- Department of Neurosurgery, Yokohama City University Graduate School of Medical Sciences, Yokohama, Japan
Correspondence Address:
Yu Iida, Department of Neurosurgery, Yokohama City University Graduate School of Medical Sciences, Yokohama, Japan.
DOI:10.25259/SNI_772_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Masanori Isoda, Yu Iida, Taisuke Akimoto, Satoshi Hori, Jun Suenaga, Nobuyuki Shimizu, Yasunobu Nakai, Tetsuya Yamamoto. Endovascular treatment for posterior inferior cerebellar artery aneurysm with vertebral artery stenosis: The critical role of diagnosing osteophyte compression. 15-Nov-2024;15:421
How to cite this URL: Masanori Isoda, Yu Iida, Taisuke Akimoto, Satoshi Hori, Jun Suenaga, Nobuyuki Shimizu, Yasunobu Nakai, Tetsuya Yamamoto. Endovascular treatment for posterior inferior cerebellar artery aneurysm with vertebral artery stenosis: The critical role of diagnosing osteophyte compression. 15-Nov-2024;15:421. Available from: https://surgicalneurologyint.com/surgicalint-articles/13224/
Abstract
Background: Vertebral artery (VA) stenosis can be caused by several factors, including arteriosclerosis, arterial dissection, and mechanical compression. Symptomatic vertebrobasilar insufficiency caused by VA stenosis due to mechanical compression associated with head rotation is well-known as Bow Hunter’s syndrome. However, an accurate diagnosis of asymptomatic osteophyte compression-induced nonrotational VA stenosis is difficult. We report a case of left posterior inferior cerebellar artery aneurysm with severe left VA stenosis, treated with stent-assisted coil embolization following appropriate diagnosis.
Case Description: A 72-year-old female patient was found to have severe asymptomatic VA stenosis at the V2 segment (C4–5 level of the cervical spine) on cerebral angiography. Osteophyte compression-induced VA stenosis was suspected, which was confirmed by cone-beam computed tomography. The VA stenosis improved by flexing the neck and fixing the head position, following which the endovascular treatment was successfully completed.
Conclusion: The site of the VA stenosis is critical in determining the etiology. Atherosclerotic VA stenosis often occurs at the origin of the artery or V4 segment, whereas bony compression-induced stenosis is more likely to occur at the V2 segment. Diagnosis and appropriate management of VA stenosis is based on determining the site.
Keywords: Aneurysm, Bow-Hunter’s syndrome, Neuroendovascular, Osteophyte, Rheumatoid arthritis, Vertebral artery stenosis
INTRODUCTION
Vertebral artery (VA) stenosis can be caused by intrinsic wall disorders, such as atherosclerosis or dissection, as well as extrinsic factors, such as mechanical compression by osteophytes.[
CASE PRESENTATION
A 72-year-old female patient with a medical history of hypertension, cervical spondylosis, and rheumatoid arthritis (RA) was found to have a de novo PICA aneurysm during follow-up imaging of asymptomatic multiple cerebral aneurysms at another hospital. The aneurysm showed a tendency to enlarge over several months, and she was referred to our hospital for treatment. No significant neurological deficits were observed in the patient. Cerebral angiography from the referring hospital showed severe stenosis at the left V2 segment (C4–5 level of the cervical spine,
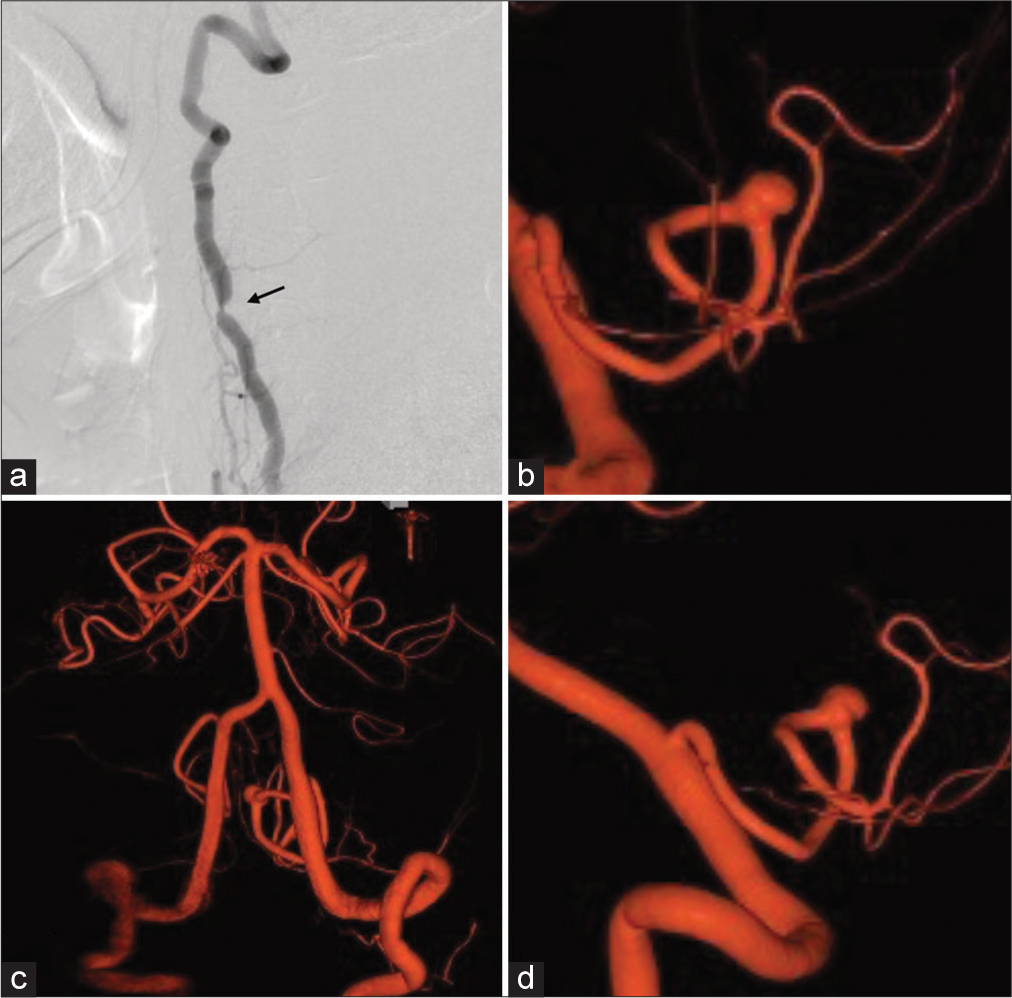
Figure 1:
Preoperative angiography findings. (a) Angiography of the left vertebral artery (VA) in the lateral projection (extracranial) shows severe stenosis at the C4–5 level (arrow). (b) The working angle three-dimensional view of the left VA shows an aneurysm at the cranial loop of the left posterior inferior cerebellar artery. (c) Angiography of the left VA in the anteroposterior projection (intracranial) shows a relatively steep angle of the VA union. (d) Angiography of the left VA in the lateral projection shows the left PICA branching cranially from the left VA.
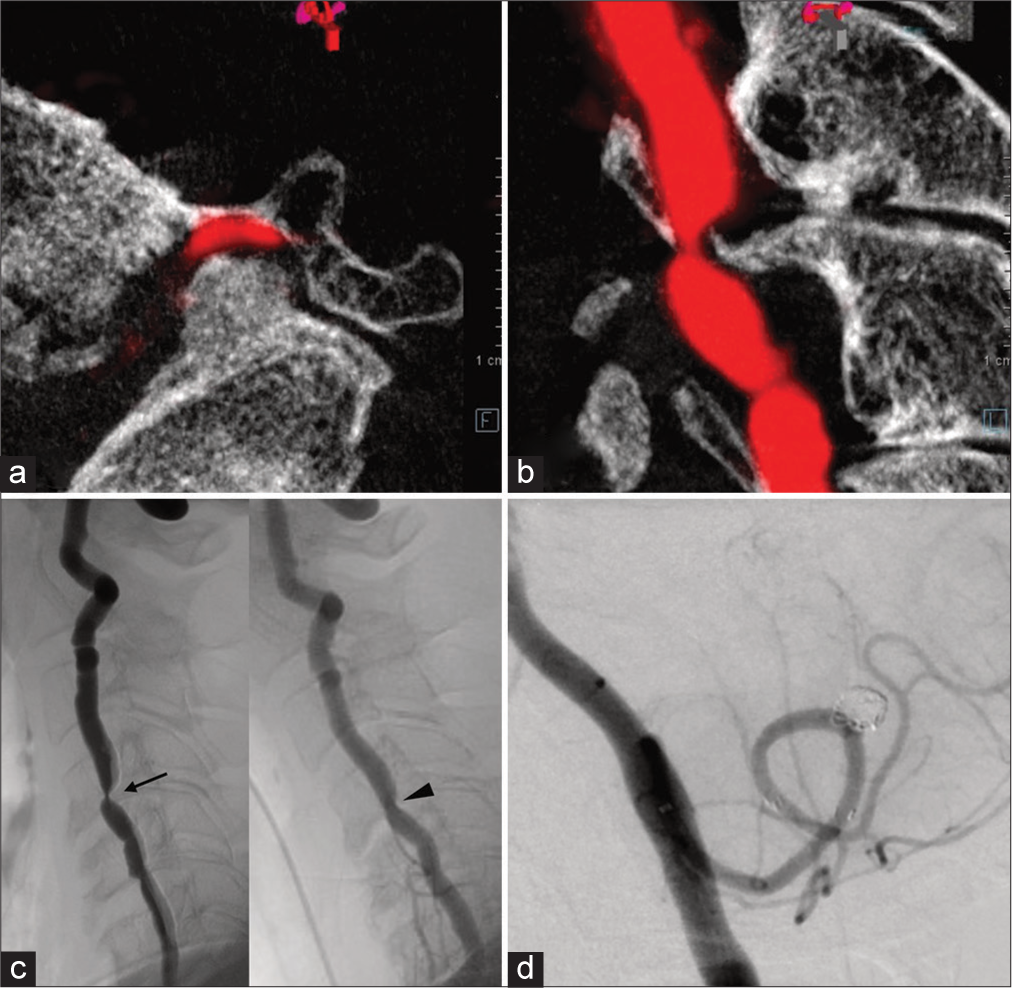
The endovascular procedure was performed under general anesthesia. The left distal radial artery was punctured from the anatomical snuff box, and a 5 Fr guiding sheath (5Fr. FUBUKI Dilator Kit 100 cm; Asahi, Aichi, Japan) was inserted and guided to the left V1 segment. VA angiography showed stenosis at the C4–5 level. Considering the atypical nature of atherosclerotic stenosis, we suspected compression by osteophytes and performed cone-beam computed tomography (CT). Cone-beam CT showed that the osteophyte at C4–5 was protruding ventrally and mechanically compressed the VA [
Figure 2:
Intraoperative computed tomography and angiography findings. (a) Sagittal and (b) axial cone-beam computed tomography images show osteophyte compression-induced left vertebral artery (VA) stenosis at the C4–5 level. (c) Angiography of the left VA with slight neck extension shows stenosis of the VA (left panel, arrow); however, the stenosis improves when the neck is flexed (right panel, arrowhead). (d) Postoperative angiography of the VA shows complete obliteration of the aneurysm.
The patient’s postoperative course was uneventful, and no new neurological symptoms developed. One week after treatment, the patient was discharged without complications. The aneurysm has not recurred for 3 months following the treatment.
DISCUSSION
BHS is caused by the mechanical compression of the VA during neck rotation, although there are few reports of VA stenosis occurring during neck extension.[
Misdiagnosing this case as VA stenosis due to arteriosclerosis and performing inappropriate interventions, such as percutaneous transluminal angioplasty or stent placement, could have increased the risk of balloon fragmentation or arterial dissection. Moreover, as the stenosis was caused by osteophyte compression, these procedures would not have resulted in improvement. In this case, the VA stenosis was located at C4–5, making atherosclerotic stenosis unlikely. Using cone-beam CT, we identified a relationship between the cervical bone and VA, leading to a diagnosis of osteophyte compression-induced VA stenosis. Correct diagnosis allowed us to alleviate the stenosis by flexing the head facilitating access through the left VA.
CONCLUSION
We performed stent-assisted coil embolization of a left PICA aneurysm associated with left VA stenosis. When VA stenosis is present, the cause could be inferred from the lesion level. If mechanical compression by osteophytes is identified as the cause, adjusting the position of the head can facilitate the smooth execution of endovascular treatment.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Cloud GC, Markus HS. Diagnosis and management of vertebral artery stenosis. QJM Int J Med. 2003. 96: 27-54
2. Correia PN, Meyer IA, Odier C. Intrinsic stenosing and occlusive pathologies of the vertebral artery: A narrative review. Neurochirurgie. 2024. 70: 101527
3. Curry BP, Ravindra VM, Boulter JH, Neal CJ, Ikeda DS. Bow hunter syndrome in rheumatoid arthritis: Illustrative case. J Neurosurg Case Lessons. 2021. 2: CASE21298
4. Eley N, Kumar R, Ryan R, Sethi R. Vertebrobasilar insufficiency syndrome in extension: Insights into surgical treatment. World Neurosurg. 2024. 183: 71-5
5. Ndongo Sonfack DJ, Bojanowski MW, Tarabay B, Gennari A, Shédid D, Yuh SJ. Vertebral artery stenosis from osteophyte: A systematic review and case series. Neurochirurgie. 2024. 70: 101525
6. Smith DR, Vanderark GD, Kempe LG. Cervical spondylosis causing vertebrobasilar insufficiency: A surgical treatment. J Neurol Neurosurg Psychiatry. 1971. 34: 388-92
7. Sorensen BF. Bow hunter’s stroke. Neurosurgery. 1978. 2: 259-61
8. Tateishi Y, Tagami A, Baba H, Osaki M, Kawakami A, Akira T. Duplex ultrasonography-detected positional vertebral artery occlusion in upper cervical rheumatoid arthritis. Spine. 2016. 41: 26-31
9. Vilanilam GK, Gopal N, Middlebrooks EH, Huang JF, Bhatt AA. Compressive lesions of the head and neck: Common and uncommon must-know entities. Neuroradiol J. 2023. 37: 164-77
10. Zaidi HA, Albuquerque FC, Chowdhry SA, Zabramski JM, Ducruet AF, Spetzler RF. Diagnosis and management of bow hunter’s syndrome: 15-year experience at barrow neurological institute. World Neurosurg. 2014. 82: 733-8
11. Zenmyo M, Ijiri K, Sasaki H, Sakakima H, Taketomi E, Nagayoshi R. Magnetic resonance angiography for vertebral artery evaluation in rheumatoid arthritis patients. Neurosurgery. 2010. 66: 1174-80 discussion 1180