- Department of Neurosurgery, Universitas Airlangga Hospital, Surabaya, East Java, Indonesia.
- Department of Neurosurgery, Mitra Keluarga Satelit Hospital, Surabaya, East Java, Indonesia.
- Department of Neurosurgery, Airlangga University, Surabaya, East Java, Indonesia.
Correspondence Address:
Tedy Apriawan, Department of Neurosurgery, Universitas Airlangga Hospital, Surabaya, East Java, Indonesia.
DOI:10.25259/SNI_333_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tedy Apriawan1, Pandu Wicaksono2, Rizki Meizikri3, Eko Agus Subagio3. Emergency surgery for traumatic spinal cord injury in a secondary hospital: A case report. 27-Jul-2021;12:375
How to cite this URL: Tedy Apriawan1, Pandu Wicaksono2, Rizki Meizikri3, Eko Agus Subagio3. Emergency surgery for traumatic spinal cord injury in a secondary hospital: A case report. 27-Jul-2021;12:375. Available from: https://surgicalneurologyint.com/surgicalint-articles/10995/
Abstract
Background: Cervical spinal cord injury (SCI) is a life-threatening condition. Prompt surgical intervention is needed to avoid hemodynamic and respiratory catastrophe. In Indonesia, however, spine surgery is more common in tertiary hospitals and thus might prolong the time gap to surgery due to referral waiting time.
Case Description: We performed an emergency surgery for a patient with complete SCI due to unstable cervical fracture. The patient was in spinal shock and experienced respiratory arrest after radiological workup. Stability was achieved in the ICU and patient was directly sent to operating theater. Anterior-posterior approach was chosen to decompress and stabilize the cervical spine. The patient was discharged on postoperative day 17 and was seen well at 1-month follow-up.
Conclusion: The capability to perform spine procedures should not be exclusive to tertiary hospitals in Indonesia. Satisfying results can be achieved with the presence of capable neurosurgeons or orthopedic surgeons and anesthesiologists in lower-level hospitals.
Keywords: Cervical, Emergency surgery, Referral, Secondary hospital, Spinal cord injury
INTRODUCTION
Spinal cord injury (SCI) worsens patients’ quality of life due to its impact on sensory, motor, and autonomic function.[
Spine surgery in Indonesia is more commonly performed in a tertiary hospital. Transporting patients with SCI, however, require careful manipulation to avoid worsening the injury.[
CASE REPORT
We report a 52-year-old old female who presented to our hospital with tetraplegia for the past 1 h before admission after falling from her house’s roof, approximately 4m height. Primary survey was notable for neck pain, abdominal labored breathing, signs of spinal shock with blood pressure of 77/46 mmHg, tetraplegia, scalp laceration at right parietal, deformed left femur, flaccid anal sphincter, and absent bulbocavernosus reflex. The patient was fully conscious during the examination. Blood pressure improved after initial fluid resuscitation only to redeteriorated around 2 h afterward and therefore vasopressor was started.
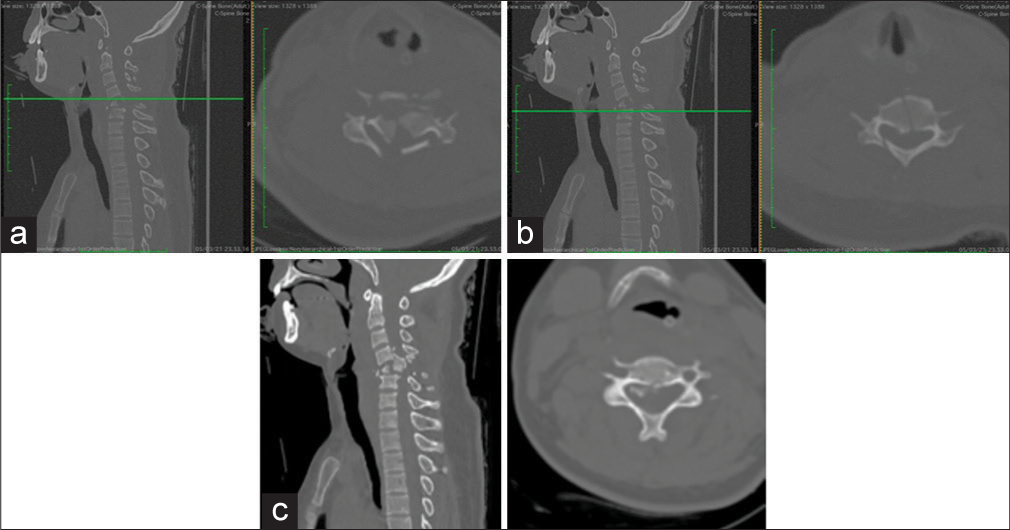
Cervical CT scan reveals a burst fracture and translational injury of C5 and split fracture of C6 [
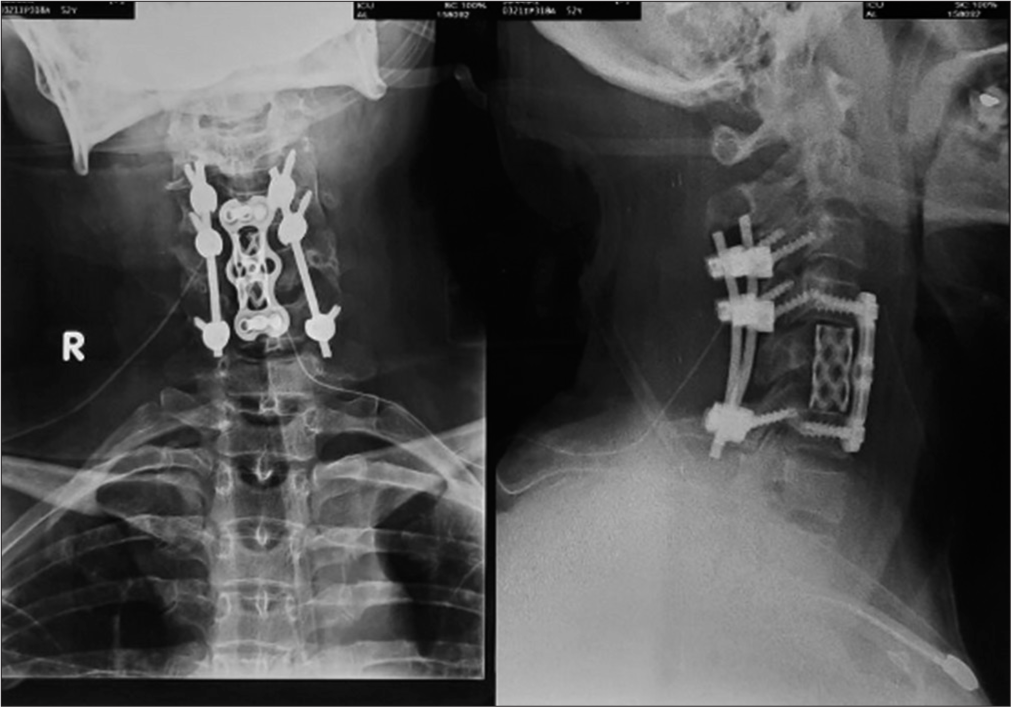
The patient was assessed with complete SCI (ASIA type A), translational injury of C5 (AOSpine C) and split fracture of C6 (AOSpine A2). Rather than looking to refer the patient, immediate surgery on the following day (22 h after admission) was preferred after respiratory and hemodynamic stability in the ICU was achieved. Combined anterior and posterior approach was preferred for this patient. Anterior cervical corpectomy and fusion with hollow cage at C5 and subsequent anterior plating were performed first. After anterior approach was completed, the patient was positioned prone for total laminectomy of C4 and C5 and lateral mass screw of C3, C4, and C6 [
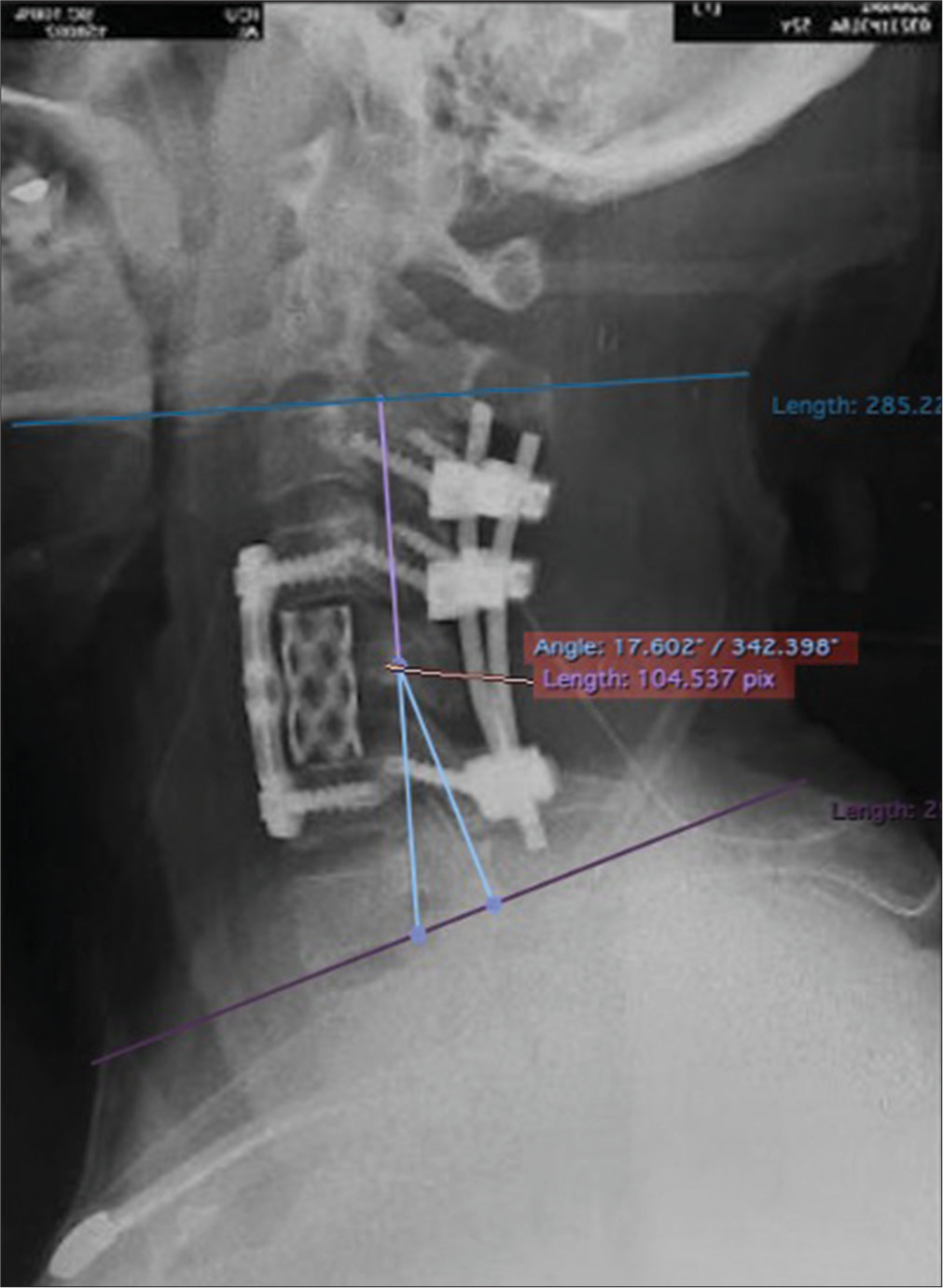
Postoperative cervical evaluation showed satisfactory position of lateral mass screw [
DISCUSSION
SCI due to cervical fracture is a life-threatening condition.[
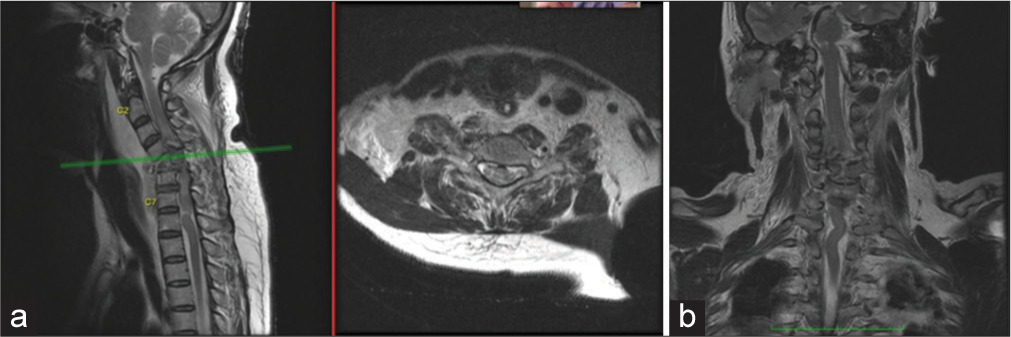
MRI was performed before surgery mainly to help prognostication and to better appreciate the involvement of ligaments and other soft tissues.[
The decision to perform surgery at our hospital was mainly based on the poor clinical condition and the radiological evidence of instability. Transporting patients with unstable hemodynamic and imminent respiratory arrest to another hospital certainly carry a substantial risk of deterioration. A cadaveric studies found that log-roll maneuver during physical examination or during an attempt to put a spinal board does not exclude the possibility of spinal column movement.[
We deem it best to stabilize the patient in the ICU and to go straight for surgery rather than refer the patient and, therefore, prolong the time gap to surgery. Given the dreadful radiological findings, however, the surgery focused more on lifesaving rather than restoring independence and mobility. Our goal was to alleviate the threat to patient’s breathing and circulation, and to allow safe mobilization to prevent further complications. After achieving relatively stable hemodynamic state, the patient was sent to the operating room at 22 h after injury. Surgery within the first 24 h has been addressed as “early surgery”[
Combined anterior and posterior approach was preferred due to (1) frank anterior pathology, (2) interlocked fracture segments behind the C4 body, (3) evidence of instability with (4) suspected posterior osteoligamentous involvement, and (5) spinal cord compression. In the present case, anterior approach was performed mainly to remove fracture segments, fuse the bone, and restore some physiological alignment. Posterior approach was mainly to stabilize and decompress. Difficulties encountered in the operating room in the present case were the occasional hemodynamic changes during surgery and positioning. Sudden hemodynamic changes (hypotension and bradycardia) during prone positioning are a known phenomenon[
Passive mobilization could be done safely after surgery. A week after surgery, the patient was cleared from the ICU. The patient developed pneumonia during hospitalization which clinically improved after antibiotic administration. As clinical and neurological condition remained stable, the patient was discharged on the 17th postoperative day for home care and further rehabilitation. The patient was seen well at the outpatient unit at 1-month follow-up.
CONCLUSION
Although spine surgery is more common in tertiary hospital in Indonesia, we successfully achieved satisfying result in the present case. Direct surgery after restoring hemodynamic stability in cervical cases should be the priority. Considering referral in such case might put the patient at risk of deterioration. The presence of neurosurgeons or orthopedic surgeons who have been trained for spine surgery, along with competent anesthesiologist in a secondary hospital, would be very helpful in treating life-threatening cervical SCI without further delay due to referral waiting time. Therefore, the capability to perform spine procedures, especially cervical ones, should not be exclusive to tertiary hospitals
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Rizki Meizikri is an awardee of Indonesia Endowment Fund for Education (Lembaga Pengelola Dana Pendidikan Republik Indonesia) and, therefore, might receive financial rewards for publishing papers on Scopus-indexed journal.
Conflicts of interest
There are no conflicts of interest.
References
1. Aarabi B, Akhtar-Danesh N, Chryssikos T, Shanmuganathan K, Schwartzbauer GT, Simard JM. Efficacy of ultra-early (< 12 h), early (12-24 h), and Late (>24-138.5 h) surgery with magnetic resonance imaging-confirmed decompression in American spinal injury association impairment scale grades A, B, and C cervical spinal cord injury. J Neurotrauma. 2020. 37: 448-57
2. Aarabi B, Sansur CA, Ibrahimi DM, Simard JM, Hersh DS, Le E. Intramedullary lesion length on postoperative magnetic resonance imaging is a strong predictor of ASIA impairment scale grade conversion following decompressive surgery in cervical spinal cord injury. Clin Neurosurg. 2017. 80: 610-20
3. Ahn H, Singh J, Nathens A, MacDonald RD, Travers A, Tallon J. Pre-Hospital care management of a potential spinal cord injured patient: A systematic review of the literature and evidence-based guidelines. J. Neurotrauma. 2011. 28: 1341-61
4. Berlowitz DJ, Wadsworth B, Ross J. Respiratory problems and management in people with spinal cord injury. Breathe. 2016. 12: 328-40
5. Bozzo A, Marcoux J, Radhakrishna M, Pelletier J, Goulet B. The role of magnetic resonance imaging in the management of acute spinal cord injury. J. Neurotrauma. 2011. 28: 1401-11
6. Chen Y, Tang Y, Vogel L, DeVivo M. Causes of spinal cord injury. Top Spinal Cord Inj Rehabil. 2013. 19: 1-8
7. Dhillon CS, Jakkan MS, Dwivedi R, Medagam NR, Jindal P, Ega S. Outcomes of unstable subaxial cervical spine fractures managed by posteroanterior stabilization and fusion. Asian Spine J. 2018. 12: 416-22
8. Edgcombe H, Carter K, Yarrow S. Anaesthesia in the prone position. Br J Anaesth. 2008. 100: 165-83
9. El Tecle NE, Dahdaleh NS, Hitchon PW. Timing of surgery in spinal cord injury. Spine (Phila Pa 1976). 2016. 41: E995-1004
10. Fehlings MG, Tetreault LA, Wilson JR, Kwon BK, Burns AS, Martin AR. A clinical practice guideline for the management of acute spinal cord injury: Introduction, rationale, and scope. Global Spine J. 2017. 7: 84S-94S
11. Fehlings MG, Vaccaro A, Wilson JR, Singh A, Cadotte DW, Harrop JS. Early versus delayed decompression for traumatic cervical spinal cord injury: Results of the surgical timing in acute spinal cord injury study (STASCIS). PLoS One. 2012. 7: e32037
12. Furlan JC, Noonan V, Singh A, Fehlings MG. Assessment of impairment in patients with acute traumatic spinal cord injury: A systematic review of the literature. J Neurotrauma. 2011. 28: 1445-77
13. Hachem LD, Ahuja CS, Fehlings MG. Assessment and management of acute spinal cord injury: From point of injury to rehabilitation. J Spinal Cord Med. 2017. 40: 665-75
14. Krause J, Saunders L. Risk of mortality and life expectancy after spinal cord injury: The role of health behaviors and participation. Top Spinal Cord Inj Rehabil. 2010. 16: 53-60
15. Kumar R, Lim J, Mekary RA, Rattani A, Dewan MC, Sharif SY. Traumatic spinal injury: Global epidemiology and worldwide volume. World Neurosurg. 2018. 113: e345-63
16. McGuire RA, Neville S, Green BA, Watts C. Spinal instability and the log-rolling maneuver. J Trauma. 1987. 27: 525-31
17. Middleton JW, Dayton A, Walsh J, Rutkowski SB, Leong G, Duong S. Life expectancy after spinal cord injury: A 50-year study. Spinal Cord. 2012. 50: 803-11
18. Park JH, Kwon JY, Lee SE, Kim YH, Kim SH. Sudden hemodynamic collapse after prone positioning on a Jackson spinal table for spinal surgery. Korean J Anesthesiol. 2020. 73: 71-4
19. Poon KS, Wu KC, Chen CC, Fung ST, Lau AW, Huang CC. Hemodynamic changes during spinal surgery in the prone position. Acta Anaesthesiol Taiwan. 2008. 46: 57-60
20. Razzak AT. Early care following traumatic spinal cord injury (TSCI) in a rehabilitation centre in Bangladesh-an analysis. Asia Pac Disabil Rehabil J. 2013. 24: 64-78
21. Sekhon LH, Fehlings MG. Epidemiology, demographics, and pathophysiology of acute spinal cord injury. Spine (Phila Pa 1976). 2001. 26: S2-12
22. Song KJ, Lee SK, Ham DH, Kim YJ, Choi BW. Limitation of previous Allen classification and subaxial cervical spine injury classification (SLIC) system in distractive-extension injury of cervical spine: Proposal of modified classification system. Eur Spine J. 2016. 25: 74-9
23. Strauss DJ, DeVivo MJ, Paculdo DR, Shavelle RM. Trends in life expectancy after spinal cord injury. Arch Phys Med Rehabil. 2006. 87: 1079-85
24. Tanaka C, Tagami T, Kaneko J, Fukuda R, Nakayama F, Sato S. Early versus late surgery after cervical spinal cord injury: A Japanese nationwide trauma database study. J Orthop Surg Res. 2019. 14: 302
25. ter Wengel PV, de Haan Y, Feller RE, Oner FC, Vandertop WP. Complete traumatic spinal cord injury: Current insights regarding timing of surgery and level of injury. Global Spine J. 2020. 10: 324-31
26. van Middendorp JJ, Hosman AJ, Pouw MH, van de Meent H. ASIA impairment scale conversion in traumatic SCI: Is it related with the ability to walk? A descriptive comparison with functional ambulation outcome measures in 273 patients. Spinal Cord. 2009. 47: 555-60
27. Wilson JR, Witiw CD, Badhiwala J, Kwon BK, Fehlings MG, Harrop JS. Early surgery for traumatic spinal cord injury: Where are we now?. Global Spine J. 2020. 10: 84S-91S
28. Yelamarthy PK, Chhabra HS, Vaccaro A, Vishwakarma G, Kluger P, Nanda A. Management and prognosis of acute traumatic cervical central cord syndrome: Systematic review and spinal cord society-spine trauma study group position statement. Eur Spine J. 2019. 28: 2390-407