- Department of Neurosurgery, Toyama University, Toyama, Japan
- Department of Neurosurgery, University of Toyama, Toyama, Japan.
Correspondence Address:
Emiko Hori, Department of Neurosurgery, Toyama University, Toyama, Japan.
DOI:10.25259/SNI_1026_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Emiko Hori1, Takuya Akai1, Keitaro Shiraishi1, Kunitaka Maruyama1, Satoshi Kuroda2. Endoscopic third ventriculostomy for patients with Blake’s pouch cyst with adult-onset hydrocephalus: Importance of improved cerebrospinal fluid flow in the prepontine cistern – A case report. 28-Apr-2023;14:155
How to cite this URL: Emiko Hori1, Takuya Akai1, Keitaro Shiraishi1, Kunitaka Maruyama1, Satoshi Kuroda2. Endoscopic third ventriculostomy for patients with Blake’s pouch cyst with adult-onset hydrocephalus: Importance of improved cerebrospinal fluid flow in the prepontine cistern – A case report. 28-Apr-2023;14:155. Available from: https://surgicalneurologyint.com/surgicalint-articles/12296/
Abstract
Background: Blake’s pouch cyst (BPC) is a posterior fossa cystic malformation that commonly occurs in children with rare adult onset. Herein, we report a case of adult onsets BPC.
Case Description: A 61-year-old man presented with gait and cognitive disturbance. Preoperative magnetic resonance imaging (MRI) revealed scarring in the prepontine cistern, and cine phase-contrast MRI revealed no pulsation. Endoscopic third ventriculostomy (ETV) was performed with opening the scarring in the prepontine cistern. Postoperative cine phase-contrast MRI revealed that cerebrospinal fluid (CSF) flow in the prepontine cistern improved, resolving the patient’s symptoms.
Conclusion: We report a case of adult-onset BPC. The mechanism by which is becomes symptomatic is still unclear. We opened the scar in prepontine cistern in addition to ETV with good results. In this report, we discussed the importance of the improvement in CSF dynamics in the prepontine cistern.
Keywords: Adult-onset, Blake’s pouch cyst, Endoscopic third ventriculostomy, Hydrocephalus, Prepontine cistern
INTRODUCTION
Blake’s pouch cyst (BPC) is a cystic malformation of the posterior fossa that is characterized by the ballooning of the superior velum into the cisterna magna. BPC is often associated with hydrocephalus and commonly occurs in children but rarely in adults even if it is a congenital anomaly like a longstanding overt ventriculomegaly in adults. Herein, we report a case of BPC in a patient with adult-onset hydrocephalus who achieved good outcomes after the opening of prepontine scarring as well as endoscopic third ventriculostomy (ETV).
CASE REPORT
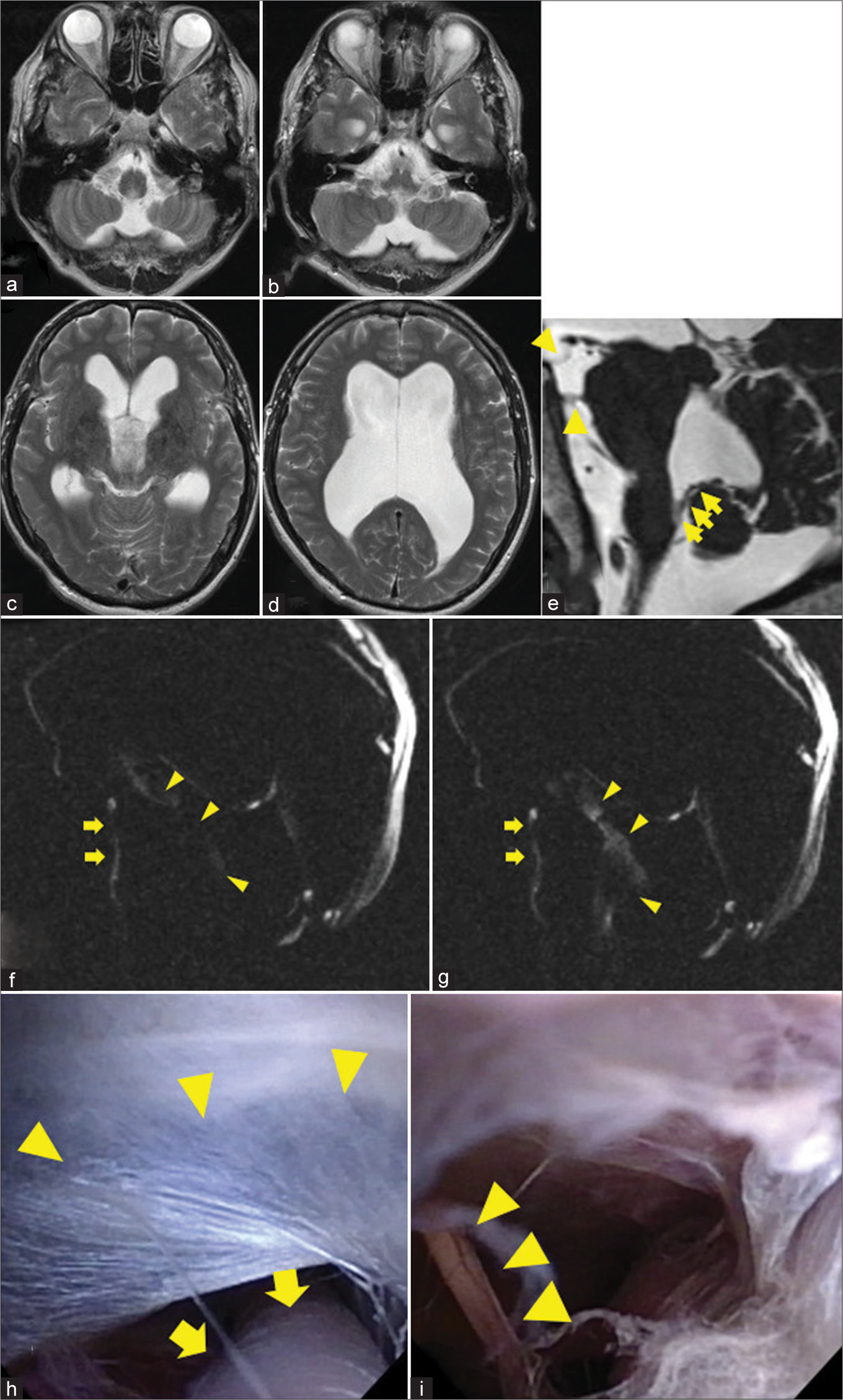
A 61-year-old man presented with gait disturbance that worsened over 2 weeks and memory disturbance since 6 months. He had a wide-based and slow gait. His score on the timed up and go test (TUG) was 14.5 s and 20 steps and that on the mini-mental state examination (MMSE) was 21. Computed tomography revealed ventriculomegaly (Evans index 0.45), and magnetic resonance imaging (MRI) revealed a cystic formation at the caudal side of the cerebellum, leading to a diagnosis of BPC [
Figure 1:
(a-d) Magnetic resonance image (MRI) showing an enlarged ventricle and cystic formation at the caudal side of the cerebellum. (e) The choroid plexus extends into the cyst compatible diagnosed as Blake’s pouch cyst (arrow). Sagittal MRI showing a downward bulging third ventricle floor and membrane like structure within the prepontine cistern (arrowheads). (f and g) Cine phase-contrast MRI revealing a normal bidirectional flow at the level of the aqueduct canal (arrowhead) but not at the prepontine cistern (arrow). (h and i) Intraoperative findings. (h) Scarring in the prepontine cistern (arrowheads) and basilar artery (arrows). (i) After opening the scar, abducens nerve (arrowheads).
We performed ETV using a flexible neuroendoscope (Olympus VEF type V®; Olympus, Tokyo, Japan). The third ventricle floor was opened with a perforating forceps and widened with a Expansor® Balloon catheter SI (Fuji Systems Corporation, Tokyo, Japan). Basilar artery and the scarring in the prepontine cistern were observed through the stoma. After perforation of the prepotine scarring, we confirmed cerebrospinal fluid (CSF) flow between the third ventricle and prepontine cistern. We also opened the scarring with perforating forceps under the critical observation of a flexible neuroendoscope [
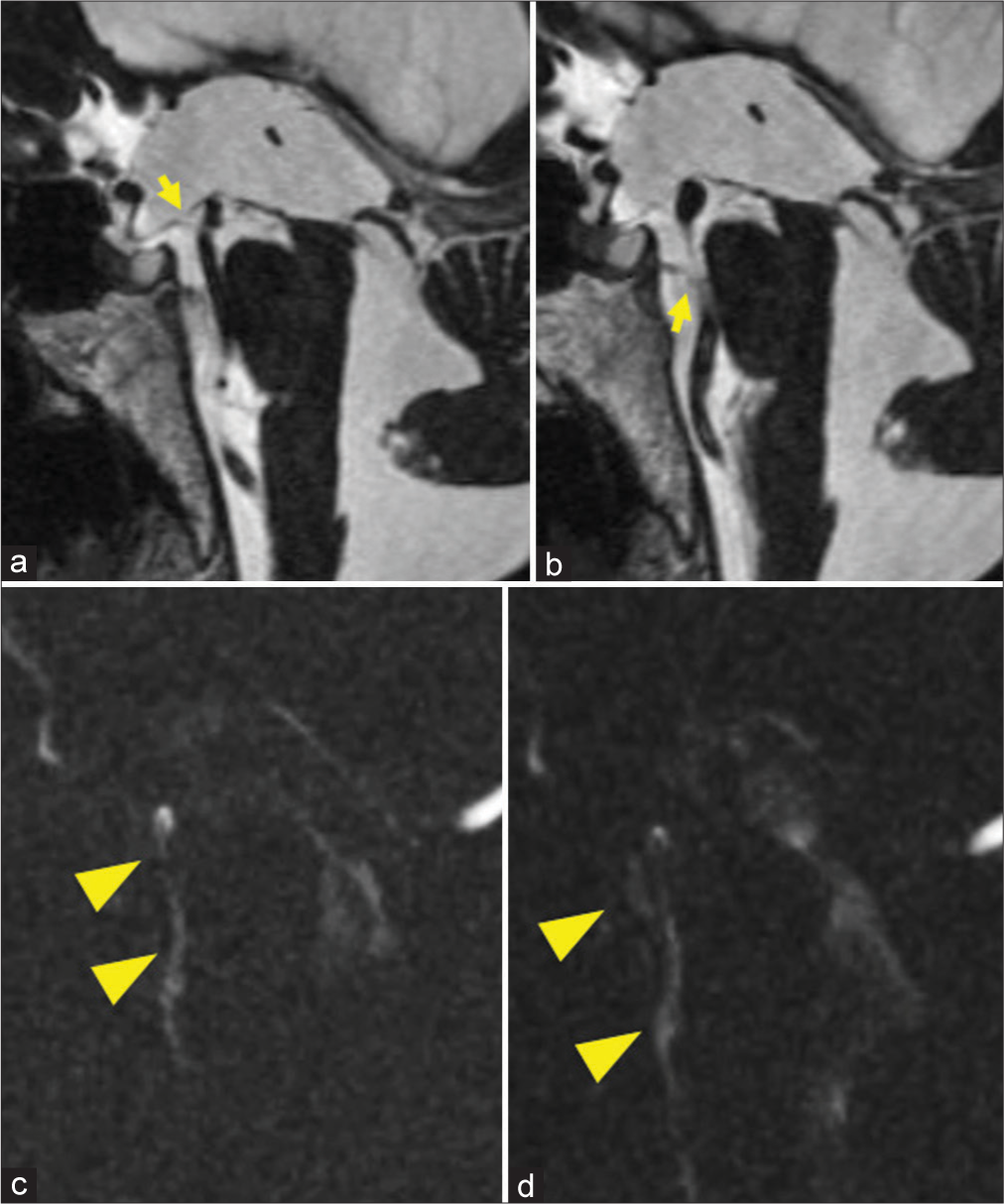
Postoperative MRI indicated the opening of the floor of third ventricle and scar in the prepontine cistern. Cine phase-contrast MRI revealed CSF flow in the prepontine cistern [
Figure 2:
(a and b) Postoperative magnetic resonance imaging (MRI): (a) The opening of the floor of third ventricle is observed (arrow). (b) The opening of the scarring in the prepontine cistern also observed (arrow). (c and d) Cine phase-contrast MRI indicating the cerebrospinal fluid flow in the prepontine cistern (arrowheads).
DISCUSSION
Dandy–Walker cyst and BPC are both congenital anomalies that originate from the rhombencephalon tegmentum. Cerebellar vermis is formed in patients with BPC but not in those with Dandy–Walker cysts.
BPC has been considered to result from a failure of regression of Blake’s pouch (the rudimental fourth ventricular tela choroidea). BPC is defined as a cystic dilatation of Blake’s pouch, which is left and dilated in the preliminary step of opening of foramen Magendie. The opening of the foramen Magendie is absent or incomplete, and the CSF flow at the outlet of the fourth ventricle may be impaired. In such a case, there are cases of shown dilatation of the ventricle and presenting symptoms.
BPC can be asymptomatic or can have clinical symptoms including headache or hydrocephalus. Blake’s pouch is treated using a ventriculoperitoneal shunt; however, many studies have reported the increasing use of ETV, because ETV could avoid the risks related with shunt placement such as isolated fourth ventricle, over drainage, and infection.[
The scarring in the prepontine cistern is a risk factor for failure of ETV[
The importance of improving CSF in the prepontine cistern has been recently demonstrated. CSF pulsation is crucial for CSF circulation, and one of the most prominent areas of pulsation is the prepontine cistern.[
Although BPC involves embryonic dysplasia, it can turn symptomatic in some adult patients. In this case, the scar in prepontine cistern was observed. It is possible that the formation of scar disturbed the CSF flow and pulsation, and stagnation of CSF caused hydrocephalus. Improvement of CSF flow in prepontine cistern is essential to achieve good outcomes.
CONCLUSION
BPC rarely occurs in adults. ETV is performed in symptomatic patients aged >60 years. In this case, we opened the scar in prepontine cistern in addition to ETV. CSF circulation in the prepontine cistern could be improved, which might result in good outcomes. Elderly patients with BPC can be symptomatic, and the opening the scar in the prepontine cistern is important for their treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
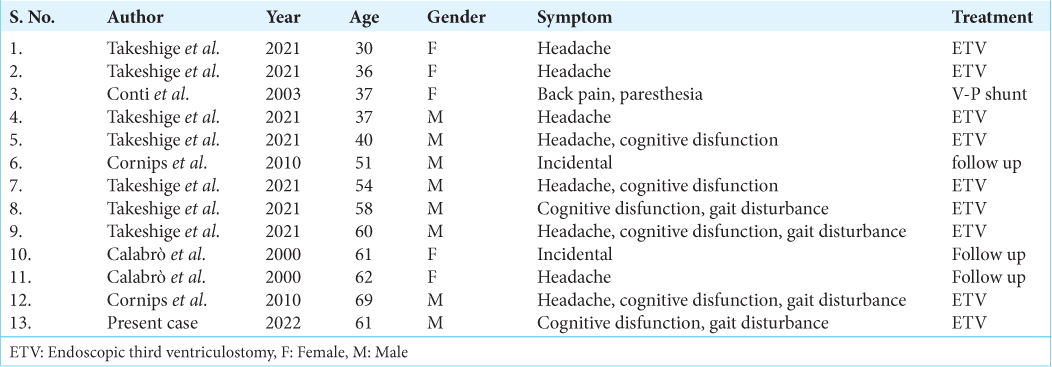
References
1. Anik I, Etus V, Anik Y, Ceylan S. Role of interpeduncular and prepontine cistern cerebrospinal fluid flow measurements in prediction of endoscopic third ventriculostomy success in pediatric triventricular hydrocephalus. Pediatr Neurosurg. 2010. 46: 344-50
2. Brusius CV, Cavalheiro S. Endoscopic third ventriculostomy is a safe and effective procedure for the treatment of Blake’s pouch cyst. Arq Neuropsiquiatr. 2013. 71: 545-8
3. Calabrò F, Arcuri T, Jinkins JR. Blake’s pouch cyst: An entity within the Dandy-Walker continuum. Neuroradiology. 2000. 42: 290-5
4. Chamiraju P, Bhatia S, Sandberg DI, Ragheb J. Endoscopic third ventriculostomy and choroid plexus cauterization in posthemorrhagic hydrocephalus of prematurity. J Neurosurg Pediatr. 2014. 13: 433-9
5. Conti C, Lunardi P, Bozzao A, Liccardo G, Fraioli B. Syringomyelia associated with hydrocephalus and Blake’s pouch cyst: Case report. Spine (Phila Pa 1976). 2003. 28: E279-83
6. Cornips EM, Overvliet GM, Weber JW, Postma AA, Hoeberigs CM, Baldewijns MM. The clinical spectrum of Blake’s pouch cyst: Report of six illustrative cases. Childs Nerv Syst. 2010. 26: 1057-64
7. Hirono S, Ito D, Murai H, Kobayashi M, Suyama M, Fujii K. Postnatal development of Blake’s pouch cyst: A case report and new insight for its pathogenesis. Childs Nerv Syst. 2014. 30: 1767-71
8. Nowosławska E, Gwizdała D, Barańska D, Grzelak P, Podgórski M, Zakrzewski K. The oscillatory flow of the cerebrospinal fluid in the Sylvian aqueduct and the prepontine cistern measured with phase contrast MRI in children with hydrocephalus-a preliminary report. Childs Nerv Syst. 2018. 34: 845-51
9. Takeshige N, Uchikado H, Yoshitake H, Negoto T, Yoshitomi M, Sakata K. Long-term outcomes of endoscopic third ventriculostomy for Blake’s pouch cyst in adults. Clin Neurol Neurosurg. 2021. 200: 106357
10. Takeuchi Y, Kimiwada T, Shirane R, Tominaga T. Progressive hydrocephalus after endoscopic third ventriculostomy in pediatric patients with Blake’s pouch cyst. NMC Case Rep J. 2020. 7: 141-5
11. Uche EO, Okorie C, Iloabachie I, Amuta DS, Uche NJ. Endoscopic third ventriculostomy (ETV) and ventriculoperitoneal shunt (VPS) in non-communicating hydrocephalus (NCH): Comparison of outcome profiles in Nigerian children. Childs Nerv Syst. 2018. 34: 1683-9
12. Wang S, Stone S, Weil AG, Fallah A, Warf BC, Ragheb J. Comparative effectiveness of flexible versus rigid neuroendoscopy for endoscopic third ventriculostomy and choroid plexus cauterization: A propensity score-matched cohort and survival analysis. J Neurosurg Pediatr. 2017. 19: 585-91
13. Warf BC, Kulkarni AV. Intraoperative assessment of cerebral aqueduct patency and cisternal scarring: Impact on success of endoscopic third ventriculostomy in 403 African children. J Neurosurg Pediatr. 2010. 5: 204-9
14. Yamada S, Kelly E. Cerebrospinal fluid dynamics and the pathophysiology of hydrocephalus: New concepts. Semin Ultrasound CT MR. 2016. 37: 84-91
15. Yamada S, Miyazaki M, Kanazawa H, Higashi M, Morohoshi Y, Bluml S. Visualization of cerebrospinal fluid movement with spin labeling at MR imaging: Preliminary results in normal and pathophysiologic conditions. Radiology. 2008. 249: 644-52
16. Yamada S. Cerebrospinal fluid physiology: Visualization of cerebrospinal fluid dynamics using the magnetic resonance imaging Time-Spatial Inversion Pulse method. Croat Med J. 2014. 55: 337-46