- Department of Neurosurgery, Kasturba Medical College, Manipal, Manipal Academy of Higher Education, Manipal, India
- Department of Neurosurgery, Post Graduate Institute of Medical Sciences, Rohtak, Haryana, India
- Department of Neurology, Connecticut University, Connecticut, United States,
- Department of Pathology All India Institute of Medical Sciences, New Delhi, India.
- Department of Neurosurgery, All India Institute of Medical Sciences, New Delhi, India.
Correspondence Address:
G. Lakshmi Prasad, Department of Neurosurgery, Kasturba Medical College, Manipal, Manipal Academy of Higher Education, Manipal, India.
DOI:10.25259/SNI_262_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: G. Lakshmi Prasad1, Gopal Krishna2, Ameya Kale3, Madhu Rajeshwari4, Shashank Sharad Kale5. Eosinophilic granuloma of the cervical spine in a young adult: A rare case report. 14-Jun-2024;15:198
How to cite this URL: G. Lakshmi Prasad1, Gopal Krishna2, Ameya Kale3, Madhu Rajeshwari4, Shashank Sharad Kale5. Eosinophilic granuloma of the cervical spine in a young adult: A rare case report. 14-Jun-2024;15:198. Available from: https://surgicalneurologyint.com/surgicalint-articles/12943/
Abstract
Background: Spinal eosinophilic granulomas (EG) are rare tumors, mostly reported in the pediatric age group. They constitute
Case Description: A 20-year-old male presented with neck pain for a 4-month duration. Six years previously, he had received six cycles of vinblastine for biopsy-proven histiocytosis of an axillary lymph node; this resulted in incomplete remission. Present magnetic resonance/computed tomography (CT) imaging revealed a lytic C2 body lesion with atlantoaxial instability. When the CT-guided biopsy was suggestive of EG, he was managed with definitive surgery and adjuvant radiotherapy.
Conclusion: Cervical spine EG is rare in adults. CT-guided biopsy should confirm the diagnosis and should be followed by definitive surgery and adjuvant radiotherapy.
Keywords: Adults, Cervical spine, Eosinophilic granuloma, Spine
INTRODUCTION
Eosinophilic granulomas (EG) constitute <1% of primary bone neoplasms and typically involve the thoracic spine but rarely the cervical spine.[
CASE ILLUSTRATION
A 20-year-old male presented with neck pain for a 4-month duration. He had 4+/5 quadriparesis with hypertonia but no sensory deficits. Six years previously, he received 6 cycles of vinblastine for biopsy-proven histiocytosis of an axillary lymph node, resulting in complete remission.
X-ray, magnetic resonance (MR), computed tomography (CT) evaluation of EG X-rays, MR, and CT studies were consistent with the diagnosis of a C2 EG.
Cervical spine X-rays revealed osteolytic destruction of the C2 body and atlantoaxial instability (AAI), while CT showed osteolytic destruction of the body/pedicles of C2 [
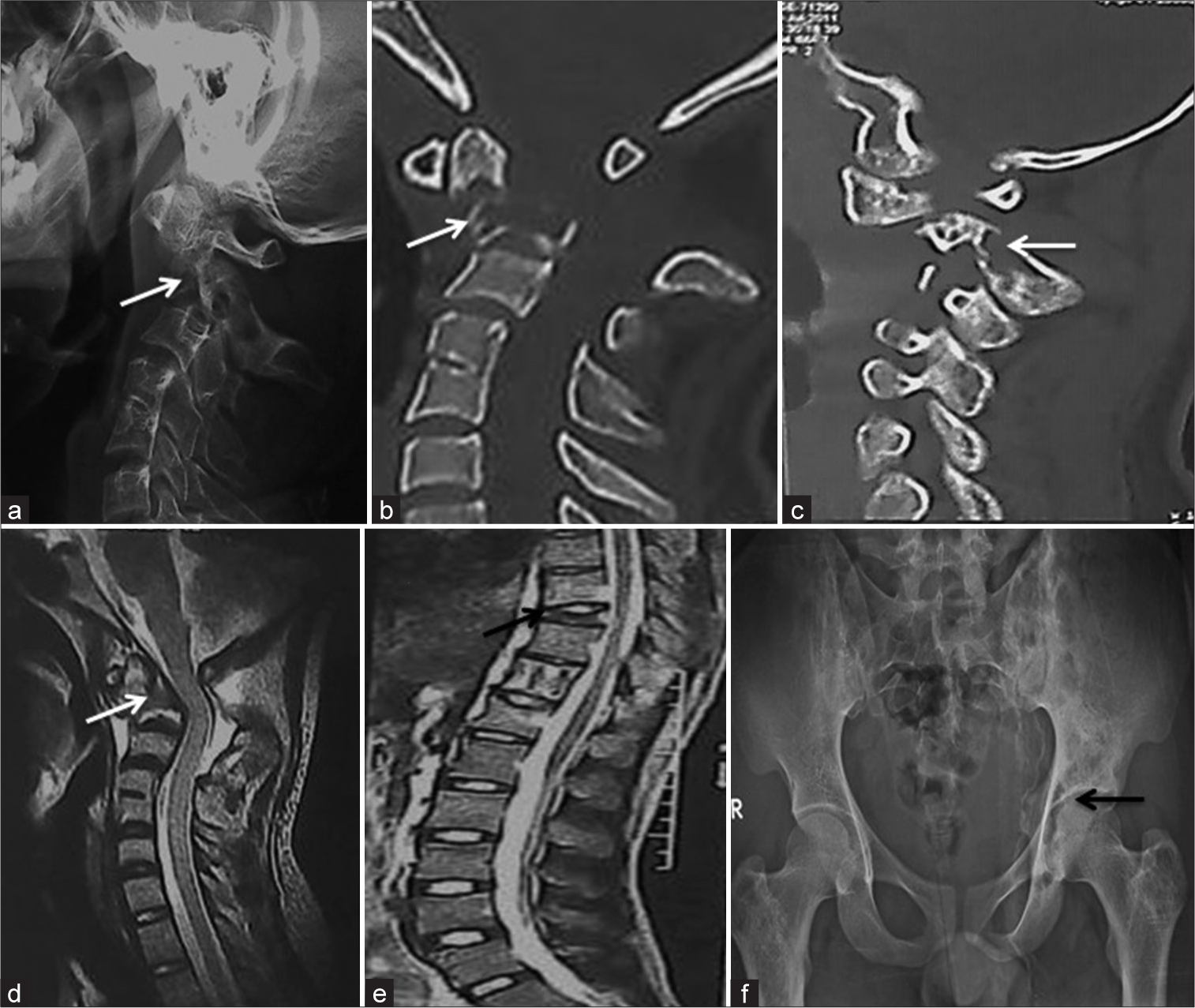
Figure 1:
(a) Plain radiographs of the cervical spine showing an osteolytic destruction of the C2 vertebral body with atlanto-axial instability (white arrow). (b,c) Sagital CT-median and paramedian images showing destruction of the body and pedicles of C2 vertebra (white arrows). (d) Sagital T2 MRI showed iso to hypointense signal at the site of bony defect with evidence of thecal sac compression (white arrow). (e,f) Note that the disc spaces are not involved. Dorsal spine sagittal T2 MRI sequence showing features of vertebra plana of the T9 vertebral body (black arrow) and lytic destruction of the left femoral head (black arrow).
Pathology
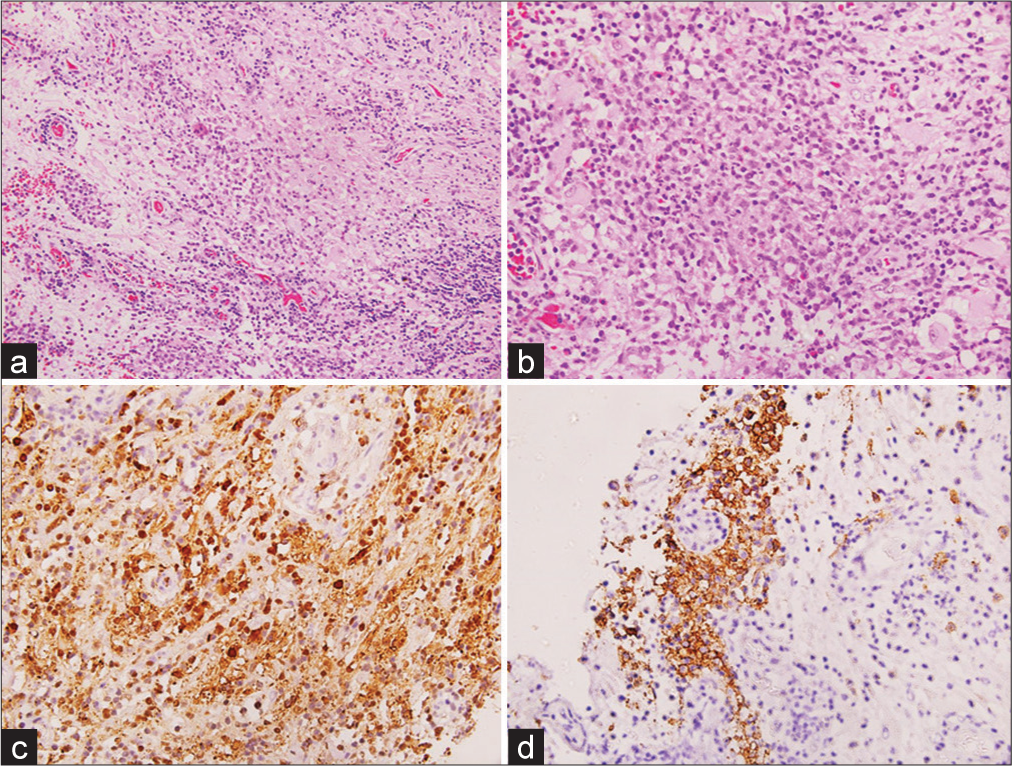
Histopathological examination showed clusters and sheets of cells with abundant cytoplasm, grooved nuclei, delicate chromatin, and inconspicuous nucleoli in a background of inflammatory infiltrate rich in lymphocytes, plasma cells, and eosinophils [
Figure 2:
(a,b) Photomicrograph showing clusters of large cells with abundant cytoplasm in a background of inflammatory cells (H&E, x200), which have abundant cytoplasm and indented/grooved nuclei (H&E, x400). (c,d) These cells are immunopositive for S100 and CD 1a (IHC, x400). IHC:immunohistochemistry, H&E:Haematoxylin and Eosin.
Follow-up treatment
He later received adjuvant low-dose radiation therapy in view of his positive history. At the follow-up of 2 years, the patient was doing well and there was no deformity or recurrence noted.
DISCUSSION
Clinical and radiographic presentation of EG
EG is considered to be the most benign and localized form of LCH and accounts for around three-fourths of those cases.[
Role of surgery
The role of surgery is controversial and should be limited to situations where there is a question regarding the diagnosis, bony instability, and/or severe neurological deficits.[
Role of RT
The role of adjuvant RT has not been clearly defined in the literature.[
Role of chemotherapy
Chemotherapy is indicated only in cases of multifocal/systemic disease or as first-line therapy in the pediatric age group with solitary EG in locations that preclude safe and complete resection.[
Pathology
On gross pathological examination, EG appears reddish-brown to yellow with intervening bony spicules. On microscopy, histiocytes are predominant cells which contain oval nuclei, eosinophilic cytoplasm, and CD1a positivity. Birbeck’s granules are characteristically seen on electron microscopy, and S-100 protein immunohistochemical staining is diagnostic. Nuclear atypia and mitosis are rare features, and differential diagnosis includes Erdheim-Chester disease, Rosai-Dorfman disease, and other dendritic neoplasms.[
CONCLUSION
Cervical spine EG is rare in adults. CT-guided biopsy should be used to confirm the diagnosis and be followed by definitive surgery and adjuvant RT.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
No financial support.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Bertram C, Madert J, Eggers C. Eosinophilic granuloma of the cervical spine. Spine (Phila Pa 1976). 2002. 27: 1408-13
2. Favara BE, Jaffe R. The histopathology of Langerhans cell histiocytosis. Br J Cancer. 1994. 23: S17-23
3. Huang W, Yang X, Cao D, Xiao J, Yang M, Feng D. Eosinophilic granuloma of spine in adults: A report of 30 cases and outcome. Acta Neurochir (Wien). 2010. 152: 1129-37
4. Huang WD, Yang XH, Wu ZP, Huang Q, Xiao JR, Yang MS. Langerhans cell histiocytosis of spine: A comparative study of clinical, imaging features, and diagnosis in children, adolescents, and adults. Spine J. 2013. 13: 1108-17
5. Jiang L, Liu ZJ, Liu XG, Zhong WQ, Ma QJ, Wei F. Langerhans cell histiocytosis of the cervical spine. A single Chinese institution experience with thirty cases. Spine (Phila Pa 1976). 2010. 35: E8-15
6. Prasad GL, Divya S. Eosinophilic granuloma of the cervical spine in adults: A review. World Neurosurg. 2019. 125: 301-11
7. Reddy PK, Vannemreddy PS, Nanda A. Eosinophilic granuloma of spine in adults: A case report and review of literature. Spinal Cord. 2000. 38: 766-8
8. Richter MP, D’Angio GJ. The role of radiation therapy in the management of children with histiocytosis X. Am J Pediatr Hematol Oncol. 1981. 3: 161-3
9. Yeom JS, Lee CK, Shin HY, Lee CS, Han CS, Chang H. Langerhans’ cell histiocytosis of the spine. Analysis of twenty-three cases. Spine (Phila Pa 1976). 1999. 24: 1740-9
10. Zheng W, Wu J, Wu Z, Xiao J. Atlantoaxial instability secondary to eosinophilic granuloma of the axis in adults: Long-term follow-up in six cases. Spine J. 2014. 14: 2701-9