina R, Lanzino G. Developmental venous anomalies: Current concepts and implications for management. Neurosurgery. 2009. 65: 20-9 discussion 29-30
14. Raz E, Shapiro M, Mir O, Nossek E, Nelson PK. Arterial and venous 3D fusion AV-3D-DSA: A novel approach to cerebrovascular neuroimaging. AJNR Am J Neuroradiol. 2021. 42: 1282-4
15. Sarwar M, McCormick WF. Intracerebral venous angioma. Case report and review. Arch Neurol. 1978. 35: 323-5
16. Truwit CL. Venous angioma of the brain: History, significance, and imaging findings. AJR Am J Roentgenol. 1992. 159: 1299-307
17. Wurm G, Schnizer M, Nussbaumer K, Wies W, Holl K. Recurrent cryptic vascular malformation associated with a developmental venous anomaly. Br J Neurosurg. 2003. 17: 188-95
18. Zhang M, Connolly ID, Teo MK, Yang G, Dodd R, Marks M. Management of arteriovenous malformations associated with developmental venous anomalies: A literature review and report of 2 cases. World Neurosurg. 2017. 106: 563-9