- Department of Neurosurgery, Baylor College of Medicine, Houston, Texas,
- Department of Medicine, Brigham and Women’s Hospital, Boston, Massachusetts,
- Departments of Cardiology, Texas Children’s Hospital, Houston, Texas,
- Departments of Neurosurgery, Texas Children’s Hospital, Houston, Texas,
- Department of Neurosurgery, Lurie Children’s Hospital, Chicago, Illinois,
- Department of Neurosurgery, University of California San Diego, San Diego, California, United States.
Correspondence Address:
Marc Andrew Prablek, Department of Neurosurgery, Baylor College of Medicine, Houston, Texas, United States.
DOI:10.25259/SNI_48_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Marc Andrew Prablek1, Melissa LoPresti1, Brandon Bertot2, Shaine Alaine Morris3, David Bauer4, Sandi Lam5, Vijay Ravindra6. Evaluation of cervical spine pathology in children with Loeys-Dietz syndrome. 18-Mar-2022;13:96
How to cite this URL: Marc Andrew Prablek1, Melissa LoPresti1, Brandon Bertot2, Shaine Alaine Morris3, David Bauer4, Sandi Lam5, Vijay Ravindra6. Evaluation of cervical spine pathology in children with Loeys-Dietz syndrome. 18-Mar-2022;13:96. Available from: https://surgicalneurologyint.com/surgicalint-articles/11451/
Abstract
Background: Loeys-Dietz syndrome (LDS) is a genetic connective tissue disorder associated with multiple musculoskeletal anomalies, including cervical spine instability. We sought to examine the nature of imaging for cervical spine instability in children with LDS due to likely pathogenic or pathogenic variants in TGFBR1, TGFBR2, TGFB2, SMAD3, or TGFB3.
Methods: A retrospective chart review was conducted, examining relevant data for all children with LDS screened at our institution from 2004 through 2021. Cervical spine X-rays were used to assess cervical instability, cervical lordosis, and basilar impression.
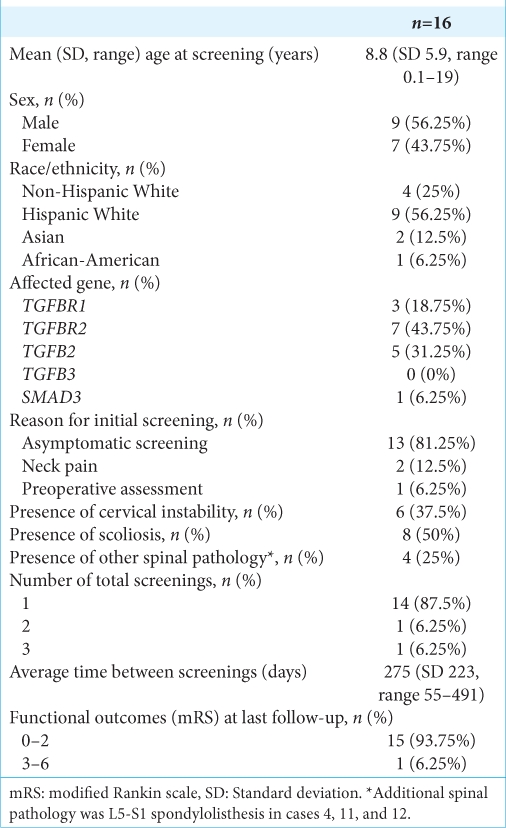
Results: A total of 39 patients were identified; 16 underwent cervical spine screening (56.25% male). Median age at initial screening was 7 years (Q1-Q3: 3.75–14, range: 0.1–19). Six of 16 patients evaluated (37.5%) had radiographical evidence of cervical instability. Mean angles of cervical lordosis were 20° (SD = 14.1°, range = 4°–33°) and 17.3° (SD = 16.4°, range = 2°–41°), respectively. Three patients demonstrated radiographical basilar impression. Radiographic progression of cervical instability was seen in one case. All but two were managed conservatively with observation, one patient underwent surgical fixation and fusion of C1-2, the other underwent complex cervical reconstruction anterior and posterior instrumentation.
Conclusion: Cervical spine evaluation is important in this cohort; we identified 37.5% had evidence of cervical spine instability, and many had concurrent spinal pathology. From our experience, we agree with the recent advisement for screening at diagnosis and for those previously diagnosed that have not undergone screening. Future study may outline more specific screening practices.
Keywords: Basilar impression, Cervical spine instability, Connective tissue disorder, Loeys-Dietz syndrome
INTRODUCTION
Loeys-Dietz syndrome (LDS) is a rare connective tissue disorder characterized by vascular, cardiac, skeletal, craniofacial, and cutaneous anomalies.[
The frequency of cervical spine instability in LDS patients is poorly described in the literature, with a prevalence ranging from 16.3% to 100%.[
MATERIALS AND METHODS
With the Institutional Review Board approval, a retrospective review was performed to identify all patients diagnosed with LDS at Texas Children’s Hospital – Baylor College of Medicine, a tertiary academic referral center, cared for between 2005 and 2018. Patients diagnosed <19 years of age were identified from the institutional Cardiovascular Genetics Program database. LDS diagnosis was defined as presence of a pathogenic or likely pathogenic variant in TGFBR1, TGFBR2, TGFB2, SMAD3, or TGFB3 in conjunction with phenotypic features of LDS, including aortic dilation, arterial tortuosity, and/or craniofacial features. Screening for cervical instability in this study was defined as undergoing cervical spine X-rays. Those without appropriate C-spine imaging were excluded from the study.
Demographic and clinical information examined included age, sex, race/ethnicity, affected gene, symptoms, reason for screening, functional status defined by modified Rankin scale, and management strategy for cervical spine instability if applicable. Due to the retrospective nature of the study, screening was unstandardized and at the discretion of the provider. Screening indications included asymptomatic patients to achieve a baseline or before a procedure which may require intubation or in an area near the cervical spine, symptoms such as neck pain, other spinal pathology to fully evaluate the spine, or neurological complaints localized to the cervical spine. Radiographical data collected included time and interval between X-rays when available, presence of cervical spine instability on X-ray, presence of scoliosis, presence of additional spinal pathology, basilar impression, and cervical lordosis. Descriptive statistics were calculated.
Radiologic parameters measured
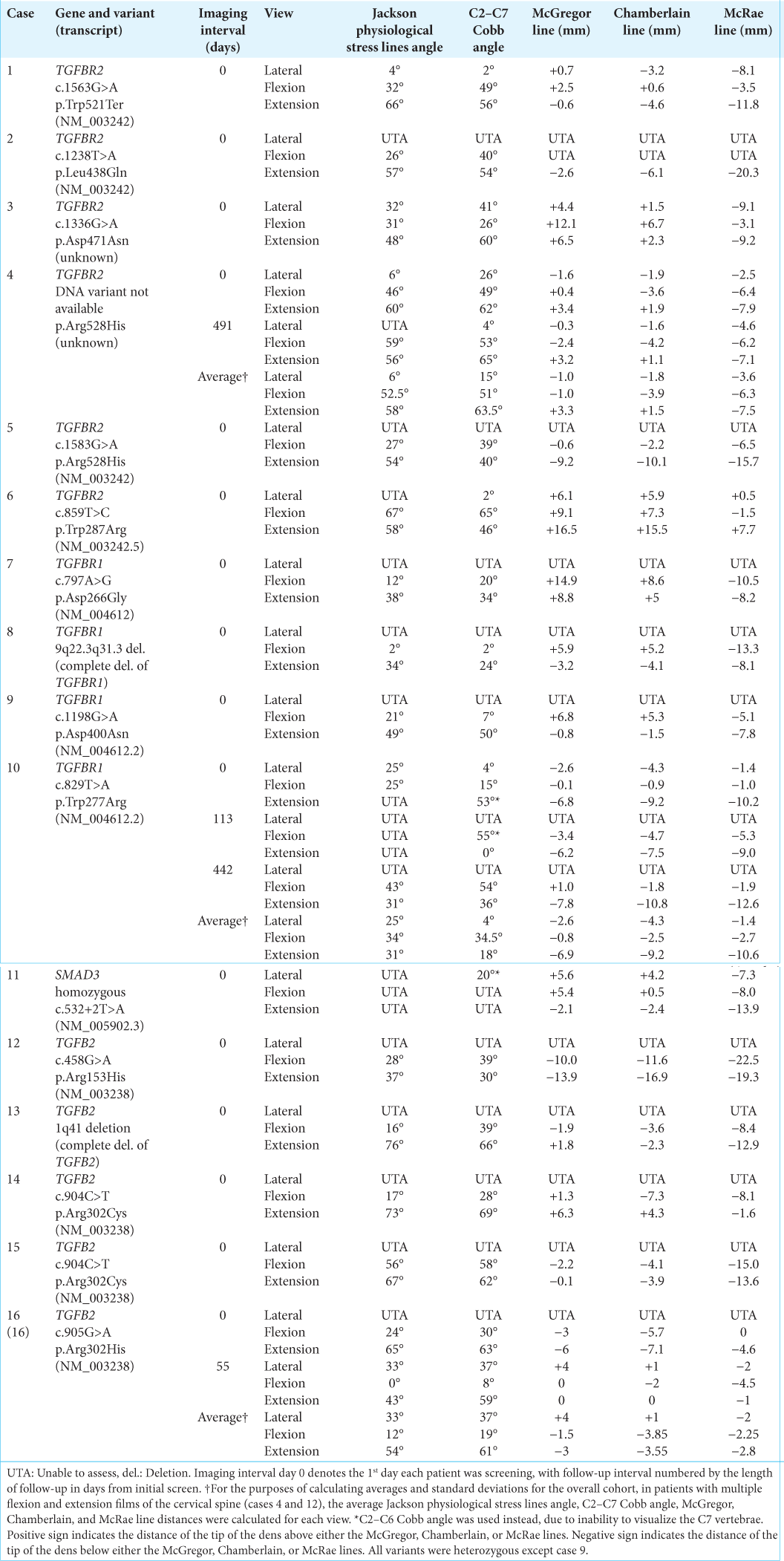
Cervical lordosis and basilar impression were assessed on neutral cervical spine X-rays using commonly accepted cervical spine measurements including the Jackson physiological stress lines angle, the C2–C7 Cobb angle, the C2–C6 Cobb angle, as well as the McGregor, Chamberlain, and McRae lines, shown using representative lateral films in [
The Jackson physiological stress lines and C2–C7 Cobb angle were used to assess the degree of cervical lordosis.[
The McGregor, Chamberlain, and McRae lines were used to identify basilar impression.[
Based on standard clinical criteria, cervical instability was defined in dynamic lateral radiographs as spondylolisthesis or retrolisthesis of one vertebral body on another that changed >2 mm between flexion and extension films.
RESULTS
Of the 39 children treated for LDS at our institution during the study period, 16 (41.02%) were evaluated for cervical instability with cervical spine flexion and extension X-rays [
Cervical spine screening
Sixteen patients underwent initial evaluation; three patients underwent additional imaging after their initial screen. In these patients, the mean interval between imaging was 275 days (SD 223, range 55–491, [
Figure 2:
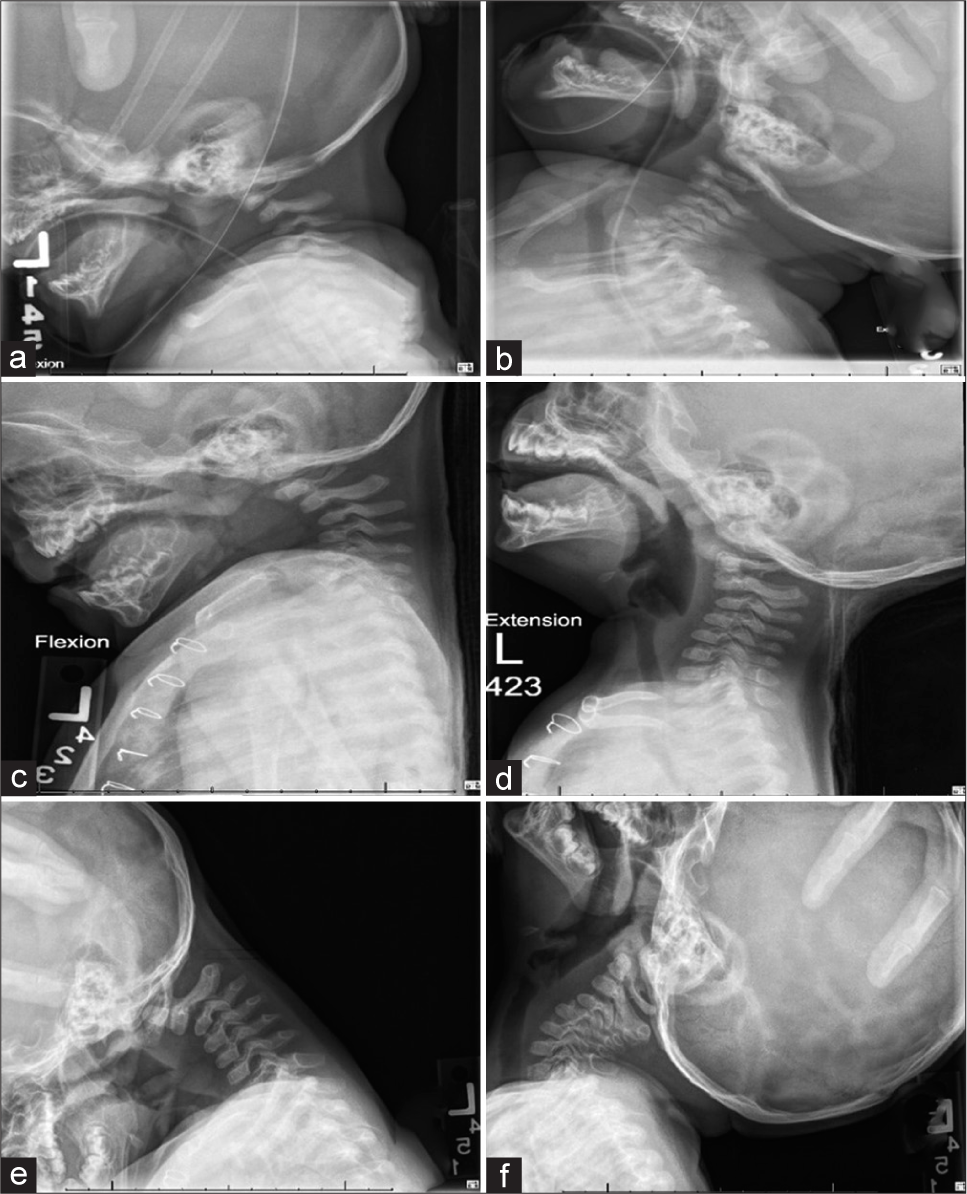
Preoperative cervical spine (a) flexion and (b) extension films at initial screening show slightly hypoplastic C3 vertebra, focal kyphosis at C3 measuring 42° with flexion that reduces to 11° with extension, and cervicothoracic junction lordosis measuring 27° with flexion and 64° with extension. Follow-up cervical spine (c) flexion and (d) extension films at 113 days follow-up demonstrate mild hypoplasia of C3, focal kyphosis with apex at C3 that increases with flexion, and anterior subluxation of C2 on C3 with minimal change in flexion and extension. Follow-up cervical spine (e) flexion and (f) extension films at 442 days follow-up demonstrate 4.5 mm of anterior motion of C2 on C3 in flexion that reduces in extension.
Cervical spine instability
Evaluation of cervical spine flexion-extension radiographs revealed cervical instability in 6 (37.5%) patients with LDS screened [
Cervical spine curvature
[
Basilar impression
Regarding assessment of basilar impression using the McGregor, Chamberlain, and McRae lines, two patients (cases 6 and 11) showed radiologic evidence of basilar impression [
Evidence of radiographic progression
Three cases (4, 10, and 16) had at least two sets of cervical spine radiographs to allow for comparison and evaluation of progression. The mean time between screening was 311 days (SD 189.6, range 113–491). However, cases 10 and 16 had incomplete follow-up imaging, lacking lateral view cervical spine radiographs. Thus, progression was assessed in case 4; the C2–C7 Cobb angle decreased by 22°, while the tip of the dens fell below McGregor, Chamberlain, and McRae lines by 0.3 mm (previously 1.6 mm), 1.6 mm (previously 1.9 mm), and 4.6 mm (previously 2.5 mm), respectively [
Other identified spinal pathologies
Of the 16 patients screened for cervical instability, 8 (50%) had concurrent scoliosis and 4 (25%) had other concurrent spinal pathology, identified as L5-S1 spondylolisthesis [
DISCUSSION
We report our institutional experience with evaluation for cervical spine instability in pediatric patients with LDS. We found an increase in evaluation after guidelines promoted screening. We also found that younger patients tended to be screened more than older patients. From the radiographs of those evaluated, we identified cervical instability, mildly reduced cervical lordosis, and basilar impression among other spinal pathologies in this group. Based on our findings, we underscore the importance of screening, highlight the pathology to recognize and follow, and promote development of a multidisciplinary team to help improve care and inform screening in this population.
Etiology of cervical spinal pathology in LDS
The predisposition to develop cervical pathology, as with other manifestations of LDS, occurs as a result of the altered TGF-β signaling pathway.[
Role of cervical spine evaluation in pediatric patients with LDS
Cervical spine instability in patients with LDS is reported widely in the literature,[
Reviews of literature and expert opinion on LDS recommend cervical spine flexion and extension X-rays at the time of initial diagnosis.[
The first step of treatment is identification of the pathology, underscoring the importance of screening. However, treatment of subclinical or preclinical disease requires caution and weighing of risks and benefits when determining the most appropriate treatment for these complex patients with multiple medical comorbidities and often asymptomatic cervical disease. The literature reports a range of treatments, including observation, bracing, traction, and corrective surgery.[
Other considerations
We also highlight other key features of cervical changes in children with LDS. We found that the mean Jackson physiological stress lines angle was 20°, the mean C2-C7 Cobb angle was 17.3°, and the one C2–C6 Cobb angle was 20°. Among the general population, the normal configuration of the cervical spine is lordotic,[
Cervical spine imaging in LDS patients may reveal additional abnormalities. C1 abnormalities, such as anterior and/or posterior arch defects as well as C1 hypoplasia, and C2 pathologies, including dens elongation, apex anterior angulation of the dens, off center location of the dens, and spondylolysis, can be present.[
Limitations
There are several limitations in our study. Due to the rarity of LDS, the small cohort of patients in our study limits our ability to draw statistically significant conclusions from our data or makes gene-based associations with findings. In addition, the suboptimal screening rate among our cohort, as well as the limited number of those with repeat screenings, perhaps due to developing understanding of disease pathology and evolving recommendations over time, precludes our ability to draw statistically significant conclusions. The retrospective study design also precludes our ability to prospectively assess screening recommendations or subsequently applied changes in management to truly evaluate efficacy of screening protocols. Finally, variability in types of and completeness of radiographs obtained, further limited our ability to assess both cervical spine curvature and basilar impression in all patients, thus reducing our power.
CONCLUSION
Patients with LDS are at risk for a myriad of spinal pathology, including cervical instability and basilar impression. We explored our experience with cervical spine instability evaluation in a pediatric cohort with LDS to identify the pathology diagnosed with screening to help inform and improve the role of screening in management in this group. We found that while screening was not universal, there was a 37.5% prevalence of cervical spine instability, presence of reduced cervical spine lordosis, and basilar impression in conjunction with other spinal abnormalities. We believe our results underscore the benefits of screening in these children, congruent with recommendations in the literature. Future studies may target more specific screening guideline improvements, including set intervals, and inform future treatment protocols.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
This work was supported by National Institutes of Health K23HL127266 (to S.A.M.).
Conflicts of interest
S.A.M. serves on the Scientific Advisory Board for Aytu biopharma for development of a clinical trial for vascular Ehlers-Danlos syndrome.
References
1. Akbarnia BA, Thompson MY.editors. The Growing Spine. Heidelberg: Springer; 2016. p.
2. Burdi AR, Huelke DF, Snyder RG, Lowrey GH. Infants and children in the adult world of automobile safety design: Pediatric and anatomical considerations for design of child restraints. J Biomech. 1969. 2: 267-80
3. Chamberlain WE. basilar impression (platybasia): A bizarre developmental anomaly of the occipital bone and upper cervical spine with striking and misleading neurologic manifestations. Yale J Biol Med. 1939. 11: 487-96
4. Cohen J, Michael M. TGFβ/Smad signaling system and its pathologic correlates. Am J Med Genet Part A. 2003. 116A: 1-10
5. Erkula G, Sponseller PD, Paulsen LC, Oswald GL, Loeys BL, Dietz HC. Musculoskeletal findings of Loeys-Dietz syndrome. J Bone Joint Surg Am. 2010. 92: 1876-83
6. Figaji AA. Anatomical and physiological differences between children and adults relevant to traumatic brain injury and the implications for clinical assessment and care. Front Neurol. 2017. 8: 685
7. Fuhrhop SK, McElroy MJ, Dietz HC, MacCarrick GL, Sponseller PD. High prevalence of cervical deformity and instability requires surveillance in Loeys-Dietz syndrome. J Bone Joint Surg Am. 2015. 97: 411-9
8. Gore DR, Sepic SB, Gardner GM. Roentgenographic findings of the cervical spine in asymptomatic people. Spine (Phila Pa 1976). 1986. 11: 521-4
9. Harrison DD, Janik TJ, Troyanovich SJ, Holland B. Comparisons of lordotic cervical spine curvatures to a theoretical ideal model of the static sagittal cervical spine. Spine (Phila Pa 1976). 1996. 21: 667-75
10. Harrison DD, Troyanovich SJ, Harrison DE, Janik TJ, Murphy DJ. A normal sagittal spinal configuration: A desirable clinical outcome. J Manipulative Physiol Ther. 1996. 19: 398-405
11. Harrison DE, Harrison DD, Cailliet R, Troyanovich SJ, Janik TJ, Holland B. Cobb method or Harrison posterior tangent method: Which to choose for lateral cervical radiographic analysis. Spine (Phila Pa 1976). 2000. 25: 2072-8
12. Jackson R.editors. The Cervical Syndrome. Springfield, IL: Charles C. Thomas; 1958. p.
13. Joaquim AF, Ghizoni E, Tedeschi H, Appenzeller S, Riew KD. Radiological evaluation of cervical spine involvement in rheumatoid arthritis. Neurosurg Focus. 2015. 38: E4
14. Kalra VB, Gilbert JW, Malhotra A. Loeys-Dietz syndrome: Cardiovascular, neuroradiological and musculoskeletal imaging findings. Pediatr Radiol. 2011. 41: 1495-504
15. .editors. Loeys-Dietz Syndrome [Database on the Internet]. Seattle: University of Washington; 2008. p.
16. Loeys BL, Schwarze U, Holm T, Callewaert BL, Thomas GH, Pannu H. Aneurysm syndromes caused by mutations in the TGF-β receptor. N Engl J Med. 2006. 355: 788-98
17. LoPresti MA, Ghali MZ, Srinivasan VM, Morris SA, Kralik SF, Chiou K. Neurovascular findings in children and young adults with Loeys-Dietz syndromes: Informing recommendations for screening. J Neurol Sci. 2020. 409: 116633
18. Lustrin ES, Karakas SP, Ortiz AO, Cinnamon J, Castillo M, Vaheesan K. Pediatric cervical spine: Normal anatomy, variants, and trauma. Radiographics. 2003. 23: 539-60
19. MacCarrick G, Black JH, Bowdin S, El-Hamamsy I, Frischmeyer-Guerrerio PA, Guerrerio AL. Loeys-Dietz syndrome: A primer for diagnosis and management. Genet Med. 2014. 16: 576-87
20. Mc GM. The significance of certain measurements of the skull in the diagnosis of basilar impression. Br J Radiol. 1948. 21: 171-81
21. McRae DL, Barnum AS. Occipitalization of the atlas. Am J Roentgenol Radium Ther Nucl Med. 1953. 70: 23-46
22. Scheer JK, Tang JA, Smith JS, Acosta FL, Protopsaltis TS, Blondel B. Cervical spine alignment, sagittal deformity, and clinical implications: A review. J Neurosurg Spine. 2013. 19: 141-59
23. Sousa SB, Lambot-Juhan K, Rio M, Baujat G, Topouchian V, Hanna N. Expanding the skeletal phenotype of Loeys-Dietz syndrome. Am J Med Genet Part A. 2011. 155: 1178-83
24. Takebayashi K, Kubota M, Yuzurihara M, Tachibana S, Kawamata T. The transspinal canal screwing technique for atlantoaxial anomalies: A technical note and 2 case reports. Neurospine. 2019. 16: 293-7
25. Yang JH, Ki CS, Han H, Song BG, Jang SY, Chung TY. Clinical features and genetic analysis of Korean patients with Loeys-Dietz syndrome. J Hum Genet. 2012. 57: 52-6
26. Yetman AT, Beroukhim RS, Ivy DD, Manchester D. Importance of the clinical recognition of Loeys-Dietz syndrome in the neonatal period. Pediatrics. 2007. 119: e1199-202
27. Zhang J, Buser Z, Abedi A, Dong X, Wang JC. Can C2-6 cobb angle replace C2-7 cobb angle? An analysis of cervical kinetic magnetic resonance images and X-rays. Spine (Phila Pa 1976). 2019. 44: 240-5