- Department of Neurosurgery and Spine Surgery, Ha Noi Medical University, Ha Nội, Vietnam.
Correspondence Address:
Lê Hoàng Nhã, Department of Neurosurgery and Spine Surgery, Ha Noi Medical University, Ha Nội, Vietnam.
DOI:10.25259/SNI_751_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Lê Hoàng Nhã, Kiều Đình Hùng. Efficacy of cement-augmented pedicle screw fixation for osteoporotic mid-thoracic vertebral fractures. 20-Oct-2023;14:378
How to cite this URL: Lê Hoàng Nhã, Kiều Đình Hùng. Efficacy of cement-augmented pedicle screw fixation for osteoporotic mid-thoracic vertebral fractures. 20-Oct-2023;14:378. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12599
Abstract
Background: Osteoporotic mid-thoracic vertebral fractures (OmTVF), often result in severe pain, and neurological deficits secondary to cord compression. Cement-augmented pedicle screw (CaPS) fixation with posterior spinal decompression (PSD) offers simultaneous decompression with stabilization of these osteoporotic vertebral fractures.
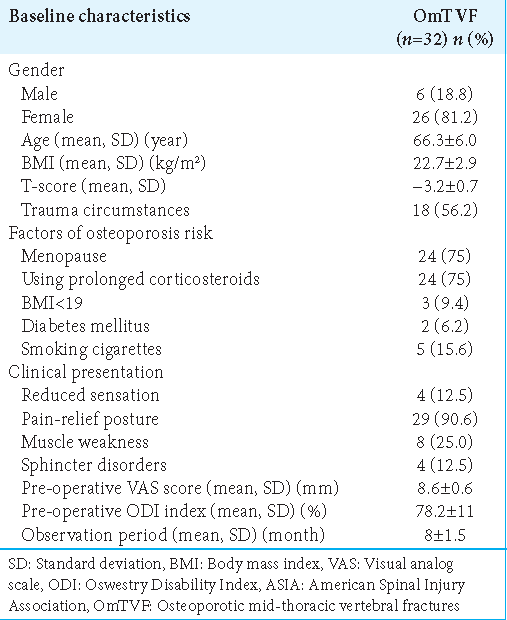
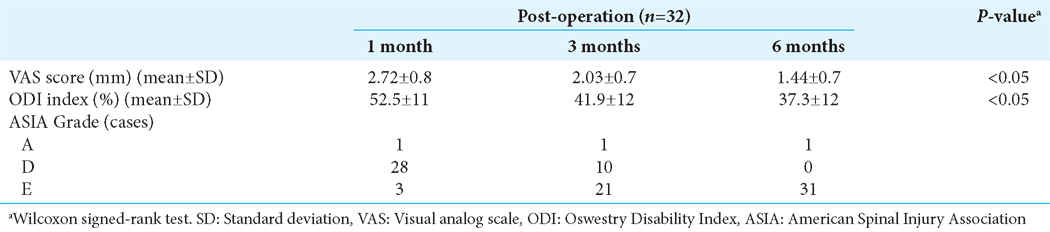
Methods: The study involved 32 patients (2022–2023) with T8–T10 osteoporotic vertebral compression fractures resulting in cord compression. All patients underwent CaPS surgery with PSD. Pain reduction was measured using the visual analog scale (VAS), and outcomes with the Oswestry Disability Index, and the American Spinal Injury Association Grades. The local kyphotic angle was also tracked with computed tomography studies performed 1, 3, and 6 months post-operatively.
Results: The average pre-operative VAS score was 8.56 mm; this decreased at 1, 3, and 6 months post-operatively to 2.72 mm, 2.03 mm, and 1.44 mm, respectively. In addition, 31 of 32 patients fully recovered within 6 postoperative months.
Conclusion: For 31 of 32 patients with T8–T10 osteoporotic vertebral fractures, CaPS fixation with PSD successfully alleviated pain and resulted in significant post-operative neurological recovery.
Keywords: Cement-augmented pedicle screw, Mid-thoracic vertebral fractures, Osteoporosis, Posterior spinal decompression
INTRODUCTION
At present, there are multiple methods for treating osteoporotic mid-thoracic vertebral fractures (OmTVF). Although conservative measures (i.e., <6 points on Blattert Fracture Score) are indicated in some cases, others with significant pain and paraparetic deficits require surgical intervention (i.e. Blatter Fracture Score >6 points).[
MATERIALS AND METHODS
Study design
This prospective study was performed at a single medical center (2022–2023). It involved 32 consecutive patients with significant neurological deficits attributed to magnetic resonance/computed tomography (CT) documented thoracic T8– T10 OmTVFs. The diagnosis of osteoporosis was based on World Health Organization criteria[
Statistical analysis
Data were examined utilizing IBM SPSS (Statistics) software 26.0 (IBM Corp., Armonk, NY, USA). Qualitative variables were shown by frequency and proportions. Wilcoxon signed-rank test assessed inter-group differences.
Ethical considerations
The hospital IRB approved data compilation, analysis, and publication of this research.
RESULTS
Outcomes
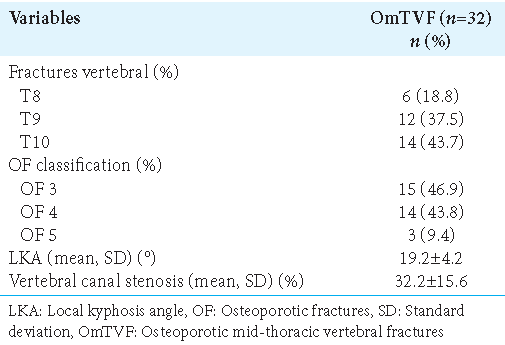
Thirty-two patients with spinal cord compression underwent CaPS with PSD for OmTVF from T8 to T10 [
Complications
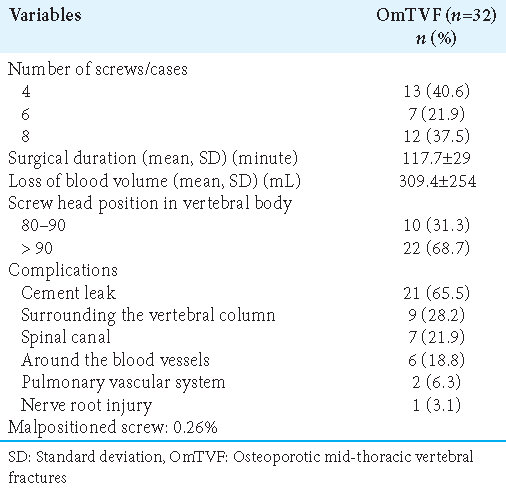
The most common complications included leakage of cement around the blood vessels and/or into the canal, or embolization of the lungs (i.e., latter 2 asymptomatic). There was one instance of nerve root damage; that patient’s deficit recovered in 6 months. There were also 5 of 190 misplaced screws.
Post-operation course
After surgery, the patient experienced significant pain relief at 1 and 3 months post-operatively, and nearly no pain at 6 postoperative months [
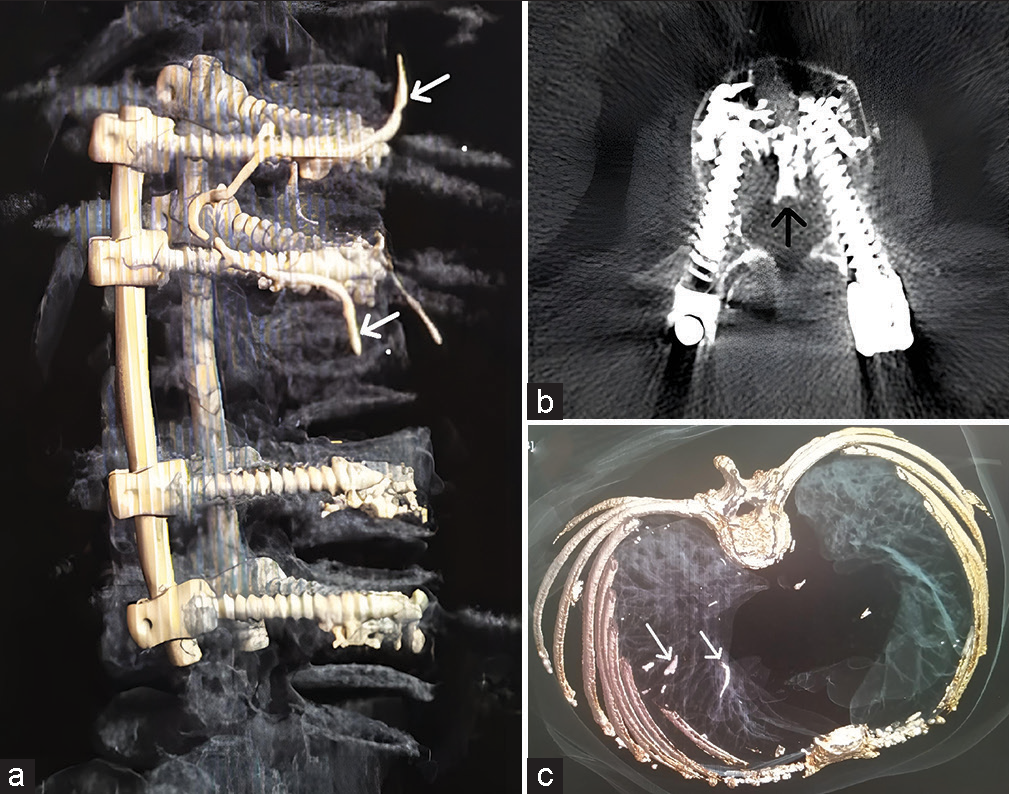
Figure 2:
A 71-year-old female patient with T8 compression fracture (T-score: −4.2) underwent a surgical procedure involving a cement-augmented pedicle screw and posterior spinal decompression. The preoperative spinal kyphotic angle (left) improved by 5° 1 month postoperatively (middle), and increased by an additional 2° at the 6-month follow-up (right).
DISCUSSION
The ultimate goal following treatment for OmVTF is pain reduction or complete pain relief.[
Measures to avoid cement-related CaSP complications
Our most frequent complication for CaSP was cement leakage around the vertebral blood vessels. To prevent cement leakage, we would recommend in the future: (1) verifying the correct positioning of screws within the vertebral body on both anteroposterior and lateral views before cement injection; (2) injecting only 2–3 mL of cement at a time, consistently monitoring with C-arm fluoroscopy; (3) immediately ceasing cement injection if leakage occurs; (4) preparing cement according to the manufacturer’s recommended ratios, avoiding excessively liquid mixtures; and (5) and avoided overfilling.
CONCLUSION
CaPS with PSD successfully achieved significant pain reduction and cord/root decompression with spinal stabilization in 31 of 32 patients with T8–T10 OmTVF.
Ethical approval
The author(s) declare that they have taken the ethical approval from IRB/IEC.
Declaration of patient consent
Patients’ consent not required as patients’ identities were not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Chen D, Jiang X. Pedicle screw fixation combined with posterior decompression and bone grafting for thoracolumbar spinal fractures can enhance curative effect and spinal cord function. Am J Transl Res. 2022. 14: 8733-40
2. Hosogane N, Nojiri K, Suzuki S, Funao H, Okada E, Isogai N. Surgical treatment of osteoporotic vertebral fracture with neurological deficit-a nationwide multicenter study in Japan. Spine Surg Relat Res. 2019. 3: 361-7
3. Kallmes DF, Schweickert PA, Marx WF, Jensen ME. Vertebroplasty in the mid-and upper thoracic spine. AJNR Am J Neuroradiol. 2002. 23: 1117-20
4. Katsumi K, Hirano T, Watanabe K, Ohashi M, Yamazaki A, Ito T. Surgical treatment for osteoporotic thoracolumbar vertebral collapse using vertebroplasty with posterior spinal fusion: A prospective multicenter study. Int Orthop. 2016. 40: 2309-15
5. Kondo KL. Osteoporotic vertebral compression fractures and vertebral augmentation. Semin Intervent Radiol. 2008. 25: 413-24
6. Mo GY, Zhou TP, Guo HZ, Li YX, Tang YC, Guo DQ. Long-term efficacy and safety of bone cement-augmented pedicle screw fixation for stage III Kummell disease. Sci Rep. 2021. 11: 13647
7. Son HJ, Choi SH, Heo DR, Kook I, Lee MK, Ahn HS. Outcomes of the use of cement-augmented cannulated pedicle screws in lumbar spinal fusion. Spine J. 2021. 21: 1857-65
8. Spiegl U, Bork H, Gruninger S, Maus U, Osterhoff G, Scheyerer MJ. Osteoporotic fractures of the thoracic and lumbar vertebrae: Diagnosis and conservative treatment. Dtsch Arztebl Int. 2021. 118: 670-7
9. Spiegl UJ, Scheyerer MJ, Osterhoff G, Gruninger S, Schnake KJ. Osteoporotic mid-thoracic vertebral body fractures: What are the differences compared to fractures of the lumbar spine?-A systematic review. Eur J Trauma Emerg Surg. 2022. 48: 1639-47
10. Suzuki N, Ogikubo O, Hansson T. The prognosis for pain, disability, activities of daily living and quality of life after an acute osteoporotic vertebral body fracture: its relation to fracture level, type of fracture and grade of fracture deformation. Eur Spine J. 2009. 18: 77-88