- Department of Neurosurgery, Cairo University, Cairo, Egypt.
- Department of Ear Nose and Throat, Cairo University, Cairo, Egypt.
Correspondence Address:
Mohamed A. R. Soliman
Department of Neurosurgery, Cairo University, Cairo, Egypt.
DOI:10.25259/SNI_547_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohamed A. R. Soliman1, Mohammad Elbaroody1, Amr K. Elsamman1, Mohamed Ibrahim Refaat1, Ehab Abd-Haleem1, Walid Elhalaby1, Hazem Gouda1, Amr Safwat1, Mohamed El Shazly1, Hisham Lasheen2, AbdelRahman Younes2, Yousry El-Hemily1, Ahmed Elsaid1, Haitham Kandel1, Mohamed Lotfy1, Ehab El Refaee1. Endoscopic endonasal skull base surgery during the COVID-19 pandemic: A developing country perspective. 25-Sep-2020;11:310
How to cite this URL: Mohamed A. R. Soliman1, Mohammad Elbaroody1, Amr K. Elsamman1, Mohamed Ibrahim Refaat1, Ehab Abd-Haleem1, Walid Elhalaby1, Hazem Gouda1, Amr Safwat1, Mohamed El Shazly1, Hisham Lasheen2, AbdelRahman Younes2, Yousry El-Hemily1, Ahmed Elsaid1, Haitham Kandel1, Mohamed Lotfy1, Ehab El Refaee1. Endoscopic endonasal skull base surgery during the COVID-19 pandemic: A developing country perspective. 25-Sep-2020;11:310. Available from: https://surgicalneurologyint.com/surgicalint-articles/10283/
Abstract
Background: Although primarily a respiratory disorder, the coronavirus pandemic has paralyzed almost all aspects of health-care delivery. Emergency procedures are likely continuing in most countries, however, some of them raises certain concerns to the surgeons such as the endoscopic endonasal skull base surgeries. The aim of this study is to present the current situation from a developing country perspective in dealing with such cases at the time of the COVID-19 pandemic.
Methods: A cross-sectional analytical survey was distributed among neurosurgeons who performed emergency surgeries during the COVID-19 pandemic in Cairo, Egypt, between May 8, 2020, and June 7, 2020. The survey entailed patients’ information (demographics, preoperative screening, and postoperative COVID-19 symptoms), surgical team information (demographics and postoperative COVID-19 symptoms), and operative information (personal protective equipment [PPE] utilization and basal craniectomy).
Results: Our survey was completed on June 7, 2020 (16 completed, 100% response rate). The patients were screened for COVID-19 preoperatively through complete blood cell (CBC) (100%), computed tomography (CT) chest (68.8%), chest examination (50%), C-reactive protein (CRP) (50%), and serological testing (6.3%). Only 18.8% of the surgical team utilized N95 mask and goggles, 12.5% utilized face shield, and none used PAPRs. Regarding the basal craniectomy, 81.3% used Kerrison Rongeur and chisel, 25% used a high-speed drill, and 6.3% used a mucosal shaver. None of the patients developed any COVID-19 symptoms during the first 3 weeks postsurgery and one of the surgeons developed high fever with negative nasopharyngeal swabs.
Conclusion: In developing countries with limited resources, preoperative screening using chest examination, CBC, and CT chest might be sufficient to replace Reverse transcription polymerase chain reaction. Developing countries require adequate support with screening tests, PPE, and critical care equipment such as ventilators.
Keywords: Coronavirus, COVID-19, Developing Countries, Endoscopic, Skull base, Trans-sphenoid
INTRODUCTION
The coronavirus (COVID-19) pandemic has affected virtually all aspects of human existence with social and psychological repercussions that generations have not witnessed. It has devastated the world economy through massive layoffs, business disruption, and collapse of financial markets. Elective surgeries at all levels have been suspended and dayto-day interactions have changed as the virus is projected to afflict large portions of the world’s population.[
Severe acute respiratory syndrome coronavirus-2 (SARSCoV-2) was first identified in Wuhan, China, in December 2019.[
The impact on health care has also varied ranging from continued routine services to almost complete shutdown. Responses have largely varied by region, but also by where a community is temporally on the epidemic curve. In many countries, patients are finding nonemergency services cancelled or delayed including consultations and elective surgeries. In other regions, more aggressive measures have been taken suspending all nonemergency procedures.[
Emergency procedures are likely continuing in most countries, however, some of them raises certain concerns to the surgeons such as the endoscopic endonasal skull base surgeries which carries an additional risk of the sinuses harboring a high COVID-19 viral load as well as potential aerosolization during endoscopic endonasal instrumentation.[
When health care has to be delivered, it is incumbent on our institutions to provide such care in the safest manner possible. This has been another challenge across the planet with the lack of availability of essential testing, medical equipment, and personal protective equipment (PPE), especially in low-income countries. A worldwide survey study was conducted during the current pandemic and was published recently showing that 12% of the neurosurgeons did not utilize PPE while dealing with the patients. This was more common in the developing countries.[
The aim of this study is to present the current situation from a developing country perspective in dealing with emergency endoscopic endonasal skull base surgeries at the time of the COVID-19 pandemic in terms of preoperative patients’ screening, surgical techniques, and intraoperative PPE utilization.
MATERIALS AND METHODS
Study design and participants
We conducted a cross-sectional analytical survey study to take a snapshot of the situation of the emergency endoscopic endonasal skull base surgeries during the COVID-19 pandemic in a developing country. To elicit prompt responses, data collection was performed electronically.
The survey was distributed electronically (Facebook Messenger and WhatsApp) among neurosurgeons from Cairo University, Egypt, who performed an urgent endoscopic endonasal skull base surgeries during the COVID-19 pandemic. We collected data between May 8, 2020, and June 7, 2020.
The survey was administered through Google Forms (Google, Mountain View, CA, USA). All responses were collated with Excel (Microsoft, Redmond, WA, USA) and cross-verified by three members of our team.
Data collection tool
The survey consisted of 12 questions designed to explore three domains; patients’ information (age, clinical manifestations [neurological and COVID-19 related], diagnosis, preoperative COVID-19 screening, and COVID-19 symptoms during the first 3 weeks postsurgery), surgical team information (age, chronic medical conditions, and COVID-19 symptoms during the first 3 weeks postsurgery), and operative information (PPE utilization and basal craniectomy). The questions were in a checkboxes format so they can choose multiple answers.
COVID-19-related symptoms included any of the following symptoms; fever, new onset of cough, worsening chronic cough, shortness of breath, difficulty breathing, sore throat, hoarse voice, difficulty swallowing, decrease or loss of sense of taste/smell, chills, headaches, unexplained fatigue/malaise/ muscle aches, diarrhea, abdominal pain, nausea/vomiting, pink eye (conjunctivitis), runny nose/sneezing without other known cause, and nasal congestion without other known cause.
We first drafted a pilot survey and administered this to two neurosurgeons. Based on their feedback, the survey was revised before full administration.
Data analysis
We used SPSS (V24, IBM Corp., USA) for data analysis. Descriptive statistics were used to summarize quantitative data and histograms for qualitative data.
Ethical consideration
Neurosurgeons were informed first about the objectives of this survey and then had the option of not participating. We maintained strict confidentiality regarding participant responses and personal data (Helsinki Declaration[
RESULTS
This manuscript was prepared in accordance with Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guidelines.[
Patients’ data
Demographics and diagnosis
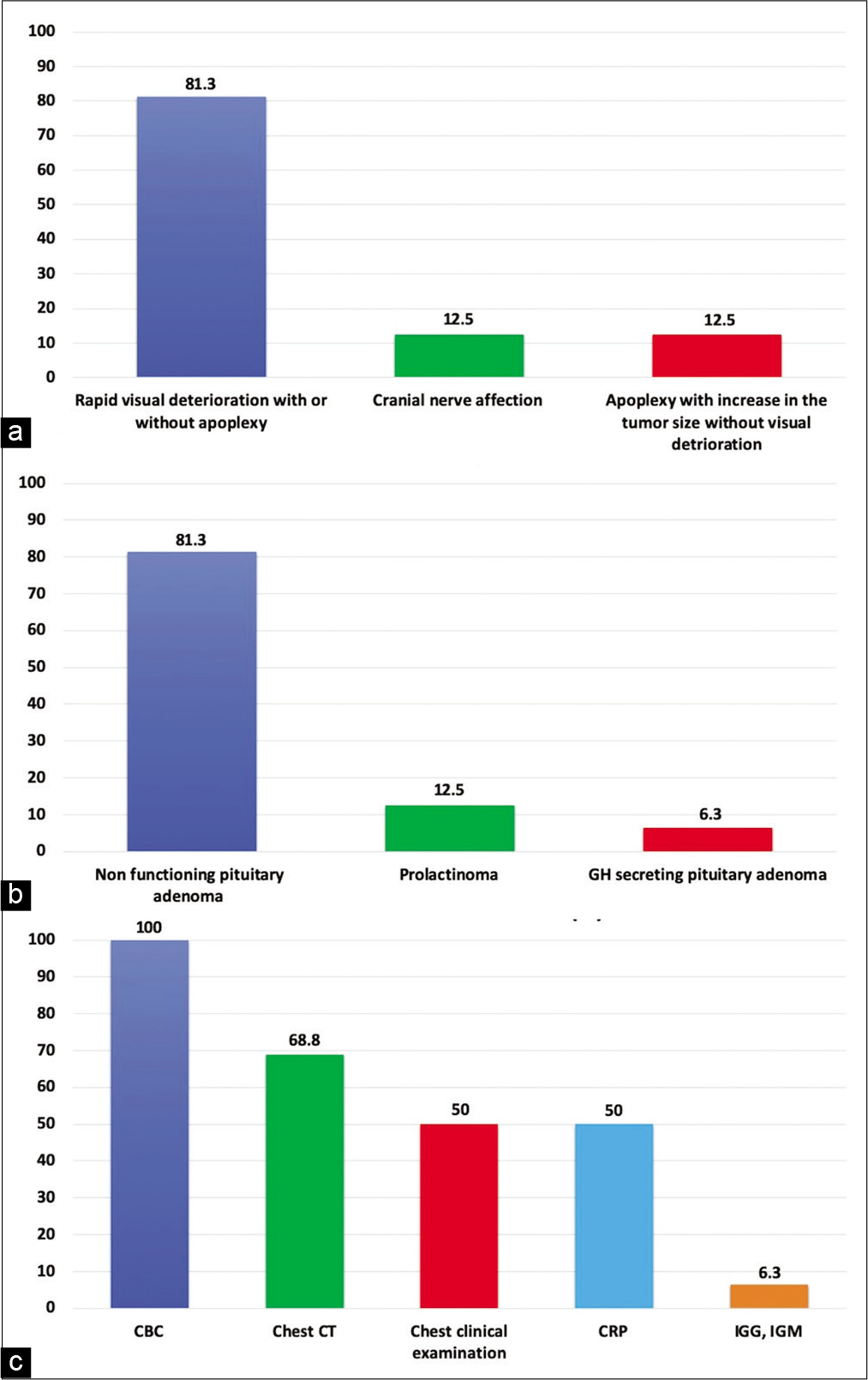
The mean age of the patients was 44.9 ± 17.7 years (range, 8–78 years) with 18.8% (n = 3) above the age of 60 years. About 81.3% (n = 13) of the patients presented by rapid visual deterioration (one of them was associated with cranial nerve deficit), 12.5% (n = 2) presented with pituitary apoplexy without visual deterioration, and 6.3% (n = 1) presented with cranial nerve deficit only [
Preoperative screening
All of the patients were screened by a preoperative complete blood picture and plain chest X-ray. While only 68.8% (n = 11) of the patients were screened through a CT chest, 50% (n = 8) through chest examination, 50% (n = 8) through C-reactive protein (CRP), and only 6.3% (n = 1) through immunoglobulins serological testing [
Postoperative COVID-19-related symptoms
None of the patients developed any manifestation of COVID-19 such as fever or pneumonia-related symptoms during the first 3 weeks after surgery.
Surgical team data
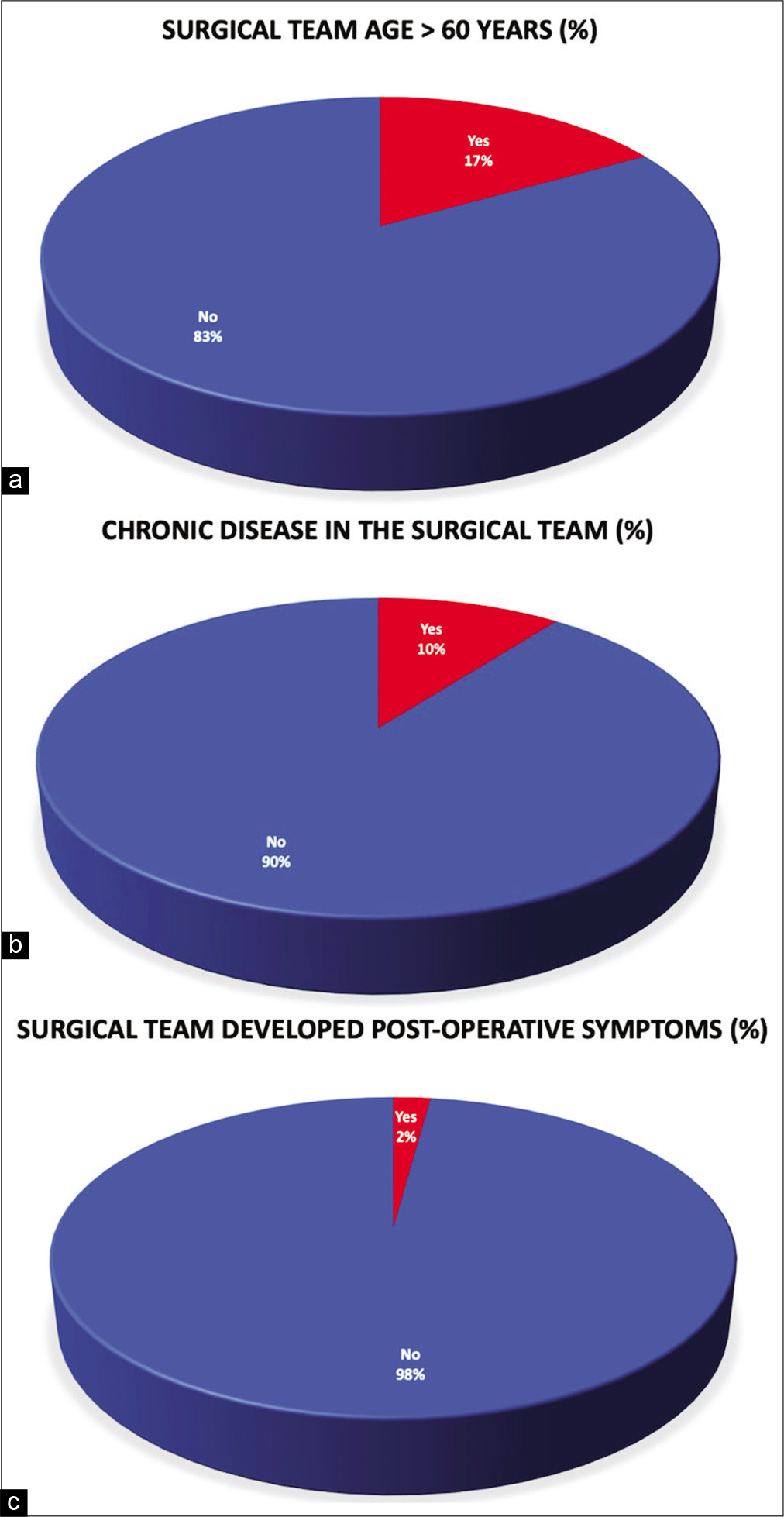
About 16.7% (n = 8) of the surgical team were above 60 years old [
Figure 2:
Surgical team information (multiple answers were allowed). (a) A pie chart graph showing the percentage of the surgical team that was above 60 years at the time of the surgery. (b) A pie chart graph showing the percentage of the surgical team that was having chronic medical conditions at the time of the surgery. (c) A pie chart graph showing the percentage of the surgical team that presented with COVID-19 symptoms during the first 3 weeks postsurgery.
Operative data
PPE utilization
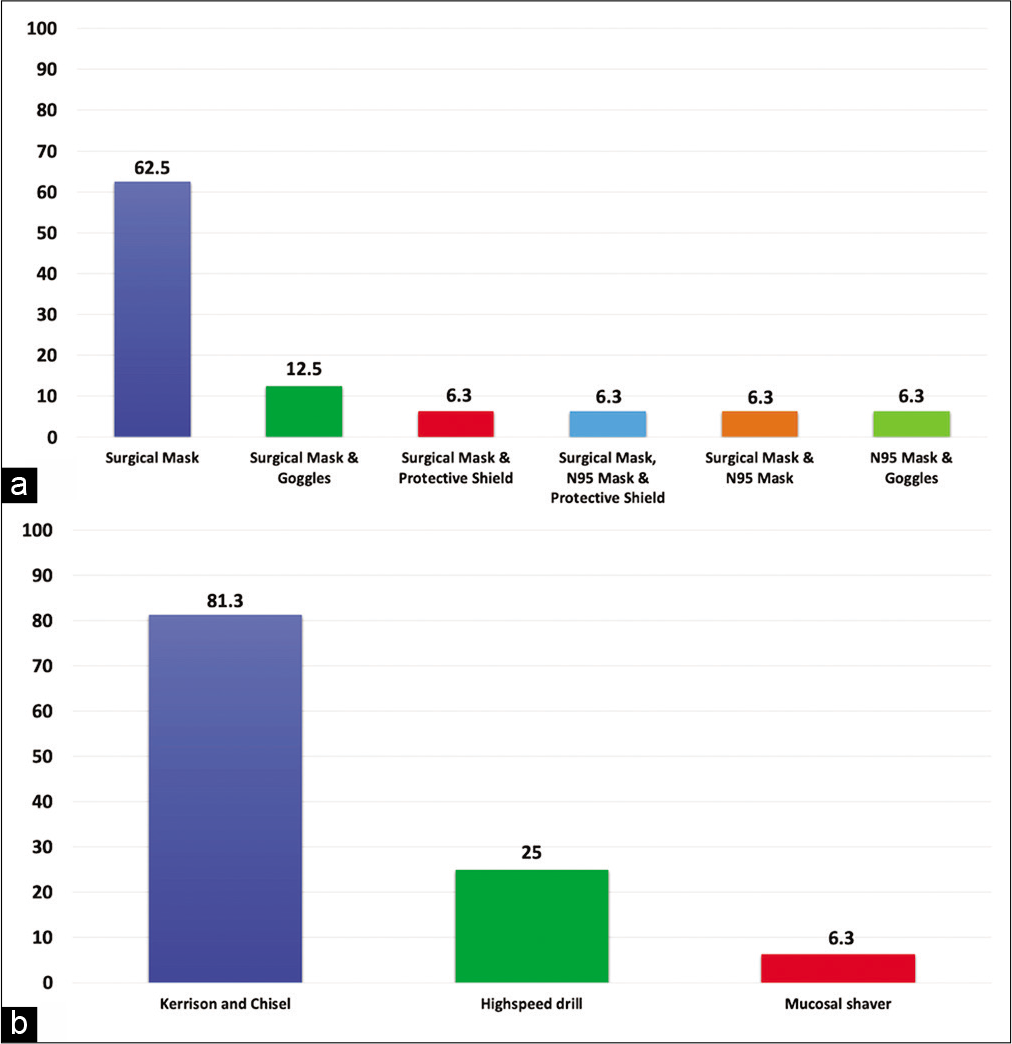
About 62.5% (n = 30) of the surgical team used regular surgical masks only covering nose and mouth, while only 12.5% (n = 6) used regular surgical mask and goggle, and only 6.3% (n = 3) of the surgeons used regular surgical mask with protective shield, regular surgical mask, protective shield, and N95 mask, regular surgical mask and N95 mask, or N95 mask only [
Basal craniectomy
Regarding the basal craniectomy, 81.3% (n = 13) used Kerrison Rongeur and chisel, 25% (n = 4) used a high-speed drill, and 6.3% (n = 1) used a mucosal shaver. There was only one case where the surgeons used the Kerrison Rongeur, chisel, high-speed drill, and mucosal shaver [
DISCUSSION
The COVID-19 pandemic has been a major threat to global health care. The impact on health systems worldwide is unprecedented. All areas of medicine have had to undergo rapid transformation. Nonessential care has been eliminated in many regions and continues unscathed in some places. Preparedness for this crisis also has varied by nation. A worldwide survey study was conducted during the current pandemic showed that hospitals from low-income countries were insufficiently prepared.[
When health care has to be delivered, it is incumbent on our institutions to provide such care in the safest manner possible. This has been a challenge in developing countries with the lack of availability of essential screening tests (PCR) and PPE. Physicians, nurses, and other health care workers are stressed for these reasons. Furthermore, the lack of treatments, incomplete understanding of the disease, absence of a vaccine, and misinformation have further compounded this stress.
Now in the midst of the pandemic, health-care facilities in developing countries are overwhelmed by COVID-19 patients. These hospitals were already overcrowded with patients suffering from acute and chronic medical conditions and patients requiring surgical treatment. Furthermore, developing countries will not be able to reduce significantly the surgical volumes to make room for patients with COVID-19. This is due to the largest portion of the surgical volume in developing countries cannot be postponed safely due to their urgent and emergent nature.[
The Egyptian authorities announced the first case infected with COVID-19 on February 14, 2020.[
Emergency procedures were continued similar to most countries, however, there are some of these procedures require more precaution due to high viral load of the SARSCoV-2 in the upper airway with potential aerosolization during the procedure such as endoscopic endonasal surgeries.[
Demographics
According to reports from the CDC, Italy and China, patients with underlying chronic medical problems and the elderly are associated with more severe COVID-19 disease.[
Preoperative screening
Tedros Ghebreyesus, the World Health Organization (WHO) chief executive, said, “You cannot fight a fire blindfolded” and his key message was “test, test, test.” The WHO has criticized countries that have not prioritized COVID-19 testing.[
About 30% of asymptomatic patients and 56% of mildly symptomatic patients can transmit SARS-CoV-2 infection.[
In developing countries such as Egypt with limited testing for the SARS-CoV-2,[
The basic clinical examination, CBC, CRP, and chest imaging were the main preoperative diagnostic tools used and created convenient prophylactic measures that served in operating on 16 urgent patients at the time of the pandemic uprise in Egypt without any report for a surgery-related spread of infection.
Intraoperative PPE utilization
There is enormous demand for PPE around the world and will be more difficult in obtaining them in developing countries. The endoscopic trans-sphenoid surgery creates clouds of aerosols and droplets which may contaminate the operating theater environment when operating on a positive COVID-19 patient.[
Despite all these measures including N95 respirator utilization, in Wuhan, the ENT surgeons were one of the worst specialties affected.[
Basal craniectomy
The SARS-CoV-2 aerosolization during upper airway procedures and sinonasal procedures is very high, especially with the use of powered instruments such as drills and debriders due to the upper airway high viral load.[
Postoperative care
Our recommendation is to deal with the patient as suspected COVID-19 positive as long as we are not able to perform an RT-PCR nasal swab to them. All the patients are transferred to the regular single-bed room for isolation and postoperative care. Daily body temperature assessment and respiratory history were done and in consistence with recommendations.[
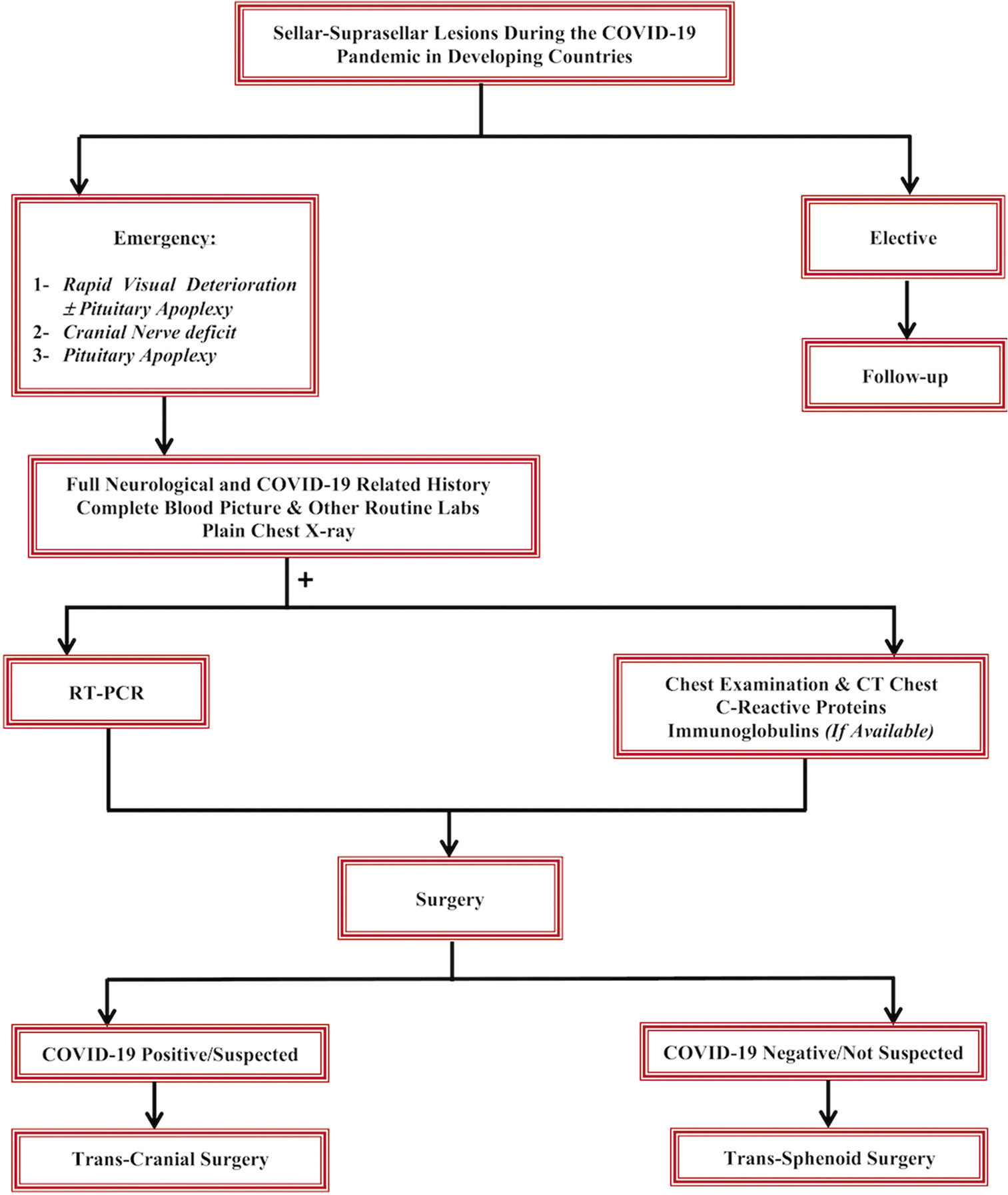
Limitations
At the time of this submission, the situation is rapidly evolving in our country, and all of the above policies might change in the near future. Furthermore, fortunately, all our cases did not present with COVID-19-related symptoms whether pre- or postoperative which might be due to asymptomatic form of the disease or they are COVID-19 negative despite that most cases were during the uprise of COVID-19 reported cases in Egypt. This series of patients is from single-center surgeons and there might be other COVID-19 confirmed positive cases operated n in other centers. Although this study was discussing the urgent trans-sphenoid skull base cases that were operated on during this pandemic, it is missing the number of nonurgent cases that presented to our clinics or emergency department with clinical signs of COVID-19. However, in case of a patient that requires urgent surgery and is clinically or radiographically suspected of COVID-19, an urgent craniectomy will be indicated [
CONCLUSION
The surgeons’ safety should be placed at the highest priority and the governments should balance the limited resources and surgeons’ safety. The idea of waking-up nearly every week on a loss of one of the neurosurgical or skull base teams to this virus is terrifying. We highlight the situation of urgent endoscopic skull base practice from a developing country with limited resources, preoperative screening using chest clinical history and examination, CBC, and CT chest might be sufficient to replace RT-PCR. All patients should be managed as suspected COVID-19 until 2 weeks postsurgery with enhanced PPE whenever possible and avoiding power drills whenever possible. If the patient requires urgent surgery and the above test are suggesting COVID-19, transcranial excision is recommended. Developing countries require adequate support with screening tests, PPE (N95 masks and PAPRs), and critical care equipment such as ventilators.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. American Academy of Otolaryngology-Head and Neck Surgery. Available from: https://www.entnet.org/content/academy-supports-cms-offers-specific-nasal-policy [Last accessed on 2020 May 22].
2. Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W. Correlation of chest CT and RT-PCR testing for coronavirus disease 2019 (COVID-19) in China: A report of 1014 cases. Radiology. 2020. 296: E32-40
3. Al-Balas M, Al-Balas HI, Al-Balas H. Surgery during the COVID-19 pandemic: A comprehensive overview and perioperative care. Am J Surg. 2020. 219: 903-6
4. Aminian A, Safari S, Razeghian-Jahromi A, Ghorbani M, Delaney CP. COVID-19 outbreak and surgical practice: Unexpected fatality in perioperative period. Ann Surg. 2020. 272: e27-9
5. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet. 2020. 395: 912-20
6. Castelnuovo P, Turri-Zanoni M, Karligkiotis A, Battaglia P, Pozzi F, Locatelli D. Skull-base surgery during the Covid-19 pandemic: The Italian skull base society recommendations. Int Forum Allergy Rhinol. 2020. 10: 963-7
7. Chow N, Fleming-Dutra K, Gierke R, Hall A, Hughes M, Pilishvili T. Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019-United States February 12-March 28, 2020. MMWR Morb Mortal Wkly Rep. 2020. 69: 382-6
8. Corman VM, Landt O, Kaiser M, Molenkamp R, Meijer A, Chu DK. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020. 25: 2000045
9. COVID-19 and Public Health Preparedness in the United States. Available from: https://www.the-hospitalist.org/hospitalist/article/218571/coronavirus-updates/covid-19-and-public-health-preparedness-united-states [Last accessed on 2020 Apr 12]..
10. Economic Analysis and Policy Division, Department of Economic & Social Affairs, United Nations. Available from: https://www.un.org/development/desa/dpad/publication/world-economic-situation-and-prospects-april-2020-briefing-no-136 [Last accessed on 2020 Apr 12].
11. UNESCO. Available from: https://www.en.unesco.org/covid19/educationresponse [Last accessed on 2020 Apr 12].
12. . Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports [Last accessed on 2020 Apr 17].
13. American College of Surgeons. Available from: https://www.facs.org/covid-19/clinical-guidance/triage [Last accessed on 2020 Apr 12].
14. Cyranoski D.editors. ‘We need to be alert’: Scientists fear second coronavirus wave as China’s lockdowns ease. Nature. 2020. p.
15. . Available from: http://www.ems.org.eg [Last accessed on 2020 Jul 06].
16. El-Ghandour NM, Elsebaie EH, Salem AA, Alkhamees AF, Zaazoue MA, Fouda MA. Letter: The impact of the coronavirus (COVID-19) pandemic on neurosurgeons worldwide. Neurosurgery. 2020. 87: E250-7
17. Fang Y, Zhang H, Xie J, Lin M, Ying L, Pang P. Sensitivity of chest CT for COVID-19: Comparison to RT-PCR. Radiology. 2020. 296: E115-7
18. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020. 382: 1708-20
19. Hassany M, Abdel-Razek W, Asem N, AbdAllah M, Zaid H. Estimation of COVID-19 burden in Egypt. Lancet Infect Dis. 2020. 20: 896-7
20. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020. 395: 497-506
21. Huang P, Liu T, Huang L, Liu H, Lei M, Xu W. Use of chest CT in combination with negative RT-PCR assay for the 2019 novel coronavirus but high clinical suspicion. Radiology. 2020. 295: 22-3
22. Characteristics of COVID-19 Patients Dying in Italy. Report Based on Available Data on March 20th, 2020. Available from: https://www.epicentro.iss.it/coronavirus/bollettino/Report-COVID-2019_20_marzo_eng.pdf [Last accessed on 2020 Mar 20].
23. Jenkins A. Letter: Transmission of COVID-19 during neurosurgical procedures-some thoughts from the United Kingdom. Neurosurgery. 2020. 87: E68
24. Kessler RA, Zimering J, Gilligan J, Rothrock R, McNeill I, Shrivastava RK. Neurosurgical management of brain and spine tumors in the COVID-19 era: An institutional experience from the epicenter of the pandemic. J Neurooncol. 2020. 148: 211-9
25. Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng Q, Meredith HR. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: Estimation and application. Ann Intern Med. 2020. 172: 577-82
26. Li Y, Qin JJ, Wang Z, Yu Y, Wen YY, Chen XK. Surgical treatment for esophageal cancer during the outbreak of COVID-19. Zhonghua Zhong Liu Za Zhi. 2020. 42: 296-300
27. Lo YT, Yang Teo NW, Ang BT. Editorial. Endonasal neurosurgery during the COVID-19 pandemic: The Singapore perspective. J Neurosurg. 2020. 17: 1-3
28. Malelelo-Ndou H, Ramathuba DU, Netshisaulu KG. Challenges experienced by health care professionals working in resource-poor intensive care settings in the Limpopo Province of South Africa. Curationis. 2019. 42: e1-8
29. McKee M, Stuckler D. If the world fails to protect the economy, COVID-19 will damage health not just now but also in the future. Nat Med. 2020. 26: 640-2
30. Murthy S, Leligdowicz A, Adhikari NK. Intensive care unit capacity in low-income countries: A systematic review. PLoS One. 2015. 10: e0116949
31. Park J, Yoo SY, Ko JH, Lee SM, Chung YJ, Lee JH. Infection prevention measures for surgical procedures during a Middle East respiratory syndrome outbreak in a tertiary care hospital in South Korea. Sci Rep. 2020. 10: 325
32. Patel ZM, Fernandez-Miranda J, Hwang PH, Nayak JV, Dodd R, Sajjadi H. Letter: Precautions for endoscopic transnasal skull base surgery during the COVID-19 pandemic. Neurosurgery. 2020. 87: E66-7
33. Prin M, Guglielminotti J, Mtalimanja O, Li G, Charles A. Emergency-to-elective surgery ratio: A global indicator of access to surgical care. World J Surg. 2018. 42: 1971-80
34. Rapid Risk Assessment: Coronavirus Disease 2019 (COVID-19) Pandemic: Increased Transmission in the EU/EEA and the UK-Eighth Update. Available from: https://www.ecdc.europa.eu/en/publications-data/rapid-risk-assessment-coronavirus-disease-2019-covid-19-pandemic-eighth-update [Last accessed on 2020 Apr 12].
35. Siow WT, Liew MF, Shrestha BR, Muchtar F, See KC. Managing COVID-19 in resource-limited settings: Critical care considerations. Crit Care. 2020. 24: 167
36. Stahel PF. How to risk-stratify elective surgery during the COVID-19 pandemic?. Patient Saf Surg. 2020. 14: 8
37. China Newsweek. Available from: http://www.view.inews.qq.com/a/20200125A07TT200?uid=&devid=BDFE70CD-5BF1-4702-91B7-329F20A6E839&qimei=bdfe70cd-5bf1-4702-91b7-329f20a6e839 [Last accessed on 2020 May 21].
38. Tao KX, Zhang BX, Zhang P, Zhu P, Wang GB, Chen XP. Recommendations for general surgery clinical practice in novel coronavirus pneumonia situation. Zhonghua Wai Ke Za Zhi. 2020. 58: E001
39. Tins B. Technical aspects of CT imaging of the spine. Insights Imaging. 2010. 1: 349-59
40. Van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020. 382: 1564-7
41. Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ. 2007. 335: 806-8
42. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19-11 March 2020. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 [Last accessed on 2020 Apr 16].
43. . World Medical Association declaration of Helsinki, Ethical principles for medical research involving human subjects. Bull World Health Organ. 2001. 79: 373-4
44. Xie X, Zhong Z, Zhao W, Zheng C, Wang F, Liu J. Chest CT for typical coronavirus disease 2019 (COVID-19) pneumonia: Relationship to negative RT-PCR testing. Radiology. 2020. 296: E41-5
45. Xu K, Lai XQ, Liu Z. Suggestions for prevention of 2019 novel coronavirus infection in otolaryngology head and neck surgery medical staff. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2020. 55: E001
46. Zou L, Ruan F, Huang M, Liang L, Huang H, Hong Z. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020. 382: 1177-9