- Department of Minimal Invasive Neurosurgery, National Centre for Neurosurgery, Astana, Kazakhstan
- Department of Pathology, National Centre for Neurosurgery, Astana, Kazakhstan
Correspondence Address:
Murat Arlanbekov, Department of Minimal Invasive Neurosurgery, National Centre for Neurosurgery, Astana, Kazakhstan.
DOI:10.25259/SNI_1082_2024
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nurali Ashirov1, Murat Arlanbekov1, Daniyar Teltayev1, Berik Zhetpisbaev2, Serik Akshulakov1. Endoscopic resection of a giant colloid cyst in the cavum septum pellucidum: Illustrative case. 16-May-2025;16:186
How to cite this URL: Nurali Ashirov1, Murat Arlanbekov1, Daniyar Teltayev1, Berik Zhetpisbaev2, Serik Akshulakov1. Endoscopic resection of a giant colloid cyst in the cavum septum pellucidum: Illustrative case. 16-May-2025;16:186. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13554
Abstract
Background: Colloid cysts (CCs) are a rare type of benign tumor, and the ones >30 mm in diameter are determined as giant CCs. The giant CCs of the cavum septum pellucidum (CSP) are located in the hard-to-reach areas of the brain, and they can be removed microsurgically and endoscopically. At present, the transition from the microsurgical resection to the endoscopic is observed, and researchers demonstrate several benefits of the endoscopic resection over the microsurgical. We noticed the absence of research illustrating the endoscopic resection of the giant CC of the CSP. Therefore, we decided to demonstrate a rare case performed in our hospital.
Case Description: Our patient was a 57-year-old male who had suffered from dizziness, headache, nausea, urinary incontinence, short-term forgetfulness, gait ataxia, cognitive decline, and vision blurring. The eventual diagnosis of the giant CC in the CSP was established, and it was complicated by occlusive hydrocephalus and headache syndrome. The endoscopic resection of the giant CC in the septum pellucidum was performed using the endoscopic transseptal approach.
Conclusion: No complications were observed in the postoperative period. The tumor was removed completely, no recurrence was noted, and only a capsule of the tumor was observed in the control magnetic resonance imaging image taken 3 months after the operation. Considering these results, we conclude that endoscopic removal may have positive and safe outcomes as the surgical treatment method for the giant CCs located in the septum pellucidum.
Keywords: Cavum septum pellucidum, Endoscopic resection, Giant colloid cyst, Third ventricle
INTRODUCTION
Colloid cysts (CCs) are benign tumors composing 0.5–2% of all brain tumors.[
The CC was first described by Wallmann in 1858 as an autopsy finding, and Walter Dandy was the first to remove this kind of tumor in 1921 successfully.[
The septum pellucidum has two membranes separated by the cerebrospinal fluid during fetal life.[
The CC in the CSP can be removed microsurgically and endoscopically.[
CASE DESCRIPTION
Patient D is a 57-year-old male who has suffered from dizziness, headache, and nausea for 2 months but did not seek medical attention. The month before the hospitalization, he experienced symptoms such as episodes of urinary incontinence and short-term forgetfulness, gait ataxia, cognitive decline, and vision blurring. Routine laboratory tests were regular. The eventual diagnosis was the giant CC in the CSP. The main disease was complicated with occlusive hydrocephalus and headache syndrome.
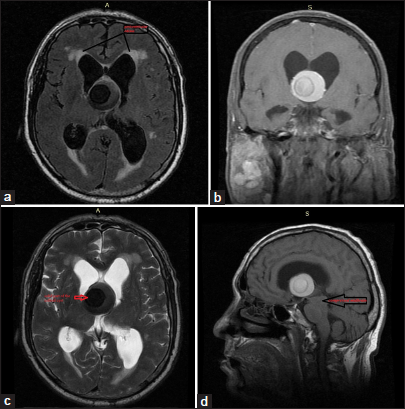
Preoperative images
On magnetic resonance imaging (MRI), a huge, uncommon appearance with the size of 30 × 31 × 35 mm was observed. It had a clear-cut heterogeneous midline. The intraventricular mass extending upwards from the interthalamic region into the lateral ventricles was detected. There was associated obstructive hydrocephalus with periventricular edema [
Figure 1:
The brain magnetic resonance imaging of the patient before the operation. (a) Axial T 2 flair; (b) T1 coronal with contrast; (c) T2 axial; and (d) T1 sagittal. (a) The arrows show the signs of a periventricular edema of the anterior corn of the lateral ventricle. (a and c) Signs of hydrocephalus and edema of the anterior and posterior horn of the lateral ventricle. (c) The arrow shows a solid part of the colloid cyst (CC). (d) The black arrow shows a giant CC, which is pressing against the midbrain from above.
Operation
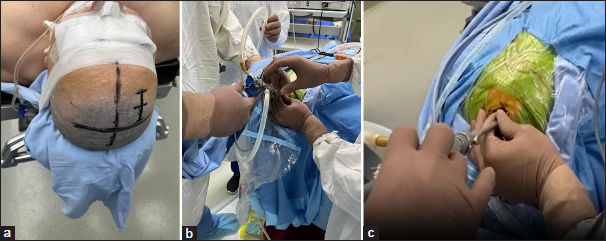
The working sheath, the trocar, and the 0°, 45°angled endoscope with a working channel diameter of 5.9 mm and a length of 130 mm were used. During the procedure, monopolar cautery, scissors, and forceps were utilized through the working channel.
The patient was in the supine position. He underwent a right side burr-hole for the endoscopic transseptal approach: 2.5 cm off the midline and 2.5 cm anterior to the coronal suture (Kocher’s point) following the recommendation of Azab et al.[
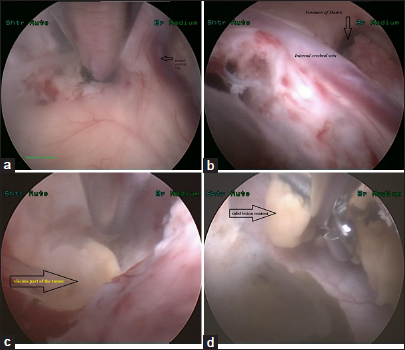
During removal, calcified areas were determined, which were crushed to the tube size for exploitation. At the inferior part of the lesion, semisolid gelatinous content compatible with the usual CC was seen and evacuated. The tumor was removed, and a capsule was left behind. The main reason for not dissecting a very thin cyst wall was the risk of bleeding and damage to the underlying structures, such as the pericallosal artery, fornix, and thalamus, which were tightly fused to the cyst capsule.[
Figure 3:
The endoscopic view during the resection of the colloid cyst (CC). (a) The cerebrotomy was performed between the internal cerebral vein (black arrow) and the septum pellucidum. Below is the forniceal column of the brain. (b) Narrowing and lateralization of the foramen of Monro (vertical black arrow) due to the large volume of the CC. (c) Opening the cyst capsule and aspiration of the viscous part of the CC (black arrow). (d) Solid cyst contents were removed with grasping forceps (black arrow).
Several challenges were met during the operation. First, mechanical fragmentation of the calcified portion of the tumor was difficult due to its high density. Second, regulating the Ringer’s Lactate temperature was challenging during the operation since the endoscopic devices require continuous fluid use. Finally, using several surgical instruments simultaneously was not possible through a monoportal endoscope during surgery.
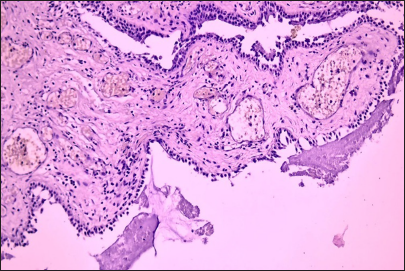
Histology
In the studied histological preparations, stained with hematoxylin and eosin, a cystic formation was examined, the wall of which is represented by fibrous tissue lined with one layer of columnar epithelium. Epithelial cells in the cytoplasm contained single mucin-containing vacuoles. There were structureless homogeneous eosinophilic masses in the cavity of the cyst. There was fibrosis, full-blooded vessels, and scattered lymphohistiocytic infiltration in the wall of the cyst [
Postoperation period
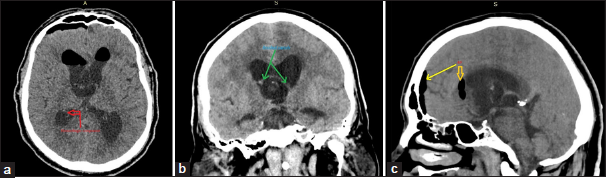
The patient’s condition was stable after surgery. Control computer tomography (CT) imaging was performed 24 h after the operation. The lateral ventricles were dilated with subependymal edema; air was detected in the anterior horns and subarachnoid space of the frontal region on the right [
Figure 5:
The brain computer tomography (CT) taken 24 h after the operation. (a) CT Axial. (b) CT coronal. (c) CT sagittal. (a) The red arrow shows a hemorrhage component of the posterior corn of the lateral ventricle. (b) The green arrows illustrate a residual capsule.(c) The yellow arrows shows the air in the anterior horns of the lateral ventricle and subarachnoid space of the frontal region.
No complications were observed in the postoperative period. Symptoms such as dizziness, headache, and nausea were regressed directly 24 h after the operation. Moreover, the follow-up examination conducted 3 months after the operation detected that urinary incontinence appeared rarely, and vision was improved compared to the preoperative period. The surgical incision was considerably short, comprising two cm; for this reason, the skin in the area of the surgical incision recovered fast. The overall hospital duration period was composed of 3 days.
Brain MRI imaging was performed about 3 months after the operation [
DISCUSSION
CCs are benign tumors considered developmental malformations. They are composed of an outer fibrous layer and an inner epithelium of ciliated or mucin-producing cells.[
Our case was a 57-year-old male who presented with dizziness, headache, nausea, a couple of episodes of urinary incontinence and short-term forgetfulness, gait ataxia, cognitive decline, and vision blurring. He had a giant cyst (30 × 31 × 35mm), which was resected through an endoscopic approach. Inside the lesion was a firm, hardly suctionable, solid gray-yellow material, which is not common for a CC. Semisolid bright gelatinous content was seen and evacuated at the central part of the lesion.
The giant size and exceptional location of the CCs are signs of an extremely rare type of CC. According to our review, there have been only two published studies of CCs located in the septum pellucidum, which were removed endoscopically,[
Beaumont et al. determined the risk factors associated with the symptomatic CC and the development of cyst-related hydrocephalus.[
An endoscopic third ventriculostomy was performed as the hydrocephalus treatment and its recurrence in our case, and after the mass wall opening, the CC was removed endoscopically. According to Samadian et al., attentive supervision is advised for CC with small size (<10 mm) and asymptomatic clinical characteristics; the endoscopic removal is recommended for moderate-size (10–20 mm) CCs with ventriculomegaly, T2 bright signal on MRI, and intraforaminal location.[
Sayehmiri et al. conducted a systematic review to compare the surgical outcomes after the microsurgical versus endoscopic removal of the CC located in the third ventricle.[
It is important to mention the presence of a new surgical tool, an ultrasound aspirator, which allows the forced aspiration of the cyst contents. Ibanez-Botella et al. carried out a retrospective descriptive study, which illustrated the surgical outcomes of 11 patients who had the endoscopic resection of the CC of the third ventricle with an ultrasonic aspirator.[
CONCLUSION
Overall, endoscopic removal may have positive and safe outcomes as the surgical treatment method of the giant CCs located in the septum pellucidum. We recommend that neurosurgeons demonstrate their illustrative cases related to the giant CCs located in the septum pellucidum, as the number of these studies is very limited. Further, a systematic analysis of these case studies is suggested to evaluate the effectiveness of the endoscopic removal of the giant CCs located in the septum pellucidum.
Ethical approval:
The Institutional Review Board approval is not required.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship:
Nil.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgments:
We are thankful to the patient for his cooperation and for allowing us to use his medical records in our case report.
References
1. Arjipour M, Gharib M, Eftekharian M. Endoscopic resection of a giant colloid cyst in the velum interpositum: Illustrative case. J Neurosurg Case Lessons. 2023. 5: CASE22381
2. Azab WA, Najibullah M, Yosef W. Endoscopic colloid cyst excision: Surgical techniques and nuances. Acta Neurochir (Wien). 2017. 159: 1053-8
3. Beaumont TL, Limbrick DD, Patel B, Chicoine MR, Rich KM, Dacey RG. Surgical management of colloid cysts of the third ventricle: A single-institution comparison of endoscopic and microsurgical resection. J Neurosurg. 2022. 137: 905-13
4. Beaumont TL, Limbrick DD, Rich KM, Wippold FJ 2nd, Dacey RG. Natural history of colloid cysts of the third ventricle. J Neurosurg. 2016. 125: 1420-30
5. Ibáñez-Botella G, Narváez IF, Pugliese B, Ros B, Arráez MA. Endoscopic resection of third ventricle colloid cysts using an ultrasonic aspirator. Neurosurg Rev. 2024. 47: 117
6. Murali SH, Parapati VR, Kesavapisharady K, Divakar G, Nair P, Venkat EH. Colloid cyst: Revision of third ventricular zones for risk stratification of hydrocephalus. World Neurosurg. 2024. 182: e276-83
7. Pryce ML, Huo CW, Dawes BH, Chung KH. Giant colloid cyst occupying a cavum septum pellucidum et vergae. J Clin Neurosci. 2020. 80: 238-41
8. Sabanci PA, Aras Y, Ali A, Unal TC, Dolen D, Sencer S. Transcortical removal of third ventricular colloid cysts: Comparison of conventional, guided microsurgical and endoscopic approaches and review of the literature. Turk Neurosurg. 2017. 27: 546-57
9. Samadian M, Ebrahimzadeh K, Maloumeh EN, Jafari A, Sharifi G, Shiravand S. Colloid cyst of the third ventricle: Long-term results of endoscopic management in a series of 112 cases. World Neurosurg. 2018. 111: e440-8
10. Sayehmiri F, Starke RM, Eichberg DG, Ghanikolahloo M, Rahmatian A, Fathi M. Comparison of microscopic and endoscopic resection of third-ventricular colloid cysts: A systematic review and meta-analysis. Clin Neurol Neurosurg. 2022. 215: 107179
11. Sarwar M. The septum pellucidum: Normal and abnormal. AJNR Am J Neuroradiol. 1989. 10: 989-1005
12. Sheikh AB, Mendelson ZS, Liu JK. Endoscopic versus microsurgical resection of colloid cysts: A systematic review and meta-analysis of 1,278 patients. World Neurosurg. 2014. 82: 1187-97
13. Siala S, Homen D, Smith B, Guimaraes C. Imaging of the septum pellucidum: Normal, variants and pathology. Br J Radiol. 2023. 96: 20221058
14. Souweidane MM, Hoffman CE, Schwartz TH. Transcavum interforniceal endoscopic surgery of the third ventricle. J Neurosurg Pediatr. 2008. 2: 231-6
15. Tubbs RS, Krishnamurthy S, Verma K, Shoja MM, Loukas M, Mortazavi MM. Cavum velum interpositum, cavum septum pellucidum, and cavum vergae: A review. Childs Nerv Syst. 2011. 27: 1927-30
16. Vialogo JG. Endoscopic transepto-interforniceal approach to colloid cysts: Case report. Arq Neuropsiquiatr. 2000. 58: 939-46
17. Winn HR. Youmans and winn neurological surgery. 7th ed., Vol. 2., Ch. 153. Amsterdam: Elsevier Health Sciences; 2016. p. 1207