- Division of Neurosurgery, American University of Beirut Medical Center, Beirut, Lebanon
- Faculty of Medicine, American University of Beirut, Beirut, Lebanon
- Department of Pathology and Laboratory Medicine, American University of Beirut Medical Center, Beirut, Lebanon
Correspondence Address:
Dr. Marwan Najjar, Division of Neurosurgery, American University of Beirut Medical Center, Beirut, Lebanon.
DOI:10.25259/SNI_373_2025
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohamad El Houshiemy1, Ibrahim Murad2, Wael Ali Shouman2, Rayyan Sakr3, Sarah Kawtharani1, Marwan Najjar1. Extradural cervical spinal meningioma without myelopathy. 06-Jun-2025;16:219
How to cite this URL: Mohamad El Houshiemy1, Ibrahim Murad2, Wael Ali Shouman2, Rayyan Sakr3, Sarah Kawtharani1, Marwan Najjar1. Extradural cervical spinal meningioma without myelopathy. 06-Jun-2025;16:219. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13621
Abstract
Background: Only 2.5-3.5% of all spinal meningiomas are extradural.
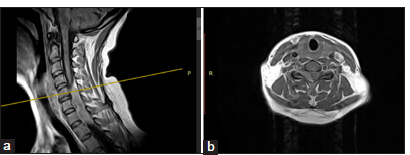
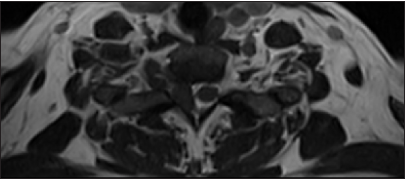
Case Description: A 45-year-old female presented with chronic neck pain and bilateral arm numbness but was otherwise neurologically normal. The cervical magnetic resonance (MR) imaging revealed a right-sided extradural extramedullary lesion extending from C5 to C7. Through a C4-C7 laminectomy, the patient underwent subtotal tumor excision; the intracanalicular portion of the tumor was excised, leaving behind some extraforaminal components. The histopathology was consistent with a typical meningioma (i.e., containing meningothelial cells and psammomatous calcifications).
Conclusion: Extradural cervical spinal meningiomas are rare. Following MR studies, patients may undergo routine dorsal resection of the intracanalicular components of the meningioma, leaving behind extraforaminal extension if warranted. Early recognition and treatment lead to the most favorable outcomes.
Keywords: Cervical spinal meningioma, Extradural tumors, Neck pain, Nerve tumor
INTRODUCTION
Purely extradural meningiomas occur 2.5–3.5% of the time and must be differentiated with biopsy/resection from more typical extradural lesions (i.e., including lymphomas, metastatic tumors, or intradural/extradural schwannomas).[
CASE PRESENTATION
Over 2 months, a 45-year-old female patient presented with chronic neck pain and bilateral arm numbness, but without a focal neurological deficit. The cervical MR image revealed a right-sided extradural extramedullary lesion extending from C5 to C7 [
DISCUSSION
Extradural spinal meningiomas are rare and are more frequently associated with more aggressive behaviors compared to their intradural counterparts.[
MR Findings for extradural spinal meningiomas
MR scans for patients presenting with cervical extradural meningiomas typically include high signal intensity seen on T1-weighted imaging, and mild hyperintensity noted on T2-weighted imaging with marked homogeneous enhancement with contrast (i.e., also often a classical dural tail and/or calcification).[
Treatment of choice for extradural meningiomas
Pathological confirmation utilizing biopsy or tumor resection is essential to differentiate extradural meningiomas from other lesions (i.e., metastases, lymphomas, schwannomas, and neurofibromas).[
CONCLUSION
Only 2.5–3.5% of all spinal meningiomas are extradural. Here, a 45-year-old female did well following subtotal resection of a combined intracanalicular (full removal)/foraminal (residual tumor) benign extradural meningioma through a right-sided C4-C7 laminectomy.
Ethical approval:
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship:
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ben Nsir A, Boughamoura M, Mahmoudi H, Kilani M, Hattab N. Uncommon progression of an extradural spinal meningioma. Case Rep Surg. 2014. 2014: 630876
2. Bettaswamy G, Ambesh P, Das KK, Sahu R, Srivastava A, Mehrotra A. Extradural spinal meningioma: Revisiting a rare entity. J Craniovertebr Junction Spine. 2016. 7: 65-8
3. Frank BL, Harrop JS, Hanna A, Ratliff J. Cervical extradural meningioma: Case report and literature review. J Spinal Cord Med. 2008. 31: 302-5
4. Haranhalli N, Nakhla JP, Yassari R, Kinon MD. Radiographic pearls in the evaluation of an extradural thoracic meningioma: A case report. Cureus. 2017. 9: e1031
5. Hsieh PC, Lu JC, Huang SC, Toh CH, Kuo HC. Unusual clinical presentation of cervical extradural meningioma detected with neuromuscular ultrasound: A case report. Exp Ther Med. 2024. 27: 205
6. Raesh T, Shetty D. Primary cervical extradural Meningioma presenting as neck mass-an unusual presentation of rare case. Int J Preclin Clin Res. 2021. 2: 51-5
7. Redhu R, Pavithra HN. Spinal extradural meningioma: Report of two cases. J Craniovertebr Junction Spine. 2024. 15: 254-57
8. Saade R, Hessel A, Ginsberg L, Fuller G, Bell D. Primary extradural meningioma presenting as a neck mass: Case report and review of the literature. Head Neck. 2015. 37: E92-5
9. Sakamoto K, Tsutsumi S, Nonaka S, Suzuki T, Ishii H, Ito M. Ossified extradural en-plaque meningioma of the cervical spine. J Clin Neurosci. 2018. 50: 124-6
10. Solanke G, Monappa V, Kudva R. Histopathological spectrum of meningiomas with emphasis on prognostic role of Ki67 labelling index. Iran J Pathol. 2020. 15: 197-204
11. Takeuchi H, Kubota T, Sato K, Hirose S. Cervical extradural meningioma with rapidly progressive myelopathy. J Clin Neurosc. 2006. 13: 397-400
12. Yamada S, Kawai S, Yonezawa T, Masui K, Nishi N, Fujiwara K. Cervical extradural en-plaque meningioma-case report. Neurol Med Chir (Tokyo). 2007. 47: 36-9
13. Zevgaridis D, Thomé C. Purely epidural spinal meningioma mimicking metastatic tumor: Case report and review of the literature. Spine (Phila Pa (1976). 2002. 27: E403-5