- Department of Neurosurgery, Kanazawa University, Kanazawa, Ishikawa, Japan.
- Department of Neurosurgery, Ishikawa Prefectural Central Hospital, Kanazawa, Ishikawa, Japan.
Correspondence Address:
Tomoya Kamide
Department of Neurosurgery, Kanazawa University, Kanazawa, Ishikawa, Japan.
DOI:10.25259/SNI_836_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tomoya Kamide1, Kouichi Misaki1, Takehiro Uno1, Akifumi Yoshikawa1, Naoyuki Uchiyama2, Mitsutoshi Nakada1. Extracranial-intracranial high-flow bypass as a rescue therapy for incomplete cerebral aneurysm occlusion after flow diversion: A case report. 17-Feb-2021;12:57
How to cite this URL: Tomoya Kamide1, Kouichi Misaki1, Takehiro Uno1, Akifumi Yoshikawa1, Naoyuki Uchiyama2, Mitsutoshi Nakada1. Extracranial-intracranial high-flow bypass as a rescue therapy for incomplete cerebral aneurysm occlusion after flow diversion: A case report. 17-Feb-2021;12:57. Available from: https://surgicalneurologyint.com/surgicalint-articles/10596/
Abstract
Background: Excellent treatment outcomes using a pipeline embolization device (PED) have been reported. However, several limitations exist. For example, patients must receive antiplatelet therapy for at least several months, and few alternative treatments exist except for inserting additional flow diverter stents in cases where aneurysm obliteration is not obtained.
Case Description: A 67-year-old female suffered from an asymptomatic large aneurysm of the left paraclinoid internal carotid artery (ICA). She underwent endovascular coil embolization, but coil compaction was confirmed at 2-year follow-up. A PED was inserted as an additional treatment. Unfortunately, the patient was required to discontinue antiplatelet therapy to undergo orthopedic surgery for her severe osteoarthritis of the knee. However, surveillance imaging performed 2 years after insertion of the PED revealed persistent filling into the aneurysm, and we could not stop the antiplatelet therapy to proceed with orthopedic surgery. Therefore, we performed ICA trapping with extracranial-intracranial high-flow bypass to cease antiplatelet therapy promptly. Antiplatelet therapy was completed 3 months after the rescue surgery, and the patient underwent orthopedic surgery.
Conclusion: The authors describe a case of failure of complete obliteration after treatment using a PED, which required cessation of antiplatelet therapy to receive orthopedic surgery. Although safety and efficacy of PED treatment have been reported, we must consider the possibility of other diseases requiring discontinuation of antiplatelet therapy after PED embolization.
Keywords: Antiplatelet therapy, Flow diverter stent, High-flow bypass, Incomplete occlusion
INTRODUCTION
The use of a pipeline embolization device (PED; Medtronic, Irvine, CA, USA) is well established for complex cerebral aneurysms and has been reported to have excellent treatment outcomes.[
CASE DESCRIPTION
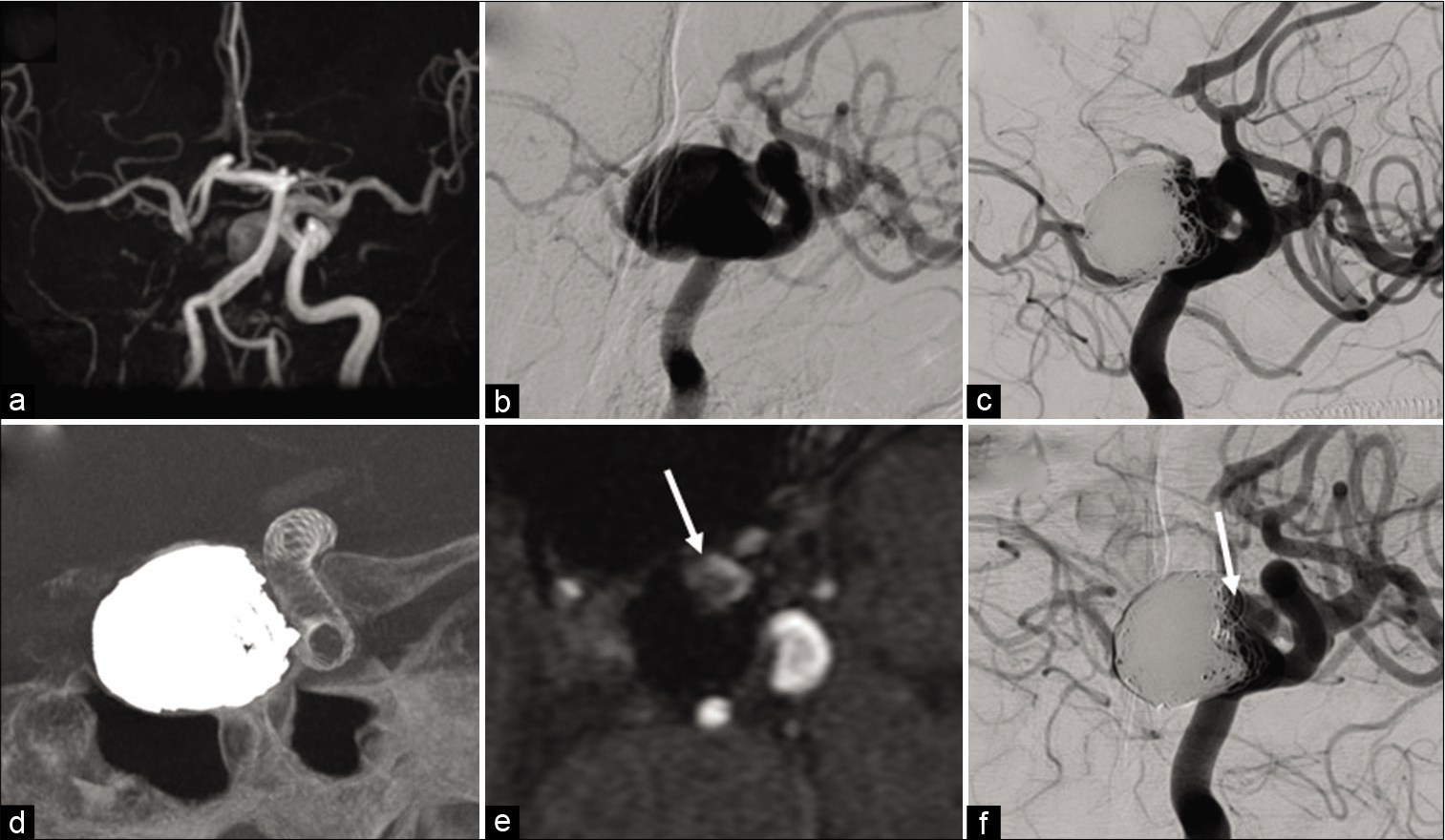
A 67-year-old female with a medical history of congenital dislocation of the hip, which required six surgeries, suffered from an asymptomatic large aneurysm of the left paraclinoid ICA, with agenesis of the right ICA [
Figure 1:
Pretreatment magnetic resonance angiography (MRA) (a) and left internal carotid angiography (b) showing a left large paraclinoid aneurysm and agenesis of the right internal carotid artery. Angiography 2 years after the coil embolization demonstrating aneurysm recurrence (c). Angiography showing the placement of the flow diverter stent (d). Time-of-flight MRA and angiography performed after 2 years after flow diversion showing residual flow into the aneurysm, increasing gradually (e and f arrows).
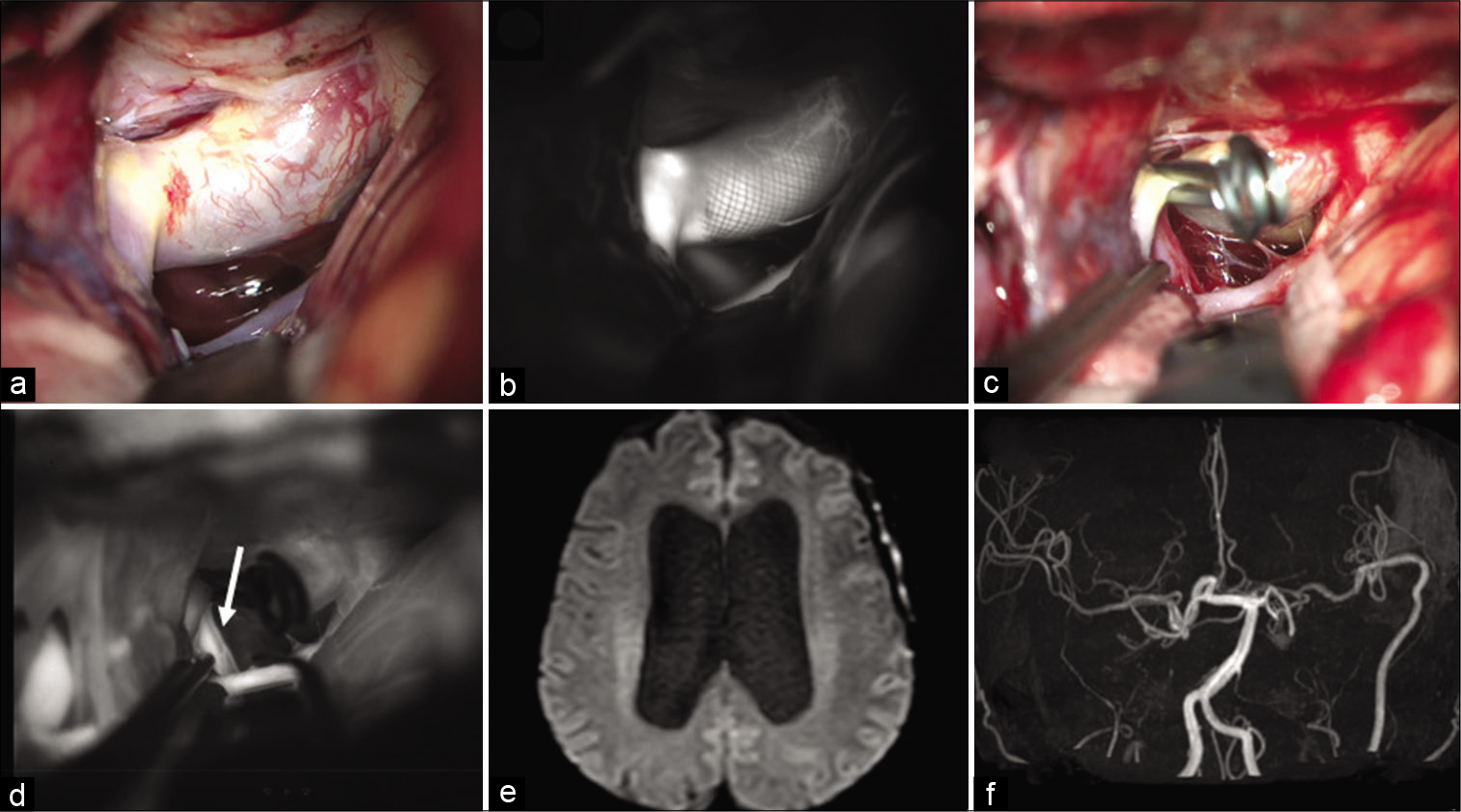
In the operation, the superficial temporal artery (STA) and radial artery (RA) were prepared. The cervical neck was exposed, and the common carotid artery, ICA, and external carotid artery (ECA) were preserved. The Sylvian fissure was opened widely, and the middle cerebral artery (MCA) was exposed. STA-MCA (M4) bypass was performed to ensure cerebral blood flow during occlusion of the MCA (M2), and subsequently, an ECA-RA-MCA (M2) bypass was performed. The PED was clearly confirmed using indocyanine green (ICG) angiography [
Figure 2:
The flow diverter stent was identified (a) and indocyanine green (ICG) angiography showed the distal edge of the stent clearly (b). The internal carotid artery was trapped (c) and ICG angiography demonstrated retrograde flow of the posterior communicating artery was observed (d, arrow). Postoperative magnetic resonance imaging (e) and angiography (f) showing no ischemia and bypass patency.
A postoperative magnetic resonance imaging and angiography showed bypass patency without ischemic change [
DISCUSSION
The treatment of flow diverter stents has become mainstream for the treatment of intracranial large and giant wide-necked aneurysms, and numerous studies have reported the safety and efficacy of PED treatment.[
A serious complication associated with PED treatment is parent artery occlusion due to the in-stent thrombosis.[
While the relative incidence has declined since the approval of flow diverter stents, EC-IC bypass could offer an important alternative treatment in a subset of appropriate patients.[
CONCLUSION
We described a case of incomplete aneurysm obliteration after PED treatment and ICA trapping with EC-IC high-flow bypass to discontinue antiplatelet therapy. A high rate of complete occlusion after PED treatment has been reported, but it is sometimes dangerous to discontinue antiplatelet therapy, especially in cases without complete aneurysm obliteration. Physicians must consider the possibility of other diseases requiring discontinuation of antiplatelet therapy over a long period after PED embolization.
Declaration of patient consent
Patient’s consent not required as patients identify is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Adeeb N, Moore JM, Wirtz M, Griessenauer CJ, Foreman PM, Shallwani H. Predictors of incomplete occlusion following pipeline embolization of intracranial aneurysms: Is it less effective in older patients?. AJNR Am J Neuroradiol. 2017. 38: 2295-300
2. Becske T, Kallmes DF, Saatci I, Mcdougall CG, Szikora I, Lanzino G. Pipeline for uncoilable or failed aneurysms: Results from a multicenter clinical trial. Radiology. 2013. 267: 858-68
3. Bender MT, Colby GP, Lin LM, Jiang B, Westbroek EM, Xu R. Predictors of cerebral aneurysm persistence and occlusion after flow diversion: A single-institution series of 445 cases with angiographic follow-up. J Neurosurg. 2019. 130: 259-67
4. Kadirvel R, Ding YH, Dai D, Rezek I, Lewis DA, Kallmes DF. Cellular mechanisms of aneurysm occlusion after treatment with a flow diverter. Radiology. 2014. 270: 394-9
5. Kallmes D, Brinjikji W, Cekirge S, Fiorella D, Hanel RA, Jabbour P. Safety and efficacy of the pipeline embolization device for treatment of intracranial aneurysms: A pooled analysis of 3 large studies. J Neurosurg. 2017. 127: 775-80
6. Maragkos GA, Ascanio LC, Salem MM, Gopakumar BA, Gomez-Paz S, Enriquez-Marulanda A. Predictive factors of incomplete aneurysm occlusion after endovascular treatment with the pipeline embolization device. J Neurosurg. 2020. 132: 1598-605
7. Moshayedi H, Omofoye OA, Yap E, Oyekunle TO, Sasaki-Adams DM, Solander SY. Factors affecting the obliteration rate of intracranial aneurysms treated with a single pipeline embolization device. World Neurosurg. 2017. 104: 205-12
8. Oishi H, Teranishi K, Nonaka S, Yamamoto M, Arai H. Symptomatic very delayed parent artery occlusion after flow diversion stent embolization. Neurol Med Chir (Tokyo). 2016. 56: 350-3
9. Potts MB, Shapiro M, Zumofen DW, Raz E, Nossek E, Desousa KG. T. Parent vessel occlusion after pipeline embolization of cerebral aneurysms of the anterior circulation. J Neurosurg. 2017. 127: 1333-41
10. Straus DC, da Silva HB, McGrath L, Levitt MR, Kim LJ, Ghodke BV. Cerebral revascularization for aneurysms in the flow-diverter era. Neurosurgery. 2017. 80: 759-68