- Department of Neurosurgery, Krishna Institute of Medical Sciences, Secunderabad, Telangana, India
- Department of Rehabilitation, Krishna Institute of Medical Sciences, Secunderabad, Telangana, India
Correspondence Address:
Manas Kumar Panigrahi, Department of Neurosurgery, Krishna Institute of Medical Sciences, Secunderabad, Telangana, India.
DOI:10.25259/SNI_309_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Manas Kumar Panigrahi1, Pratik Koradia1, Dilip Kumar1, Harshal Dholke1, Sudhindra Vooturi2. Factors influencing outcome in patients with intramedullary spinal cord tumors undergoing resective surgery. 11-Oct-2024;15:370
How to cite this URL: Manas Kumar Panigrahi1, Pratik Koradia1, Dilip Kumar1, Harshal Dholke1, Sudhindra Vooturi2. Factors influencing outcome in patients with intramedullary spinal cord tumors undergoing resective surgery. 11-Oct-2024;15:370. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13145
Abstract
Background: We evaluated whether preoperative functional status influenced surgical outcomes for patients with intramedullary spinal cord tumors (IMSCT).
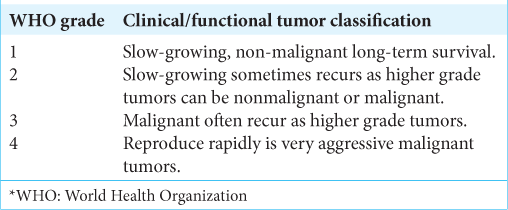
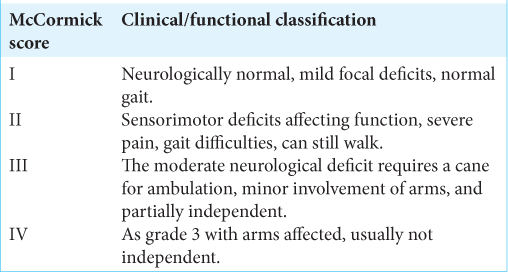
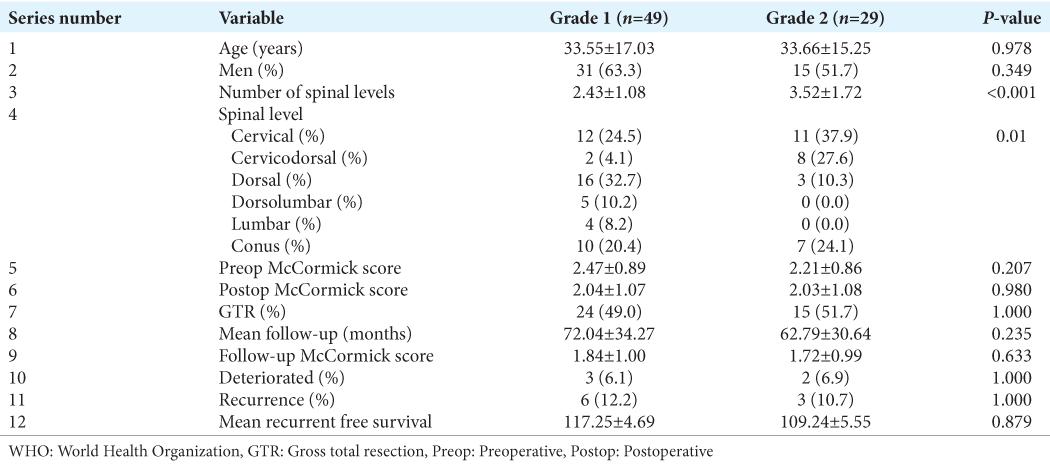
Methods: We analyzed whether lower preoperative McCormick scores impacted primary outcomes for 78 consecutive patients with IMSCT of World Health Organization (WHO) grades I and II undergoing tumor resection between 2010 and 2018.
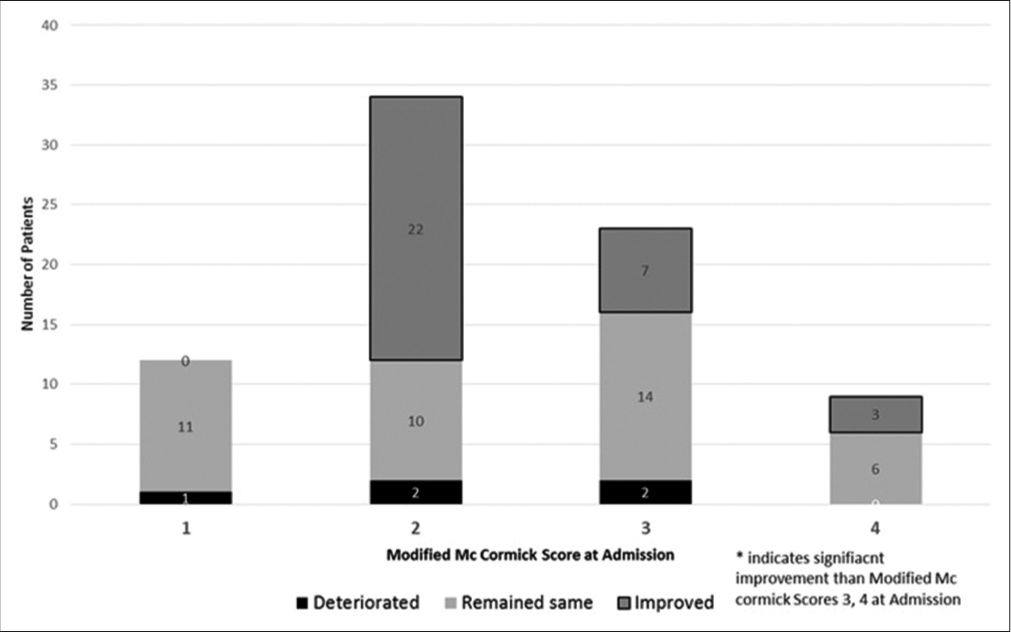
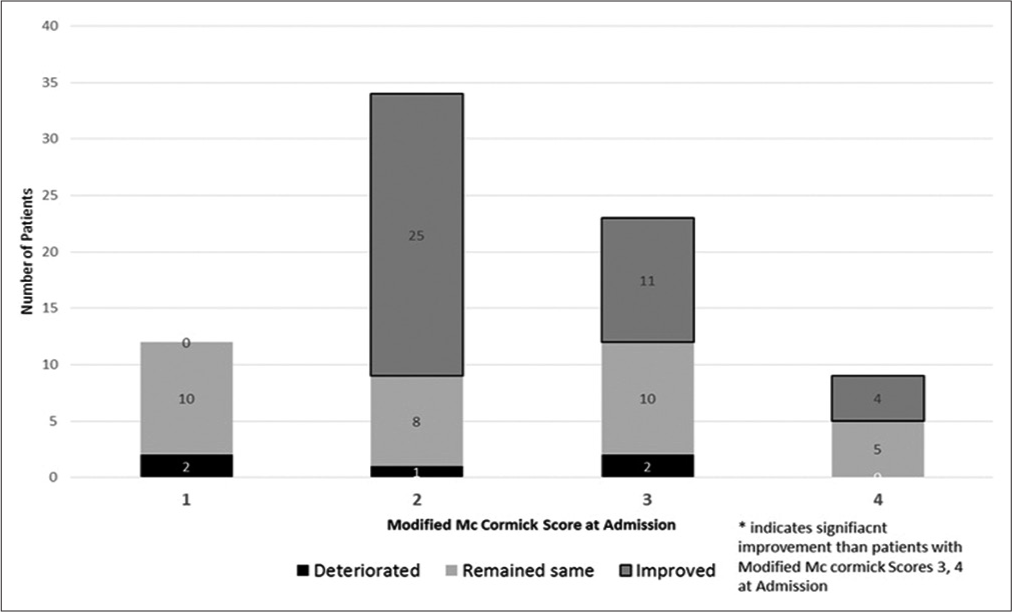
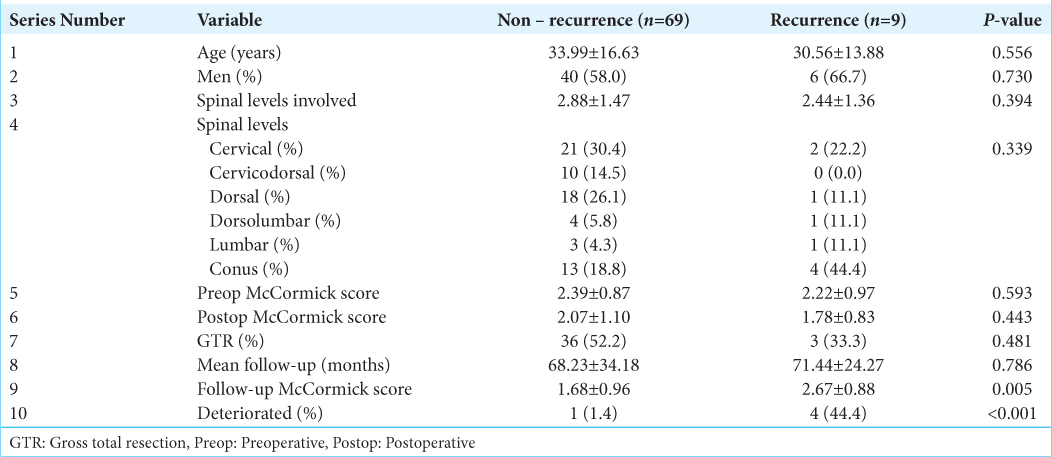
Results: Patients averaged 33.6 years of age, 57.5% were male, and lesions predominantly involved the cervical 23 (29.5%) followed by the thoracic spine 19 (24.3%). Over the average follow-up interval of 69.83 months, IMSCTs recurred in 11.5% of patients, with 6.4% showing functional deterioration. At follow-up, 73.5% of patients with a preoperative modified McCormick score of two or one showed better functional improvement.
Conclusion: The WHO pathological grades I and II did not significantly influence outcomes for patients with intramedullary spinal cord lesions. However, patients with low preoperative McCormick scores (two or one) demonstrated better functional outcomes.
Keywords: Clinical presentation, Extent of resection, Intramedullary tumor, Malignance, Spinal cord
INTRODUCTION
Intramedullary spinal cord tumors (IMSCT) account for 20–30% of primary spinal cord tumors in adults and are predominantly found in the thoracic, followed by the cervical and lumbar regions.[
MATERIALS AND METHODS
This prospective study included 78 consecutive patients with grades I and II IMSCT (i.e., according to the WHO) undergoing tumor resection between 2010 and 2018. Patients averaged 33.60 years of age, 46 (57.5%) were male, and tumors were, respectively, located in the cervical (23 patients = 29.5%), followed by the thoracic (19 = 24.3%) and conus (17 = 21.7%) regions. We were most interested in whether patients with lower preoperative McCormick neurological scores (two or one) or lower grades I and II WHO pathology had better outcomes at 5 postoperative years [
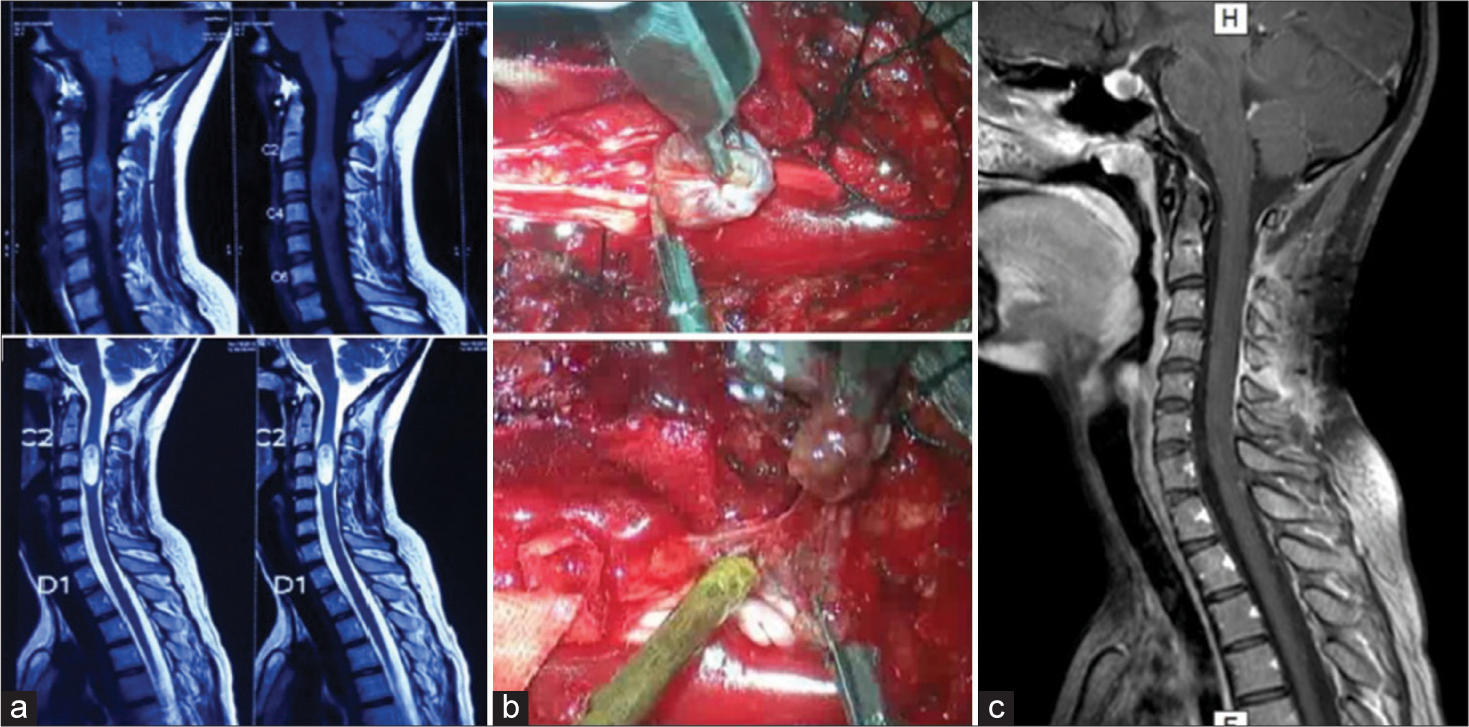
Surgery
Patients underwent routine laminectomies using an operating microscope, intraoperative monitoring, and the Cavitron ultrasonic surgical aspirator to facilitate maximal tumor resections. Adjuvant therapies (routine radiation, cyber knife radiosurgery, or tomo-radiotherapy) were offered to patients with high-grade tumors, progressive disease, and/or for those who had just subtotal tumor resections.
Statistical analysis
The study population was divided into groups based on the WHO grades I and II and recurrence at follow-up. We also used student t-tests and Chi-square tests to evaluate categorical variables. P < 0.05 was considered significant.
RESULTS
Pathology
The WHO histopathology revealed ependymomas in 28 (35.9%) patients [
DISCUSSION
In the present study, 78 patients underwent early surgical resection of low WHO grades I and II IMSCT tumors. Notably, all of our patients were either in the WHO grades I or II, and nearly 73.5% had McCormick Functional scores of two or one (i.e., they could walk independently and had mild neurological deficits [
Extent of spinal segments involved versus outcome
Neither the number of spinal surgical segments nor the location of IMSCT significantly influenced surgical outcomes and/or recurrence rates for the low WHO grade I and II lesions in our sample; this would likely not be true for higher grade lesions. Patients with minimal preoperative deficits (McCormick scores of two or one) were more likely to remain functionally independent at the latest follow-up.
CONCLUSION
Patients with low preoperative McCormick scores (i.e., of one or two) demonstrated better functional outcomes after IMSCT surgery, while WHO grades of I or II did not significantly impact results.
Ethical approval
The study was approved by Institutional Ethics Committee -KFRC/EC/APR/0013/2010.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Duong LM, McCarthy BJ, McLendon RE, Dolecek TA, Kruchko C, Douglas LL. Descriptive epidemiology of malignant and nonmalignant primary spinal cord, spinal meninges, and cauda equina tumors, United States, 2004-2007. Cancer. 2012. 118: 4220-7
2. Fathy M, Keshk M, El Sherif A. Surgical management and outcome of intramedullary spinal cord tumour. Egypt J Neurosurg. 2019. 34: 2
3. Grimm S, Chamberlain MC. Adult primary spinal cord tumors. Expert Rev Neurother. 2009. 9: 1487-95
4. Jallo GI, Danish S, Velasquez L, Epstein F. Intramedullary low-grade astrocytomas: Long-term outcome following radical surgery. J Neurooncol. 2001. 53: 61-6
5. McCormick PC, Torres R, Post KD, Stein BM. Intramedullary ependymoma of the spinal cord. J Neurosurg. 1990. 72: 523-32
6. Raco A, Esposito V, Lenzi J, Piccirilli M, Delfini R, Cantore G. Long-term follow-up of intramedullary spinal cord tumors: A series of 202 cases. Neurosurgery. 2005. 56: 972-81
7. WHO Classification of Tumours Editorial Boa, editors. World Health Organization classification of tumours of the central nervous system. Lyon: International Agency for Research on Cancer; 2021. p.