- Department of Neurosurgery, Faculty of Human Medicine, Zagazig University, Zagazig, Egypt.
Correspondence Address:
Mohamed Salah, Department of Neurosurgery, Zagazig University, Zagazig, Egypt.
DOI:10.25259/SNI_971_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohamed Salah, Ahmed Yahia Elhuseny, Essam M. Youssef. Endoscopic third ventriculostomy for the management of hydrocephalus secondary to posterior fossa tumors: A retrospective study. 25-Feb-2022;13:65
How to cite this URL: Mohamed Salah, Ahmed Yahia Elhuseny, Essam M. Youssef. Endoscopic third ventriculostomy for the management of hydrocephalus secondary to posterior fossa tumors: A retrospective study. 25-Feb-2022;13:65. Available from: https://surgicalneurologyint.com/surgicalint-articles/11416/
Abstract
Background: Endoscopic third ventriculostomy (ETV) is an effective alternative to ventriculoperitoneal shunting as well as external ventricular drainage for the urgent management of acute hydrocephalus. We performed this study to investigate the efficacy and safety of ETV before tumor resection in managing hydrocephalus in patients with posterior fossa brain tumors (PFBT) in our neurosurgery department.
Methods: We conducted this retrospective observational study between February 2018 and February 2020 on all cases diagnosed with PFBT associated with triventricular obstructive hydrocephalus. We retrospectively reviewed the demographic characteristics, operative procedures, and radiological investigations of all cases. During the follow-up period, clinical, as well as radiological success were evaluated.
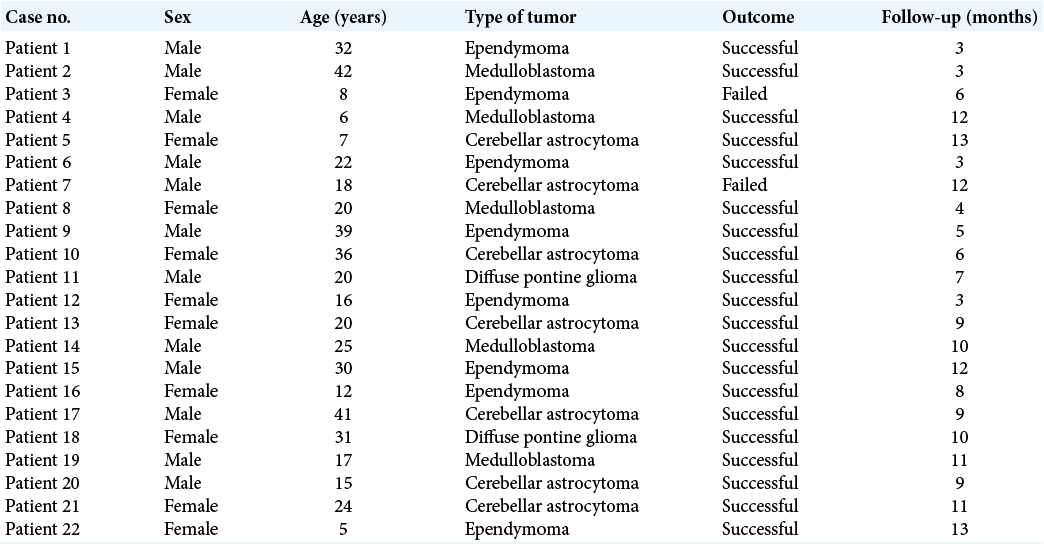
Results: Twenty-two ETV procedures were performed in 22 cases of PFBT (mean age = 22.1 years, SD = 11.4). Of the 22 cases, 8 cases (36.4%) had ependymoma, 7 cases (31.8%) had cerebellar astrocytoma, and 5 cases (22.7 %) had medulloblastoma, while 2 cases (9.1%) had diffuse pontine gliomas. The median follow-up duration was 9 months (range 3–13 months). The most commonly reported clinical presentation was the significant intracranial pressure increase. All operations were performed successfully in all cases. Only two ETV post-tumor resection failures were documented during the follow-up period.
Conclusion: Preoperative ETV has shown to be an effective long-term cerebrospinal fluid diversion procedure to manage PFBT-associated hydrocephalus, with a relatively low rate of complications. Further prospective studies are required to assess the regular use of ETV before complete tumor resection.
Keywords: Brain, Endoscopic third ventriculostomy, Posterior fossa, Resection, Tumors
INTRODUCTION
One of the most prevalent neurosurgical pathologies requiring neurosurgical intervention is hydrocephalus. Managing hydrocephalus secondary to central nervous system tumors is a complicated, challenging neurosurgical issue.[
Endoscopic third ventriculostomy (ETV) was first identified as a treatment option for hydrocephalus by William Mixter in 1923.[
There is a paucity of data regarding the incidence of perioperative complications as well as permanent hydrocephalus in patients who underwent ETV procedures before PFBT surgeries. We performed this study to investigate the efficacy and safety of ETV before tumor resection in managing hydrocephalus in patients with PFBT.
MATERIALS AND METHODS
The “Strengthening the Reporting of Observational Studies in Epidemiology” statement guidelines were followed while reporting this study.[
Eligibility criteria
We included all cases diagnosed to have PFBT with associated triventricular obstructive hydrocephalus. Cases experiencing active stage either of ventriculitis or meningitis, intraventricular hemorrhage, or patients who did not accept the ETV treatment were excluded from our study.
Case definition
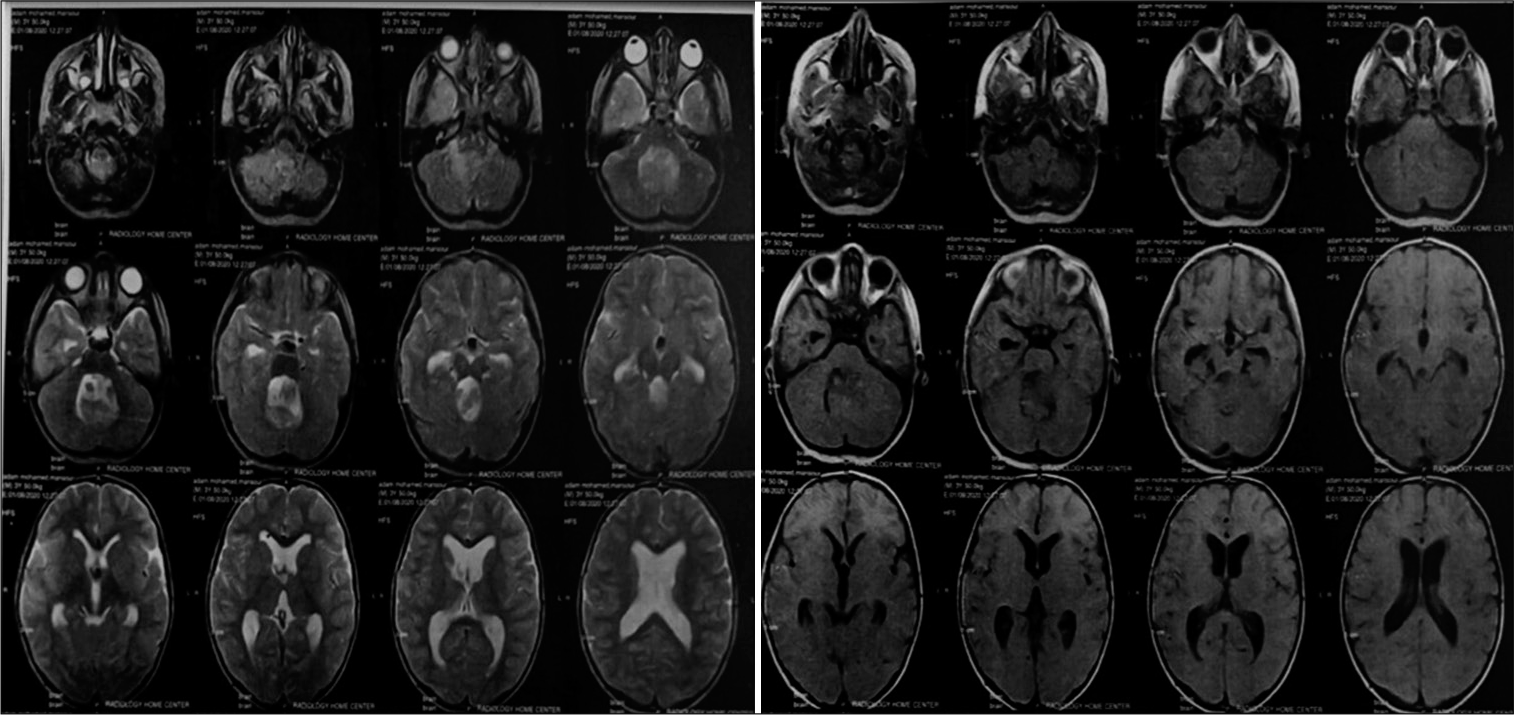
Patients were diagnosed to have symptomatic hydrocephalus if they had a clinical presentation of increased intracranial pressure (ICP) (i.e., headache, impaired consciousness, nausea, or vomiting) and the magnetic resonance imaging showed enlarged ventricles as well as the obstruction of the fourth ventricle [
Procedures
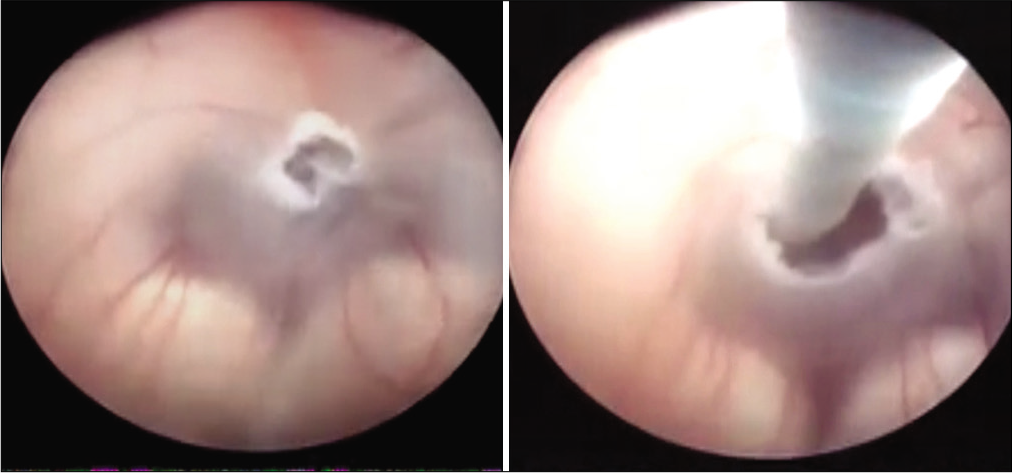
The previous literature has extensively described the ETV procedures’ technique.[
Clinical and radiological assessment
During the follow-up period, clinical success was characterized as the absence of hydrocephalus clinical presentations during the study’s follow-up duration. The continuation or deterioration of hydrocephalus-related clinical manifestations necessitating shunt insertion and the postoperative complications were the characterizations of ETV failure. We assessed the radiological success 72 h after surgery, with the absence of the leakage of CSF; it was considered when the preoperative imaging features of hydrocephalus were improved as well as the features of elevated ICP.
Data analysis
The dichotomous data were expressed as frequencies and percentages, while the continuous data were presented as mean and standard deviation or the median and range in case of normally and non-normally distributed data, respectively. All analyses were carried out using the Microsoft® Excel software version 2019.
RESULTS
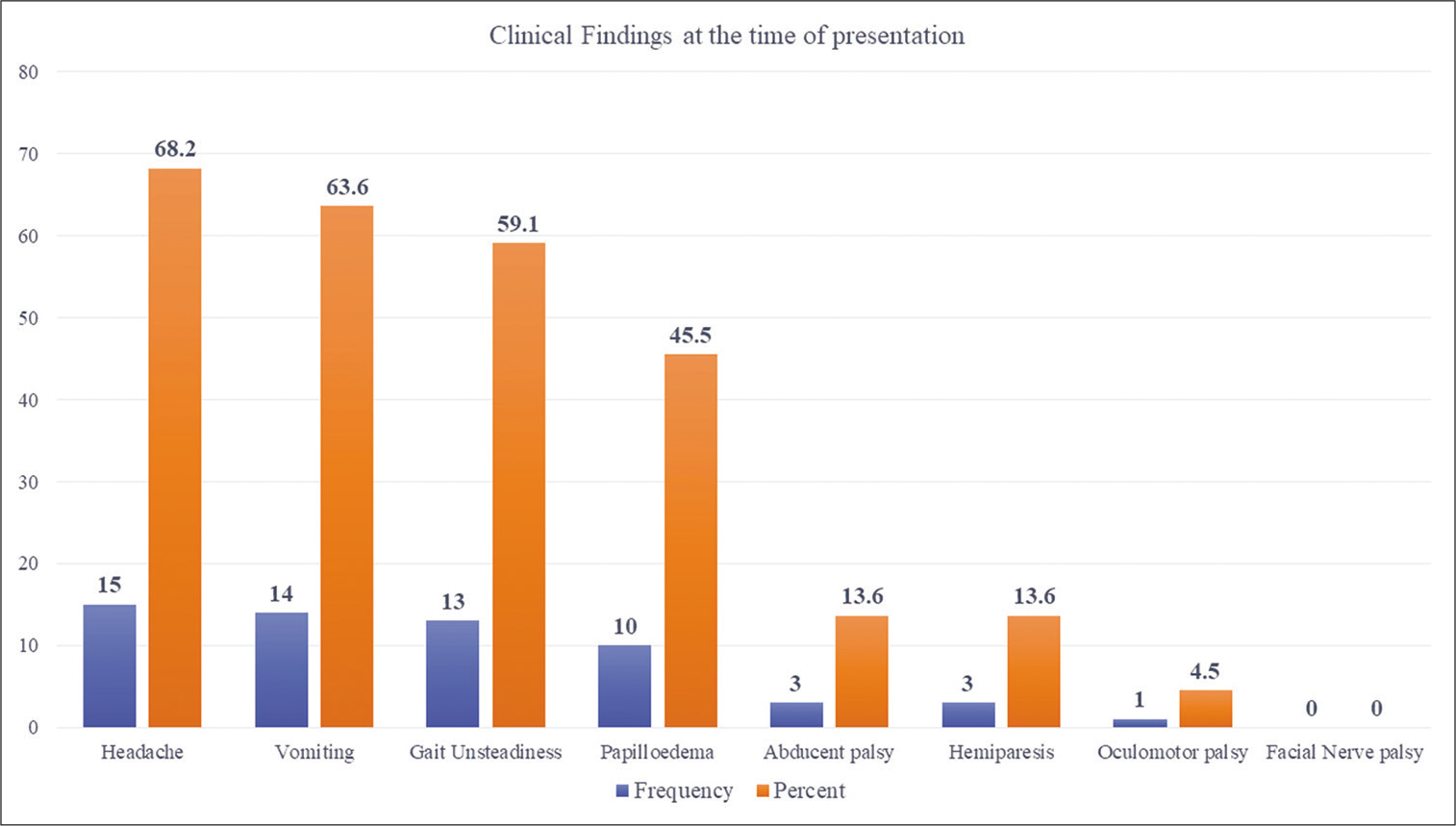
We performed 22 ETV procedures in 22 cases (12 males and 10 females). The patients’ age ranged between 5 and 42 years old (mean age = 22.1 years, SD = 11.4). The most common types of PFBT were ependymoma noted in 8 cases (36.4%) followed by cerebellar astrocytoma in 7 cases (31.8%) and medulloblastoma noted in 5 cases (22.7 %). Diffuse pontine glioma was reported in only 2 cases (9.1%). The follow-up duration ranged between 3 and 13 months (median follow-up = 9 months, IQR = 6.50). In the studied cases, the most commonly reported clinical presentation was the significant ICP increase in the form of headaches and vomiting followed by gait unsteadiness and papilledema [
There were no mechanical difficulties reported during the fenestration of the third ventricle’s floor; all operations were performed successfully in all cases. ETV was effective in relieving hydrocephalus. No ETV failures were observed before surgical excision of the PFBT; all patients exhibited significant clinical improvement as well as the radiological absence of ventriculomegaly. During the follow-up phase, two ETV post-tumor resection failures were documented. The ETV outcome, as well as the follow-up periods of the included patients, is detailed in [
DISCUSSION
There is no agreement about how to manage adult patients with PFBT-associated obstructive hydrocephalus surgically. The previous literature stated that, at the time of presentation, most patients with PFBT experience hydrocephalus; the management of such cases is still debatable. Previously, the VP shunt placement was an effective preoperative management in cases with PFBT-related hydrocephalus. However, as neurosurgeons became more conscious of the frequent ventricular shunting-associated complications, as well as the less frequent complications such as upward herniation, tumor bleeding, and intracranial tumor seedling inside the peritoneum, they began to inquire about the routine ventricular shunting.[
Summary of the main findings
In our study, 22 ETV procedures were performed in 22 cases. The age ranged between 5 and 42 years old, with a mean age of 22.1 years, and the follow-up duration ranged between 3 and 13 months, with a median of 9 months. Regarding the distribution of PFBT among the studied population, 36.4% had ependymoma, 31.8% had cerebellar astrocytoma, 22.7% had medulloblastoma, and 9.1% had diffuse pontine glioma.
All operations were performed successfully in all cases, with no serious intraoperative complications. In our study, ETV relieved hydrocephalus effectively before the surgical excision of the PFBT. All cases showed considerable clinical and radiological improvements. During the follow-up period, only two ETV post-tumor resection failures were detected.
The first case was an 8-year-old girl with ependymoma who presented 6 months after tumor resection with symptoms of high ICP. The CT scan showed that there was obstructive hydrocephalus; despite a patent fourth ventricle. Moreover, we observed a nonenhancing mass in the left frontal lobe, with nearby perifocal edema, causing a considerable mass effect. A second ETV was performed for this patient; it exhibited a patent stoma of the floor of the third ventricle. The other case was an 18-year-old male patient with cerebellar astrocytoma who experienced CSF infection 5 days after tumor excision; this case was treated with EVD as well as antibiotics, then, a VP shunt was inserted.
Agreement and disagreement with the previous studies
In 2019, a retrospective analysis was conducted by Frisoli et al. on children with PFBT- associated hydrocephalus who underwent tumor resection. They showed that ETV before PFBT resection in the pediatric population decreased the postoperative VP shunt placement (16% of patients underwent ETV compared to 31% in the matched control group), with no complications reported during ETV.[
In 2018, a retrospective study was conducted on adult patients who underwent ETVs before PFBT surgery; of them, 82.5% had symptomatic hydrocephalous, and all of them reported clinical improvement after EVT, with no reported EVT-related complications.[
Furthermore, in Marx et al., the authors performed a 10-year period study between 2005 and 2014. They reported that the incidence rate of hydrocephalus before PFBT surgery in adults is lower than the rate reported in the previous literature in the pediatric population, and it is estimated to be 21.4%. Furthermore, they stated that the persistent hydrocephalus occurrence risk was low (5.7%) while it was 2.1% for the newly formed hydrocephalus following PFBT surgery, and not all adult patients require ETV before PFBT surgeries.[
In a previous single-center experience retrospective study conducted by Grand et al., the authors reported that the success rate of the total of 243 completed procedures was 72.8%. Of the intended ETV procedures, only nine complications were documented (3.6%); of these complications, only 5 complications (2%) were serious. The authors concluded that in selected patients, the use of ETV in adult hydrocephalus has a broad scope, with a low complication rate and relatively good efficacy.[
Significance of the findings
Before tumor resection, an EVD insertion is a viable CSF diversion management option that can be used in patients with PFBT and subsequent obstructive hydrocephalus. EVD increases the risk of CSF inflammation, hemorrhage, and upward herniation. As a result of these issues, a more conservative care protocol was introduced, which included preoperative steroids accompanied by tumor excision and, if necessary, the insertion of an EVD.[
The success rate of ETV is mainly dependent on the tumor’s localization as well as its growth pattern. Compared to benign lesions, progressive tumors are more prone to close ventriculostoma. Furthermore, the symptoms’ duration seems to be a predictor.[
Complete resection of PFBT should restore the normal CSF pathway. However, many children would develop uncontrolled persistent hydrocephalus after tumor resection because of the postoperative adhesions related to either the aqueduct or the outlets of the fourth ventricle.[
The main limitation of our study is the low number of included patients. Furthermore, being a single-institution observational study limits the generalization of our findings. We could not include a control group because of the retrospective design; thus, we recommend that further prospective clinical trials should compare different groups to assess the optimal CSF diversion procedure and to assess the long-term follow-up among such cases.
CONCLUSION
Preoperative ETV has been shown to be an effective long-term CSF diversion procedure to manage PFBT-associated hydrocephalus, with a relatively low rate of complications. To support these findings, further prospective studies are required to assess the regular use of ETV before complete tumor resection.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bhatia R, Tahir M, Chandler CL. The management of hydrocephalus in children with posterior fossa tumours: The role of pre-resectional endoscopic third ventriculostomy. Pediatr Neurosurg. 2009. 45: 186-91
2. Bouras T, Sgouros S. Complications of endoscopic third ventriculostomy: A systematic review. Acta Neurochir Suppl. 2012. 113: 149-53
3. Braksick SA, Himes BT, Snyder K, Van Gompel JJ, Fugate JE, Rabinstein AA. Ventriculostomy and risk of upward herniation in patients with obstructive hydrocephalus from posterior fossa mass lesions. Neurocrit Care. 2018. 28: 338-43
4. Due-Tonnessen BJ, Helseth E. Management of hydrocephalus in children with posterior fossa tumors: Role of tumor surgery. Pediatr Neurosurg. 2007. 43: 92-6
5. El Beltagy MA, Kamal HM, Taha H, Awad M, El Khateeb N. Endoscopic third ventriculostomy before tumor surgery in children with posterior fossa tumors, CCHE experience. Childs Nerv Syst. 2010. 26: 1699-704
6. El-Ghandour NM. Endoscopic third ventriculostomy versus ventriculoperitoneal shunt in the treatment of obstructive hydrocephalus due to posterior fossa tumors in children. Childs Nerv Syst. 2011. 27: 117-26
7. Farb R, Rovira A, Hodler J, Kubik-Huch RA, von Schulthess GK.editors. Hydrocephalus and CSF disorders. Diseases of the Brain, Head and Neck, Spine 2020-2023. Diagnostic Imaging. Cham, CH: IDKD Springer Series; 2020. p. 11-24
8. Foreman P, McClugage S, Naftel R, Griessenauer CJ, Ditty BJ, Agee BS. Validation and modification of a predictive model of postresection hydrocephalus in pediatric patients with posterior fossa tumors. J Neurosurg Pediatr. 2013. 12: 220-6
9. Frisoli F, Kakareka M, Cole KA, Waanders AJ, Storm PB, Lang SS. Endoscopic third ventriculostomy prior to resection of posterior fossa tumors in children. Childs Nerv Syst. 2019. 35: 789-94
10. Grand W, Leonardo J, Chamczuk AJ, Korus AJ. Endoscopic third ventriculostomy in 250 adults with hydrocephalus: Patient selection, outcomes, and complications. Neurosurgery. 2016. 78: 109-19
11. Grant JA, McLone DG. Third ventriculostomy: A review. Surg Neurol. 1997. 47: 210-2
12. Hong S, Hirokawa D, Usami K, Ogiwara H. The long-term outcomes of endoscopic third ventriculostomy in pediatric hydrocephalus, with an emphasis on future intellectual development and shunt dependency. J Neurosurg Pediatr. 2018. 23: 104-8
13. Hopf NJ, Grunert P, Fries G, Resch KD, Perneczky A. Endoscopic third ventriculostomy: Outcome analysis of 100 consecutive procedures. Neurosurgery. 1999. 44: 795-804
14. Jung TY, Chong S, Kim IY, Lee JY, Phi JH, Kim SK. Prevention of complications in endoscopic third ventriculostomy. J Korean Neurosurg Soc. 2017. 60: 282-8
15. Kulkarni AV, Drake JM, Kestle JR, Mallucci CL, Sgouros S, Constantini S. Endoscopic third ventriculostomy vs cerebrospinal fluid shunt in the treatment of hydrocephalus in children: A propensity score-adjusted analysis. Neurosurgery. 2010. 67: 588-93
16. Lee M, Wisoff JH, Abbott R, Freed D, Epstein FJ. Management of hydrocephalus in children with medulloblastoma: Prognostic factors for shunting. Pediatr Neurosurg. 1994. 20: 240-7
17. Limbrick DD, Baird LC, Klimo P, Riva-Cambrin J, Flannery AM. Pediatric Hydrocephalus Systematic R Evidence-Based Guidelines Task F Pediatric hydrocephalus: Systematic literature review and evidence-based guidelines Part. 4 Cerebrospinal fluid shunt or endoscopic third ventriculostomy for the treatment of hydrocephalus in children. J Neurosurg Pediatr. 2014. 14: 30-4
18. Lin CT, Riva-Cambrin JK. Management of posterior fossa tumors and hydrocephalus in children: A review. Childs Nerv Syst. 2015. 31: 1781-9
19. Marx S, El Damaty A, Manwaring J, El Refaee E, Fleck S, Fritsch M. Endoscopic third ventriculostomy before posterior fossa tumor surgery in adult patients. J Neurol Surg A Cent Eur Neurosurg. 2018. 79: 123-9
20. Marx S, Reinfelder M, Matthes M, Schroeder HW, Baldauf J. Frequency and treatment of hydrocephalus prior to and after posterior fossa tumor surgery in adult patients. Acta Neurochir (Wien). 2018. 160: 1063-71
21. Moorthy RK, Rajshekhar V. Endoscopic third ventriculostomy for hydrocephalus: A review of indications, outcomes, and complications. Neurol India. 2011. 59: 848-54
22. Oertel JM, Schroeder HW, Gaab MR. Third ventriculostomy for treatment of hydrocephalus: Results of 271 procedures. Neurosurg Q. 2006. 16: 24-31
23. Oliveira LM, Nitrini R, Roman GC. Normal-pressure hydrocephalus: A critical review. Dement Neuropsychol. 2019. 13: 133-43
24. Ray P, Jallo GI, Kim RY, Kim BS, Wilson S, Kothbauer K. Endoscopic third ventriculostomy for tumor-related hydrocephalus in a pediatric population. Neurosurg Focus. 2005. 19: E8
25. Ruggiero C, Cinalli G, Spennato P, Aliberti F, Cianciulli E, Trischitta V. Endoscopic third ventriculostomy in the treatment of hydrocephalus in posterior fossa tumors in children. Childs Nerv Syst. 2004. 20: 828-33
26. Sainte-Rose C, Cinalli G, Roux FE, Maixner R, Chumas PD, Mansour M. Management of hydrocephalus in pediatric patients with posterior fossa tumors: The role of endoscopic third ventriculostomy. J Neurosurg. 2001. 95: 791-7
27. Sherrod BA, Iyer RR, Kestle JR. Endoscopic third ventriculostomy for pediatric tumor-associated hydrocephalus. Neurosurg Focus. 2020. 48: E5
28. Texakalidis P, Tora MS, Wetzel JS, Chern JJ. Endoscopic third ventriculostomy versus shunt for pediatric hydrocephalus: A systematic literature review and meta-analysis. Childs Nerv Syst. 2019. 35: 1283-93
29. von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. J Clin Epidemiol. 2008. 61: 344-9
30. Vulcu S, Eickele L, Cinalli G, Wagner W, Oertel J. Long-term results of endoscopic third ventriculostomy: An outcome analysis. J Neurosurg. 2015. 123: 1456-62
31. Wong TT, Liang ML, Chen HH, Chang FC. Hydrocephalus with brain tumors in children. Childs Nerv Syst. 2011. 27: 1723-34