- Department of Neurosurgery, University of Arizona, Tucson, United States
- College of Medicine, The University of Arizona College of Medicine - Tucson, United States
- Department of Cellular and Molecular Medicine, University of Arizona, Tucson, United States
- Global Neurosurgical Alliance, Tucson, Arizona, United States
- College of Medicine, The University of Arizona College of Medicine - Phoenix, Arizona, United States.
Correspondence Address:
Martin Weinand, Department of Neurosurgery, University of Arizona, Tucson, Arizona, United States.
DOI:10.25259/SNI_624_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Albert Alan1,2,3,4, Michelle Ennabe3,4,5, Neil Joshi1, Martin Weinand1,2. Emotional intelligence in neurosurgery: Mitigating burnout and enhancing performance. 15-Sep-2023;14:326
How to cite this URL: Albert Alan1,2,3,4, Michelle Ennabe3,4,5, Neil Joshi1, Martin Weinand1,2. Emotional intelligence in neurosurgery: Mitigating burnout and enhancing performance. 15-Sep-2023;14:326. Available from: https://surgicalneurologyint.com/surgicalint-articles/12561/
Abstract
Background: This study underscores the high burnout rates among physicians, particularly surgical residents, attributing it to the demanding health-care ecosystem. It highlights the negative impacts of burnout, such as medical errors and increased health-care costs, while exploring the potential mitigating role of emotional intelligence (EI) and mindfulness. The research aimed to analyze the existing literature on EI in neurosurgery, focusing on its relationship with physician burnout and its potential role in healthcare leadership and residency training programs.
Methods: A comprehensive literature review was conducted using multiple databases, including PubMed, OVID Embase, and OVID Medline, using the keywords “Emotional Intelligence” and “neurosurgery.” The search duration spanned from each database’s inception to June 2023.
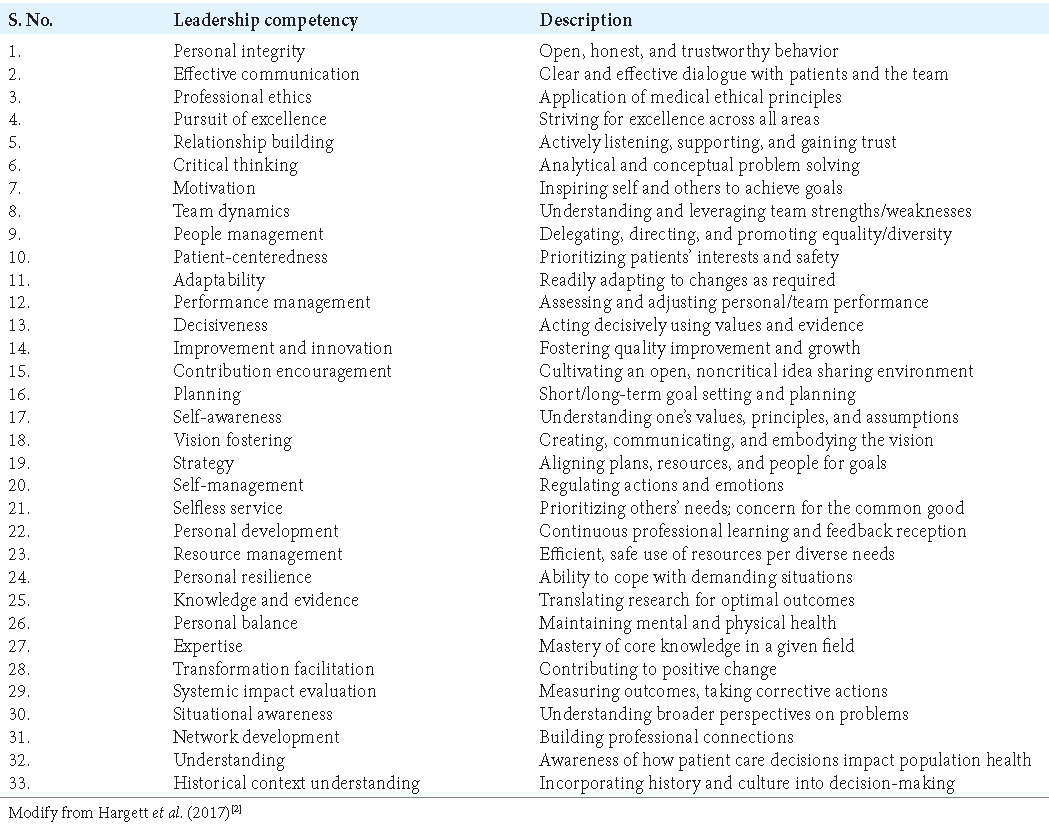
Results: The review highlighted various studies emphasizing the importance of integrating EI and mindfulness training into medical education and leadership, suggesting that a balance between technical competencies and interpersonal skills are critical. It identified personal integrity, effective communication, professional ethics, pursuit of excellence, relationship building, and critical thinking as key competencies for health-care leadership.
Conclusion: EI and a growth mindset play a critical role in managing burnout, enhancing job satisfaction and performance, and promoting effective healthcare leadership. The review, however, acknowledges certain limitations such as small sample sizes, single-institution experiences, potential biases, and inconsistencies in burnout parameters and EI measurement tools. Despite these, it points toward potential areas for future investigation and highlights the importance of standardized EI measurement tools and robust quantitative assessment methods.
Keywords: Emotional intelligence, Health-care leadership, Mindfulness training, Neurosurgical leadership, Physician burnout
INTRODUCTION
The health-care environment is a highly demanding ecosystem that requires physicians to excel in diverse roles due to high stress, rapidly evolving regulations, and escalating responsibilities.[
Physician burnout has serious consequences, including higher rates of major medical errors, escalating health-care costs, and even suicidal ideation among health-care providers.[
Despite the promising associations, traditional evaluation methods for residents typically do not directly assess EI, and medical education and professional training often lack interventions to improve EI.[
Hence, it is increasingly evident that EI, along with mindfulness, another skill closely linked to managing high-stress situations, could provide solutions in this evolving health-care environment.[
MATERIALS AND METHODS
A literature review was conducted to investigate the current corpus of research pertaining to EI in neurosurgery. This thorough investigation involved searching multiple databases such as PubMed, OVID Embase, and OVID Medline. The search duration encompassed the period from the establishment of each individual database up until June 2023. The primary search strategy employed the keywords “Emotional Intelligence” and “neurosurgery” to retrieve relevant studies and articles.
RESULTS
The third entry in the table depicted a study by Richards et al.[
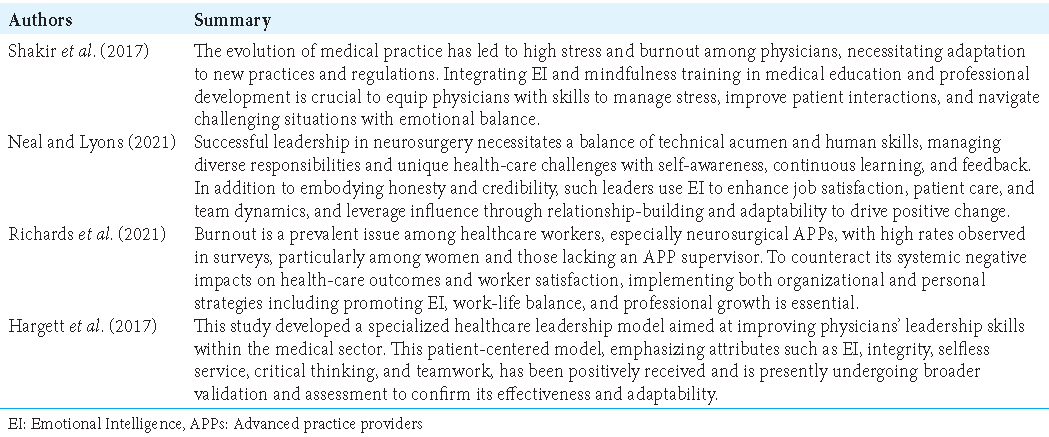
The collective findings presented in
DISCUSSION
The integration of EI and mindfulness training into medical education, the maintenance of technical and interpersonal competencies in neurosurgical leadership, the management of burnout through a combination of organizational and individual strategies, and the adoption of a comprehensive healthcare leadership model emerged as significant themes in
The phenomenon of burnout and the importance of EI in the health-care field have gained substantial attention in recent years, particularly in the context of medical residency and leadership. The studies discussed herein indicate that EI and mindset are vital factors influencing the well-being and job satisfaction of physicians, particularly those undergoing residency or practicing in demanding surgical disciplines.[
Interestingly, a growth mindset is associated with higher motivation, improved test scores, and reduced stress.[
The Accreditation Council for Graduate Medical Education (ACGME) mandates six core competencies, and the integration of EI and mindset education could enhance the acquisition of these competencies.[
Given that neurosurgical leaders play a crucial role in fostering supportive environments and influencing organizational culture, their EI, and mindset assume paramount importance.[
This comprehensive literature review is not without inherent limitations. First, the review heavily relies on studies that possess certain inherent constraints, such as significant sample size restrictions. These limitations can potentially impact the generalizability of the findings. In addition, a substantial portion of the studies included in the review are based on single-institution experiences, which may limit the external validity of the conclusions. Moreover, several studies incorporated in the review employ a cross-sectional design, which inherently limits the establishment of causal relationships and longitudinal insights. Furthermore, it is important to consider that certain studies within the review may have potential response biases and selection biases. These biases can introduce distortions and influence the outcomes, thereby warranting caution when interpreting the results.
Another noteworthy challenge is the absence of universally accepted parameters for defining burnout, which hinders the ability to draw definitive conclusions. The lack of standardized criteria may lead to variations in the identification and classification of burnout, posing difficulties in synthesizing the literature. Furthermore, the literature review encompasses studies conducted during different periods, including those carried out during the COVID-19 era. It is crucial to recognize that the pandemic may have significantly impacted the perceptions and experiences of burnout among health-care professionals. Therefore, the findings should be considered within the context of this unique and evolving situation.
In addition, it is important to highlight that the studies included in the review often employ diverse tools for measuring EI. This variability in measurement tools can limit the comparability of outcomes across different studies, making it challenging to establish consistent patterns or draw definitive conclusions. Finally, it is worth noting that the effectiveness of interventions aimed at enhancing EI is typically evaluated through subjective measures. This reliance on subjective assessments calls for the implementation of more robust and quantitative tools to assess improvements in EI, enabling a more rigorous evaluation of intervention outcomes. Recognizing and addressing these limitations are essential for the development of future research and the advancement of knowledge in the field of burnout and EI among health-care professionals.
CONCLUSION
The literature review presented in this paper underscores the indispensability of EI and a growth mindset in the realm of medical practice, with an emphasis on the sphere of neurosurgical leadership. The analysis throws light on the tangible relationship that EI and a growth mindset share with professional burnout, job contentment, and overall performance within the profession. The integration of EI and mindfulness training into medical education and the cultivation of a growth mindset have surfaced as critical themes. Their incorporation stands to contribute meaningfully to decreased instances of burnout, enhanced patient relationships, and the fostering of an effective teaching environment. Furthermore, these elements are seen to be integral in the enhancement of leadership skills and behaviors pivotal to triumph in the health-care industry.
However, while the conclusions drawn provide valuable insights, they do not stand immune to certain limitations. Constraints related to sample size, reliance on single-institution experiences, and employment of cross-sectional study designs hinder the establishment of causal relationships and limit the scope for longitudinal insights. Potential biases, such as response and selection biases, lack of universally accepted burnout parameters, and inconsistencies in EI measurement tools across different studies, further confine this review. Furthermore, the unique circumstances created by the COVID-19 pandemic and its impact on the perceptions and experiences of burnout among health-care professionals must be considered when interpreting the findings. Despite these shortcomings, the insights derived from the review provide essential areas for further investigation. Future studies should strive to counter these limitations, delve deeper into the potential of EI-centric training methods in the health-care landscape, and foster the development of standard EI measurement tools and robust quantitative assessment methods. The growth of this body of knowledge is essential to the scientific community, given the promising role of EI and a growth mindset in enhancing job satisfaction, reducing burnout, and improving patient care. Ultimately, this holistic approach could lead to meaningful enhancements in both professional well-being and the efficiency of health-care systems.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Commentary:
You just read an excellent review on Emotional Intelligence in Neurosurgery. I congratulate the authors for their initiative.
Emotional Intelligence is an elusive subject; a lecture or a textbook fails to capture the totality of its meaning. Medical schools teach students bedside manners and a professional code of conduct. Later, in the residency, the young physician discovers the foundations of the specialty, including the nuances of the techniques, those little details that we can call the “touch.” Unfortunately, neither at the medical school nor at the residency the budding physician will receive instructions about developing that other “touch” Emotional Intelligence. And this is not their fault; Emotional Intelligence is a transmissible condition acquired through repeated exposure.
I will share with you one of the instances that set for me standards of behavior.
In the third year of my residency in neurosurgery, I had the opportunity to travel to the U.S.A. and spend March as a foreign visiting fellow in a microsurgical training program at a large academic Hospital in the Midwest. Dr. A. was the chairman of the department. The other foreign fellow was a Mexican neurosurgeon. We stayed in contiguous rooms in the Nurse’s Home, adjacent to the Hospital.
Every day we went to the microsurgical laboratory, and late in the afternoon, we walked toward the Hospital to observe the clinical-radiological round. We sat in the back row of the room, behind residents from two specialties, a clinical fellow, and the faculty of neurosurgery and radiology. Ideas and opinions glided smoothly between the chairman, the faculty, and the residents. It was not a volley of “very interesting, but completely wrong interpretation of anatomy and physiology,” instead was “It didn’t occur to me that approach but tell us what you think about this way that incorporates some of your suggestions.”
With my colleague and later dear friend, we sensed that the department’s chairman installed the tenor and manner of the clinical rounds in the faculty and resident. Two events in the waning days of my stay reinforced our assumption.
One night, we met Mr. F, who introduced himself as the husband of a patient the chairman had operated on a few days ago. On the day of her discharge, Mr. F. asked Dr. A. how he could express his gratitude. The chairman said he knew two foreign fellows in the microsurgical laboratory whom he did not have the chance to take to dinner. Would Mr. F be kind and take us to dinner?
Two days after, while I was having lunch at the hospital cafeteria, Dr. A. approached me, and after asking my permission, he sat next to me and told me that due to an unexpected event, he would leave town the next morning. He would not be around the day I returned to my country. He thanked me for coming from far away and wished me the best of luck with my career. I had zero publications, and my contribution to micro neurosurgery at that Hospital was a row of poorly sutured surgical gloves. We should not reduce Emotional Intelligence to just a helpful tool for installing collegiality in a department; it is a state of mind that spreads into everyday activities, including but not limited to the operating room or clinical grand rounds.
Emotional intelligence skills are not teachable but transmissible. We must treasure those who are the depository of this vital component of the human condition.
Jorge A. Lazareff, M.D.
Emeritus Professor of Neurosurgery, Department of Neurosurgery, David Geffen School of Medicine, University of California, Los Angeles.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Cofer KD, Hollis RH, Goss L, Morris MS, Porterfield JR, Chu DI. Burnout is associated with emotional intelligence but not traditional job performance measurements in surgical residents. J Surg Educ. 2018. 75: 1171-9
2. Hargett CW, Doty JP, Hauck JN, Webb AM, Cook SH, Tsipis NE. Developing a model for effective leadership in healthcare: A concept mapping approach. J Healthc Leadersh. 2017. 9: 69-78
3. Johnson JM, Stern TA. Teaching residents about emotional intelligence and its impact on leadership. Acad Psychiatry. 2014. 38: 510-3
4. Lambert JA, Vanderbilt AA, Papadimos TJ. Improved emotional intelligence in perioperative care through simulation-based medical education during anesthesiology residency training: A call for implementation. Adv Med Educ Pract. 2019. 10: 39-42
5. Neal MT, Lyons MK. Empowering qualities and skills for leaders in neurosurgery. Surg Neurol Int. 2021. 12: 9
6. Richards AE, Curley KL, Zhang N, Bendok BR, Zimmerman RS, Patel NP. Burnout and emotional intelligence in neurosurgical advanced practice providers across the United States: A cross-sectional analysis. World Neurosurg. 2021. 155: e335-44
7. Serebrakian AT, Petrusa ER, McKinley SK, Ortiz R, Austen WG, Phitayakorn R. Evaluating and comparing emotional intelligence and improvement mindset of plastic surgery residents. J Surg Res. 2021. 268: 750-6
8. Shakir HJ, Recor CL, Sheehan DW, Reynolds RM. The need for incorporating emotional intelligence and mindfulness training in modern medical education. Postgrad Med J. 2017. 93: 509-11