- Department of Neurosurgery, Tazuke Kofukai Medical Research Institute Kitano Hospital, Osaka,
- Department of Neurosurgery, Japanese Red Cross Fukui Hospital, Fukui,
- Department of Health Science, Graduate School of Health Science, Morinomiya University of Medical Sciences, Osaka, Japan.
Correspondence Address:
Hiroki Toda, Department of Neurosurgery, Tazuke Kofukai Medical Research Institute and Kitano Hospital, Osaka, Japan.
DOI:10.25259/SNI_997_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Wataru Yoshizaki1, Yoshiki Fujikawa1, Sadaharu Torikoshi2, Toshiro Katayama3, Koichi Iwasaki1, Hiroki Toda1. Effects of microvascular decompression on quality-of-life in trigeminal neuralgia patients aged 70 years and older. 03-Feb-2023;14:41
How to cite this URL: Wataru Yoshizaki1, Yoshiki Fujikawa1, Sadaharu Torikoshi2, Toshiro Katayama3, Koichi Iwasaki1, Hiroki Toda1. Effects of microvascular decompression on quality-of-life in trigeminal neuralgia patients aged 70 years and older. 03-Feb-2023;14:41. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12138
Abstract
Background: Trigeminal neuralgia (TN) occasionally affects older adults, frequently worsens, and becomes refractory to medication. Older adult patients with TN may consider microvascular decompression (MVD) for their treatment. No study examines MVD effects on older adult TN patients’ health-related quality of life (HRQoL). The present study evaluates the HRQoL of TN patients aged 70 years and older before and after MVD.
Methods: Adult TN patients who underwent MVD evaluated their HRQoL using the 36-Item Short-form (SF-36) Health Survey before and 6 months after MVD. The patients were divided into four groups according to their decade of age. The clinical parameters and operative outcomes were analyzed statistically. The SF-36 physical, mental, and role social component summary scores and eight domain scale scores were analyzed using a twoway repeated-measures analysis of variance (ANOVA) to compare the effects of age group and preoperative and postoperative time points.
Results: Among 57 adult patients (34 women, 23 men; mean age, 69 years; range, 30–89 years), 21 patients were in their seventies, and 11 were in their eighties. The SF-36 scores of patients in all age groups improved after MVD. Two-way repeated-measures ANOVA demonstrated a significant age group effect on the physical component summary and its physical functioning domain. A time point effect was significant on all component summaries and domains. There was a significant interaction between age group and time point effects on the bodily pain domain. These results suggested that patients 70 years and older had significant postoperative HRQoL improvement, but their improvement of physical-related HRQoL and multiple physical pain issues were limited.
Conclusion: Impaired HRQoL in TN patients aged 70 years and older can improve after MVD. Careful management of multiple comorbidities and surgical risks enables MVD to be an appropriate treatment for older adult patients with refractory TN.
Keywords: 36-Item short-form health survey (SF-36), Health-related quality of life, Microvascular decompression, Older adult, Trigeminal neuralgia
INTRODUCTION
Trigeminal neuralgia (TN), characterized by severe, unilateral, and brief electric shock-like facial pains, occasionally affects older adults.[
Health-related quality of life (HRQoL) following treatment is another concern in evaluating the treatment modality, especially for older adult patients.[
MATERIALS AND METHODS
Patient populations and demographics
We prospectively studied 57 consecutive patients with TN who underwent MVD surgery between January 2018 and December 2020. Written informed consent was obtained from all patients. The institutional review board approved this cohort study. The authors prepared the manuscript following the Strengthening the Reporting of Observational Studies in Epidemiology guideline.[
Inclusion criteria were a diagnosis of classical TN according to the International Classification of Headache Disorders 3rd edition,[
The clinical parameters were as follows: age at operation, affected side, neuralgia type, preoperative comorbidity, operative findings of offending vessels, preoperative, and postoperative Barrow Neurological Institute (BNI) pain intensity score I, no trigeminal pain, no medication; II, occasional pain, not requiring medication; III, some pain, adequately controlled with medication; IV, some pain, not adequately controlled with medication; V, severe pain/no pain relief)[
HRQoL SF-36 evaluation
We interviewed the TN patients about their HRQoL before and 6 months after MVD using SF-36 version 2 (Medical Outcomes Trust, Hanover, NH).[
Statistical analysis
Descriptive statistics for patient demographics and outcomes showed the numbers and percentages (%) for categorical variables, the mean with ranges or 95% confidence intervals (95% CI) for continuous variables, and the median with ranges for ordinal variables and dosage of carbamazepine.
The effect of age groups and time points on the categorical and ordinal patient demographic data was analyzed using Fisher’s exact test and generalized linear models, respectively. A two-way repeated-measures analysis of variance (ANOVA) examined the effect of age group (30–59 years, 60–69 years, 70–79 years, 80–89 years; between-subjects) and time point (preoperative vs. postoperative 6 months, within-subjects) on the SF-36 three component summary scores and eight domain scale scores after eliminating outliers and checking normality. We examined a post hoc pairwise comparison between age groups at each time point and a comparison between time points in each age group. Bonferroni adjustments were applied for ANOVA analysis to avoid type I error. Bonferroni adjustments were set significance at α < 0.017 (αadj = 0.05/3, [0.0033 for P < 0.01]) for the examination of three component summary scores and at α < 0.0063 (αadj = 0.05/8 [00142 for P < 0.01]) for the eight domain scales.
The correlation between the SF-36 component summary scores taken before and after MVD and BNI scores was measured using the Pearson correlation. All analyses were conducted using R version 4.0.2.[
The efforts to minimize biases in this study included a prospective study design for the chronology and selection bias and a standardized interview using the SF-36 for the interviewer bias.[
RESULTS
Patient characteristics, operative findings, and postoperative outcomes
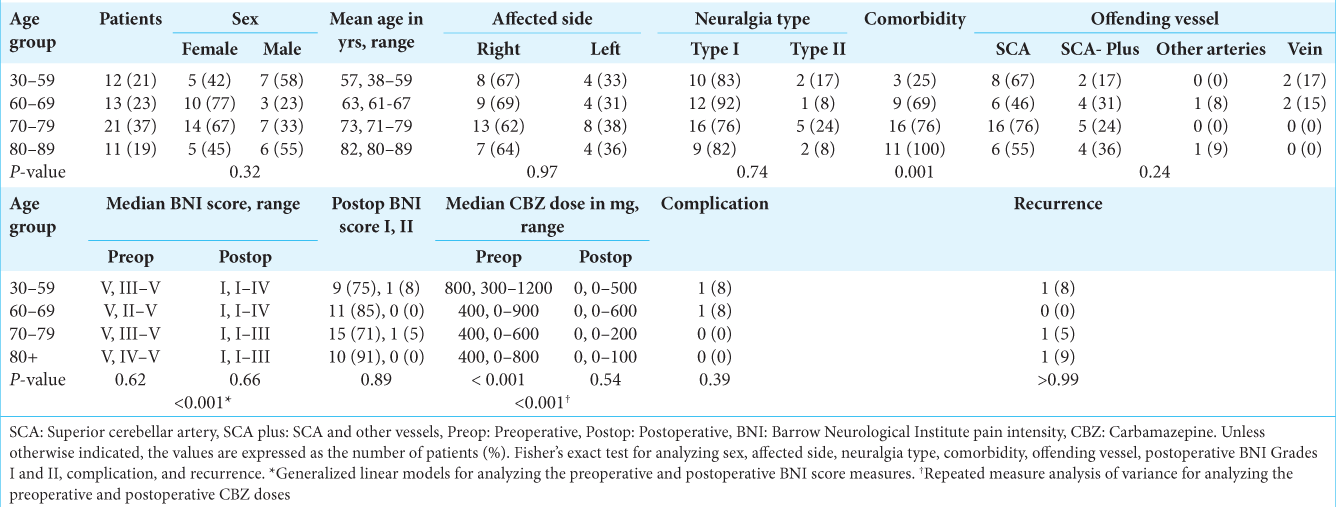
Fifty-seven adult patients (34 women, 23 men; mean age, 69 years; range, 30–89 years) were eligible for statistical analysis [
Nine of 11 patients aged 80 years and older had complete pain relief (BNI score I) with no significant complications [
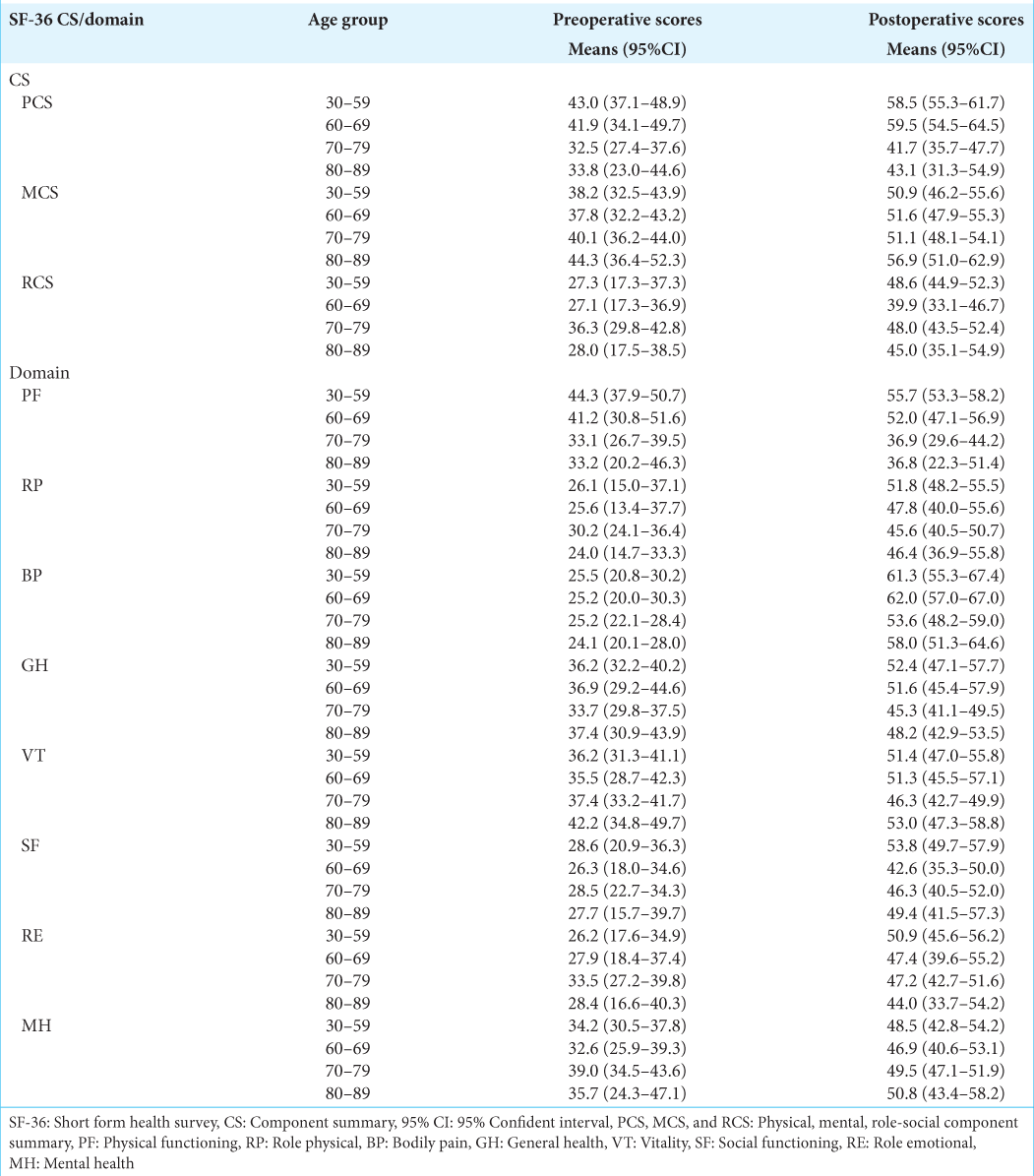
Preoperative and postoperative SF-36 scores
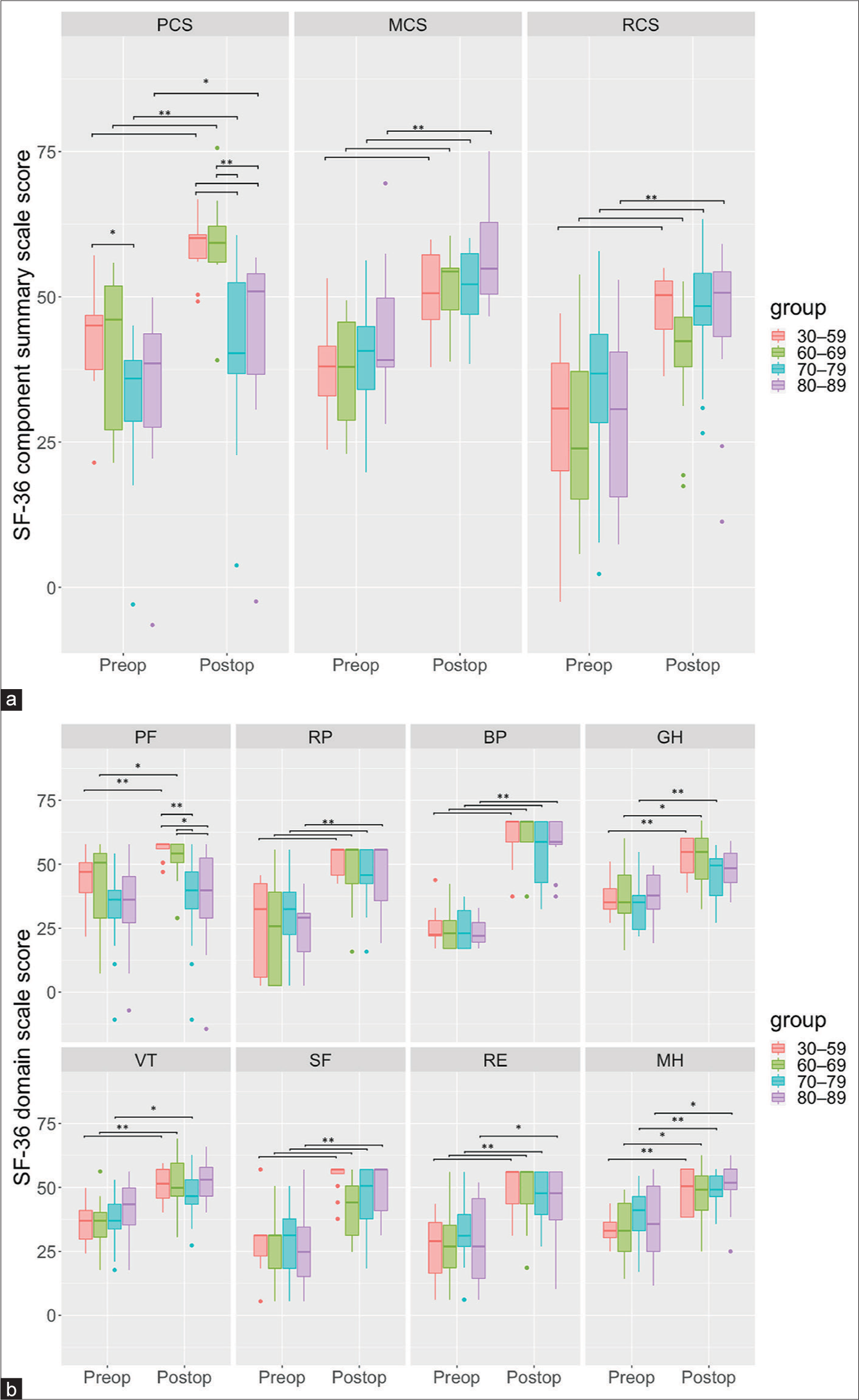
In all age groups, the SF-36 PCS, MCS, and RCS scores were low before MVD and considerably improved after MVD [
Figure 1:
Box plots showing the 36-Item Short-form (SF-36) Health Survey component summary score (a) and domain scale scores (b) of the patients of 59 years or younger (red), those of 60–69 years (green), those of 70–79 years (blue), and those of 80 years and older (purple) in the preoperative and postoperative time points. The Bonferroni-adjusted p-value is set at 0.017 (*) and 0.0034 (**) for the three component summary scores (a) and at 0.00625 (*) and 0.00125 (**) for the eight domain scale scores (b). PCS, MCS, and RCS: Physical, mental, and role-social component summary, PF: Physical functioning, RP: Role physical, BP: Bodily pain, GH: General health, VT: Vitality, SF: Social functioning, RE: Role emotional, MH: Mental health, Preop: preoperative, Postop: postoperative.
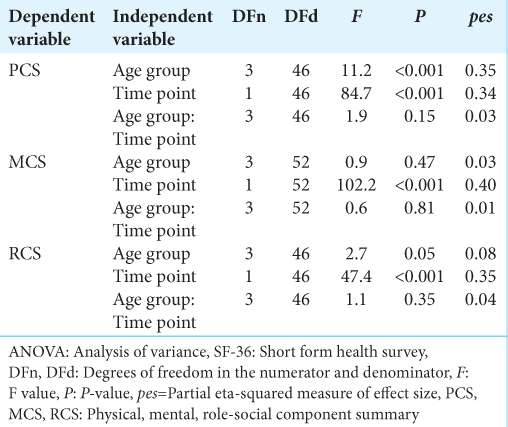
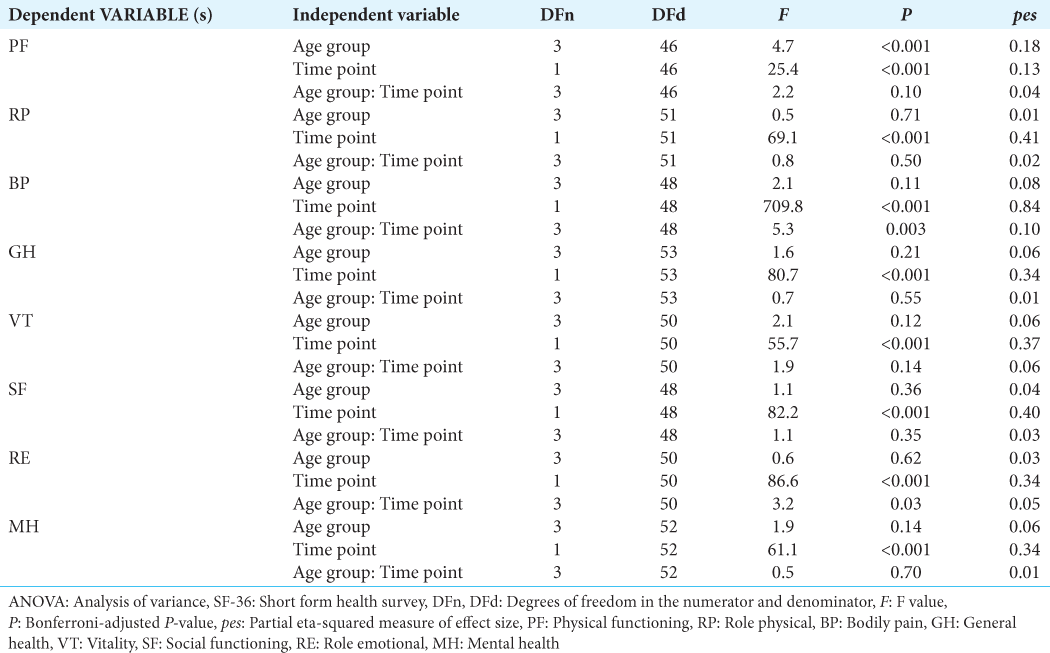
Two-way repeated-measures ANOVA and post hoc analysis examined the SF-36 results as follows. Two-way repeated-measure ANOVA demonstrated no significant interaction between age group and time point effects on any component summary scores [
Among the eight domain scales, physical functioning was the domain with a significant age group effect (F (3, 46) = 4.7, P < 0.001, pes = 0.18) and a significant time point effect (F (1, 46) = 25.4, P< 0.001, pes = 0.13), but with no significant interaction between age group and time point effects [
Bodily pain was the only domain with a significant interaction between age group and time point effects (F (3, 48) = 5.3, P = 0.003, pes = 0.10). A simple main effect of the time point on the bodily pain domain scale score was significant (F (1, 48) = 709.8, P < 0.001, pes = 0.6284); however, the effect on the age group was not significant [
As briefly described above, general health and vitality domains were the domains in which postoperative improvements were significant in all age groups except for the patients 80 years and older [
Correlation between BNI and component summary score
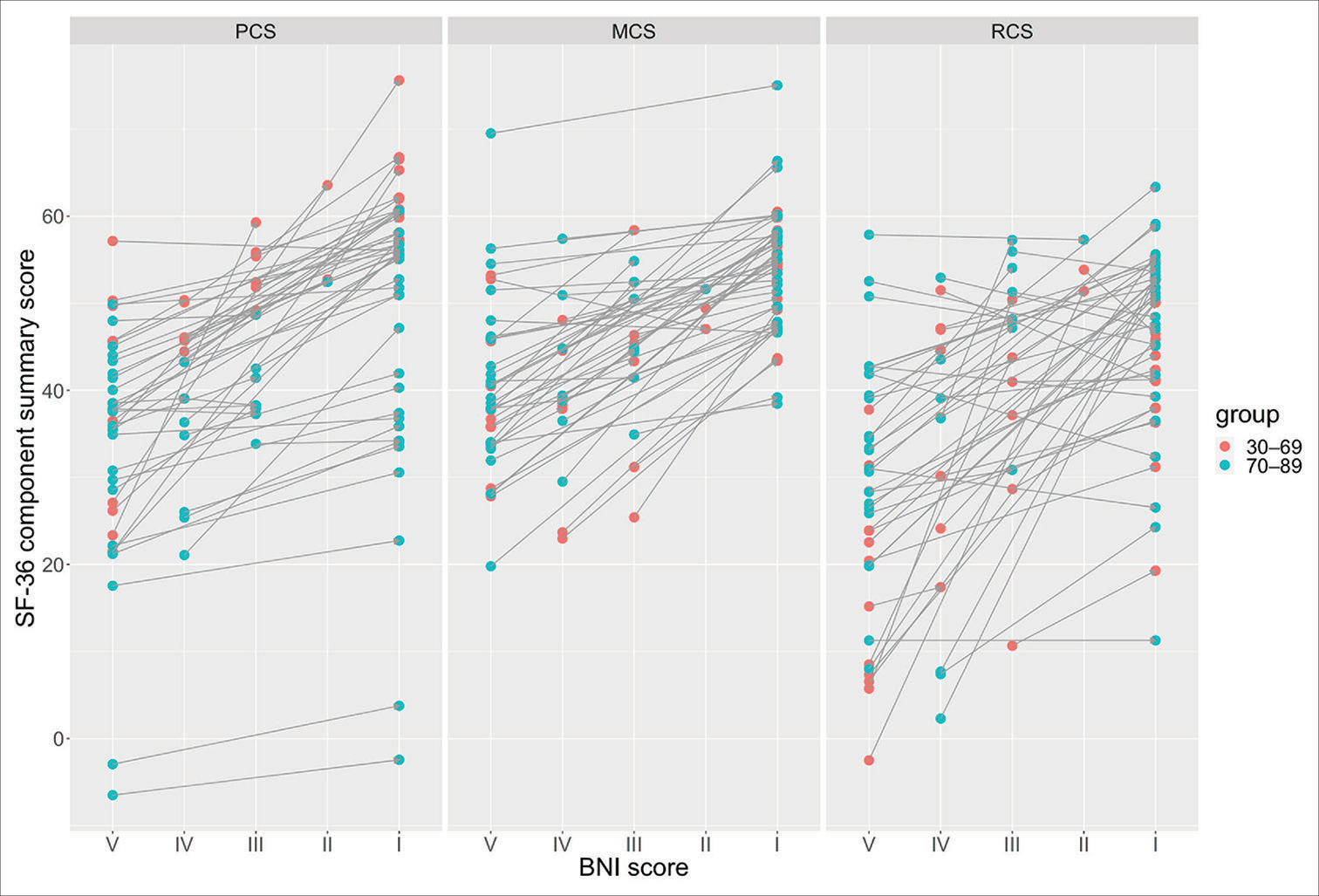
The mean SF-36 component summary and domain scale scores increased above 40 postoperatively, except for the physical functioning domain scale scores in patients 70 years and older [
Figure 2:
Paired scatter plots showing the Barrow Neurological Institute pain intensity score (BNI score) and SF-36 component summary score of the patients of 30–69 years (red) and those of 70–89 years (blue). The paired preoperative and postoperative time points are lined with arrows from the preoperative to the postoperative time point. The right upward arrow indicates improvement of both the BNI and component summary scores. In contrast, the right downward arrow suggests improvement of the BNI score and deterioration of the component summary score. PCS, MCS, and RCS: Physical, mental, and role-social component summary.
DISCUSSION
The present study showed that young and older adult TN patients suffer impaired physical, mental, and social functioning of HRQoL, and these HRQoL scores improved after MVD in any age group. Only few studies have investigated the HRQoL of MVD-treated TN patients at various postoperative time points.[
The present study illustrated that aging per se does not interfere with the HRQoL improvement following MVD, although postoperative improvement of physical-related HRQoL is limited in older patients. A time point effect was significant on all SF-36 component summary and domain scores, suggesting that these HRQoL scores improve following MVD in both older and non-older groups. There was a significant interaction between age group and time point effects on the bodily pain domain. This significant interaction can be interpreted as a result of multiple bodily pain issues besides TN in older adults, as their TN improved significantly after MVD.
The results suggest that older adult patients can see their HRQoL improvement following MVD. Pain relief and medication reduction contribute to HRQoL improvement. The HRQoL of older adult patients does not deteriorate postoperatively as long as severe complications do not occur. The quantitative HRQoL data are compatible with our intuitive and empirical assessment of surgical outcomes in older adult patients.
In practice, older TN patients may consider ablation treatment using a gamma knife[
This study has several limitations. The present preliminary examination is a prospective but not randomized, single-center, small-scale, and single-modality study. Further research should compare the HRQoL effects of MVD with a gamma knife and other surgical modalities for older adult patients. In addition, a forthcoming study should estimate patients’ frailty for their preoperative conditions and the surgical impacts on their frailty. Furthermore, the patients in the present study had no severe postoperative complications; therefore, the effects of surgical complications on HRQoL[
CONCLUSION
Impaired HRQoL in TN patients aged 70 years and older can improve after MVD. Careful management of multiple comorbidities and surgical risks enables MVD to be an appropriate treatment for older adult patients with refractory TN.
Authors’ contributions
Wataru Yoshizaki: Investigation, Writing-Original Draft; Yoshiki Fujikawa: Investigation, Writing-Original Draft; Sadaharu Torikoshi: Investigation; Toshiro Katayama: Software, Formal analysis, Data Curation; Koichi Iwasaki: Validation, Supervision; Hiroki Toda: Conceptualization, Methodology, Software, Writing-Original Draft, Writing-Review and Editing, Visualization, Supervision.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Akram H, Mirza B, Kitchen N, Zakrzewska JM. Proposal for evaluating the quality of reports of surgical interventions in the treatment of trigeminal neuralgia: The Surgical Trigeminal Neuralgia Score. Neurosurg Focus. 2013. 35: E3
2. Cruccu G, Gronseth G, Alksne J, Argoff C, Brainin M, Burchiel K. AAN-EFNS guidelines on trigeminal neuralgia management. Eur J Neurol. 2008. 15: 1013-28
3. Ferguson GG, Brett DC, Peerless SJ, Barr HW, Girvin JP. Trigeminal neuralgia: A comparison of the results of percutaneous rhizotomy and microvascular decompression. Can J Neurol Sci. 1981. 8: 207-14
4. Fukuhara S, Bito S, Green J, Hsiao A, Kurokawa K. Translation, adaptation, and validation of the SF-36 Health Survey for use in Japan. J Clin Epidemiol. 1998. 51: 1037-44
5. Gronseth G, Cruccu G, Alksne J, Argoff C, Brainin M, Burchiel K. Practice parameter: The diagnostic evaluation and treatment of trigeminal neuralgia (an evidence-based review): Report of the Quality Standards Subcommittee of the American Academy of Neurology and the European Federation of Neurological Societies. Neurology. 2008. 71: 1183-90
6. Günther T, Gerganov VM, Stieglitz L, Ludemann W, Samii A, Samii M. Microvascular decompression for trigeminal neuralgia in the elderly: Long-term treatment outcome and comparison with younger patients. Neurosurgery. 2009. 65: 477-82 discussion 82
7. Hall GC, Carroll D, McQuay HJ. Primary care incidence and treatment of four neuropathic pain conditions: A descriptive study, 2002-2005. BMC Fam Pract. 2008. 9: 26
8. Holste K, Chan AY, Rolston JD, Englot DJ. Pain outcomes following microvascular decompression for drug-resistant trigeminal neuralgia: A systematic review and meta-analysis. Neurosurgery. 2020. 86: 182-90
9. International Headache Socie. Headache classification committee of the international headache society (IHS) the international classification of headache disorders, 3rd ed. Cephalalgia. 2018. 38: 1-211
10. Jafree DJ, Williams AC, Zakrzewska JM. Impact of pain and postoperative complications on patient-reported outcome measures 5 years after microvascular decompression or partial sensory rhizotomy for trigeminal neuralgia. Acta Neurochir (Wien). 2018. 160: 125-34
11. Katusic S, Beard CM, Bergstralh E, Kurland LT. Incidence and clinical features of trigeminal neuralgia, Rochester, Minnesota, 1945-1984. Ann Neurol. 1990. 27: 89-95
12. Katusic S, Williams DB, Beard CM, Bergstralh EJ, Kurland LT. Epidemiology and clinical features of idiopathic trigeminal neuralgia and glossopharyngeal neuralgia: Similarities and differences, Rochester, Minnesota, 1945-1984. Neuroepidemiology. 1991. 10: 276-81
13. Li L, Seaman SC, Bathla G, Smith MC, Dundar B, Noeller J. Microvascular decompression versus stereotactic radiosurgery for trigeminal neuralgia: A single-institution experience. World Neurosurg. 2020. 143: e400-8
14. Linskey ME, Ratanatharathorn V, Peñagaricano J. A prospective cohort study of microvascular decompression and gamma knife surgery in patients with trigeminal neuralgia. J Neurosurg. 2008. 109: 160-72
15. McLaughlin MR, Jannetta PJ, Clyde BL, Subach BR, Comey CH, Resnick DK. Microvascular decompression of cranial nerves: Lessons learned after 4400 operations. J Neurosurg. 1999. 90: 1-8
16. Noorani I, Lodge A, Durnford A, Vajramani G, Sparrow O. Comparison of first-time microvascular decompression with percutaneous surgery for trigeminal neuralgia: Long-term outcomes and prognostic factors. Acta Neurochir (Wien). 2021. 163: 1623-34
17. Nova CV, Zakrzewska JM, Baker SR, Riordain RN. Treatment outcomes in trigeminal neuralgia-a systematic review of domains, dimensions and measures. World Neurosurg X. 2020. 6: 100070
18. Obermueller K, Shiban E, Obermueller T, Meyer B, Lehmberg J. Working ability and use of healthcare resources for patients with trigeminal neuralgia treated via microvascular decompression. Acta Neurochir (Wien). 2018. 160: 2521-7
19. Oh IH, Choi SK, Park BJ, Kim TS, Rhee BA, Lim YJ. The treatment outcome of elderly patients with idiopathic trigeminal neuralgia: Micro-vascular decompression versus gamma knife radiosurgery. J Korean Neurosurg Soc. 2008. 44: 199-204
20. Pannucci CJ, Wilkins EG. Identifying and avoiding bias in research. Plast Reconstr Surg. 2010. 126: 619-25
21. Phan K, Rao PJ, Dexter M. Microvascular decompression for elderly patients with trigeminal neuralgia. J Clin Neurosci. 2016. 29: 7-14
22. R Foundation for Statistical Computing. Vienna, Austria: R: A Language and Environment for Statistical Computing, Vienna, Austria. Available from: https://www.r-project.org [Last accessed on 2023 Jan 19].
23. Raygor KP, Lee AT, Nichols N, Wang DD, Ward MM, Barbaro NM. Long-term pain outcomes in elderly patients with trigeminal neuralgia: Comparison of first-time microvascular decompression and stereotactic radiosurgery. Neurosurg Focus. 2020. 49: E23
24. Rogers CL, Shetter AG, Fiedler JA, Smith KA, Han PP, Speiser BL. Gamma knife radiosurgery for trigeminal neuralgia: The initial experience of the Barrow Neurological Institute. Int J Radiat Oncol Biol Phys. 2000. 47: 1013-9
25. Rughani AI, Dumont TM, Lin CT, Tranmer BI, Horgan MA. Safety of microvascular decompression for trigeminal neuralgia in the elderly. Clinical article. J Neurosurg. 2011. 115: 202-9
26. Sekula RF, Frederickson AM, Jannetta PJ, Quigley MR, Aziz KM, Arnone GD. Microvascular decompression for elderly patients with trigeminal neuralgia: A prospective study and systematic review with meta-analysis. J Neurosurg. 2011. 114: 172-9
27. Shibahashi K, Morita A, Kimura T. Surgical results of microvascular decompression procedures and patient’s postoperative quality of life: Review of 139 cases. Neurol Med Chir. 2013. 53: 360-4
28. Toda H, Goto M, Iwasaki K. Patterns and variations in microvascular decompression for trigeminal neuralgia. Neurol Med Chir (Tokyo). 2015. 55: 432-41
29. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the Reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ. 2007. 335: 806-8
30. Wallach J, Ho AL, Kim LH, Chaudhuri AA, Chaudhary N, Vaz-Guimaraes F. Quantitative analysis of the safety and efficacy of microvascular decompression for patients with trigeminal neuralgia above and below 65 years of age. J Clin Neurosci. 2018. 55: 13-6
31. Wang DD, Raygor KP, Cage TA, Ward MM, Westcott S, Barbaro NM. Prospective comparison of long-term pain relief rates after frst-time microvascular decompression and stereotactic radiosurgery for trigeminal neuralgia. J Neurosurg. 2018. 128: 68-77
32. Ware JE, Kosinski M, Gandek B, Aaronson NK, Apolone G, Bech P. The factor structure of the SF-36 Health Survey in 10 countries: Results from the IQOLA project. International quality of life assessment. J Clin Epidemiol. 1998. 51: 1159-65
33. Yang DB, Wang ZM, Jiang DY, Chen HC. The efficacy and safety of microvascular decompression for idiopathic trigeminal neuralgia in patients older than 65 years. J Craniofac Surg. 2014. 25: 1393-6
34. Yu R, Wang C, Qu C, Jiang J, Meng Q, Wang J. Study on the therapeutic effects of trigeminal neuralgia with microvascular decompression and stereotactic gamma knife surgery in the elderly. J Craniofac Surg. 2019. 30: e77-80
35. Zakrzewska JM, Linskey ME. Trigeminal neuralgia. BMJ Clin Evid. 2009. 2009: 1207
36. Zakrzewska JM, Lopez BC, Kim SE, Coakham HB. Patient reports of satisfaction after microvascular decompression and partial sensory rhizotomy for trigeminal neuralgia. Neurosurgery. 2005. 56: 1304-11 discussion 11-2
37. Zakrzewska JM, Patsalos PN. Long-term cohort study comparing medical (oxcarbazepine) and surgical management of intractable trigeminal neuralgia. Pain. 2002. 95: 259-66
38. Zeng YJ, Zhang H, Yu S, Zhang W, Sun XC. Efficacy and safety of microvascular decompression and gamma knife surgery treatments for patients with primary trigeminal neuralgia: A prospective study. World Neurosurg. 2018. 116: e113-7
39. Zhao H, Tang Y, Zhang X, Li S. Microvascular decompression for idiopathic primary trigeminal neuralgia in patients over 75 Years of age. J Craniofac Surg. 2016. 27: 1295-7