- Department of Neurosurgery, PGIMER, Chandigarh, India
- Department of Neurosurgery, LSU-HSC, Shreveport, Louisiana, USA
Correspondence Address:
Amey R. Savardekar
Department of Neurosurgery, PGIMER, Chandigarh, India
DOI:10.4103/sni.sni_244_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Harsimrat Bir Singh Sodhi, Amey R. Savardekar, Ravi B. Chauhan, Devi Prasad Patra, Navneet Singla, Pravin Salunke. Factors predicting long-term outcome after short-segment posterior fixation for traumatic thoracolumbar fractures. 26-Sep-2017;8:233
How to cite this URL: Harsimrat Bir Singh Sodhi, Amey R. Savardekar, Ravi B. Chauhan, Devi Prasad Patra, Navneet Singla, Pravin Salunke. Factors predicting long-term outcome after short-segment posterior fixation for traumatic thoracolumbar fractures. 26-Sep-2017;8:233. Available from: http://surgicalneurologyint.com/surgicalint-articles/factors-predicting-long%e2%80%91term-outcome-after-short%e2%80%91segment-posterior-fixation-for-traumatic-thoracolumbar-fractures/
Abstract
Background:The “gold standard” for instrumentation of unstable thoracolumbar fracture-dislocations is pedicle screw and rod fixation. Although traditional treatment supports long-segment posterior fixation (LSPF), more recent studies show short-segment posterior fixation (SSPF) may be effective, but incur higher failure rates. Here, we evaluated the effectiveness of SSPF in the management of unstable thoracolumbar injuries and analyzed the factors impacting long-term outcomes.
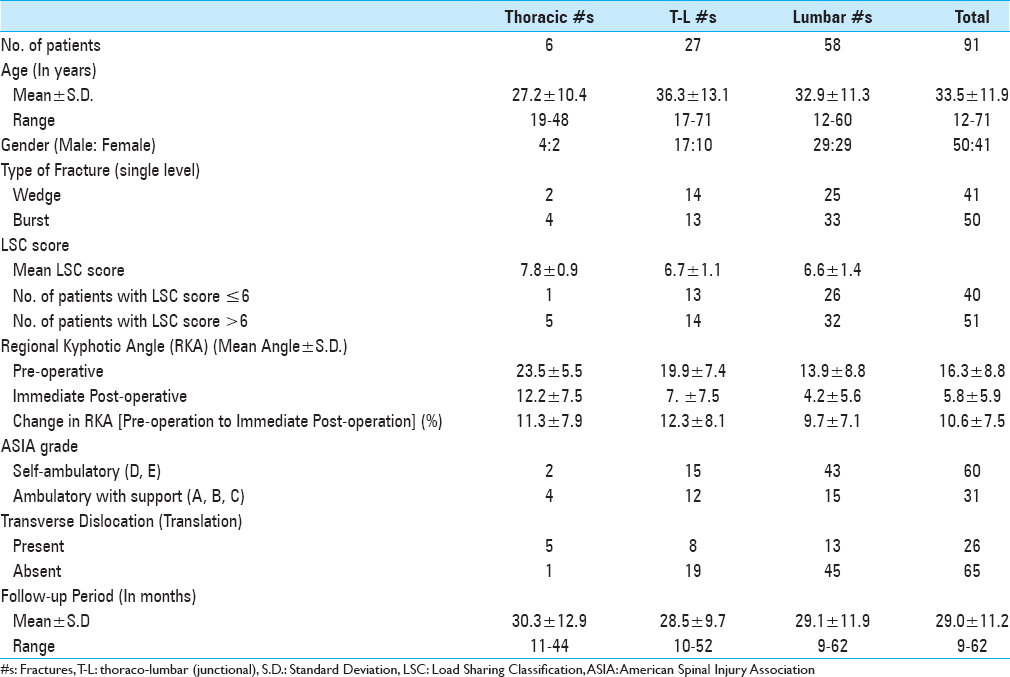
Methods:In this retrospective analysis of 91 patients with thoracolumbar fractures managed with SSPF alone, we assessed the clinical and radiological parameters at preoperative, postoperative, and follow-up intervals along with reasons for failures of SSPF.
Results:We analyzed 91 patients (mean age: 33.5 years; Male: Female = 50:41) with thoracolumbar fractures treated with SSPF over a median follow-up period of 30 months. SSPF failures were observed in 26 of 91 (28.6%) patients; the median time to implant failure was 17 months. On univariate analysis, statistically significant factors contributing to failure of SSPF included the presence of a burst fracture, a preoperative LSC (load-sharing classification) score >6, and translation/dislocation. With multinomial regression analysis, the only factor predictive for SSPF failure was the patients' postoperative ambulatory status.
Conclusion:Patients with thoracolumbar facture dislocations, subjected to axial spinal loading postoperatively, should not be considered for SSPF alone. The following factors also contributed to SSPF failures: a burst fracture, a preoperative LSC score of >6, and/or presence of transverse dislocation.
Keywords: Factors affecting outcome, long-term outcome, short segment posterior fixation, spine fractures, spinal injury, spinal instrumentation, surgical treatment, thoracolumbar fractures
INTRODUCTION
Thoracolumbar spinal trauma resulting in three-column injuries often require surgical intervention to prevent future painful deformity or worsening neurologic function.[
Recent studies document the efficacy of short-segment posterior fixation (SSPF: one level above/below) vs. long-segment posterior fixation (LSPF: two levels above/below). Nevertheless, SSPFs have been associated with a higher rate of implant failure and recurrent kyphosis.[
MATERIALS AND METHODS
Study design and patient population
We retrospectively analyzed 91 patients with traumatic thoracolumbar fractures who underwent SSPF with pedicle screw/rod fixation over 20 months (2012–2013). Clinical and radiological data were obtained from the hospital medical records with prior approval from the Institutional Review Broad.
Inclusion criteria
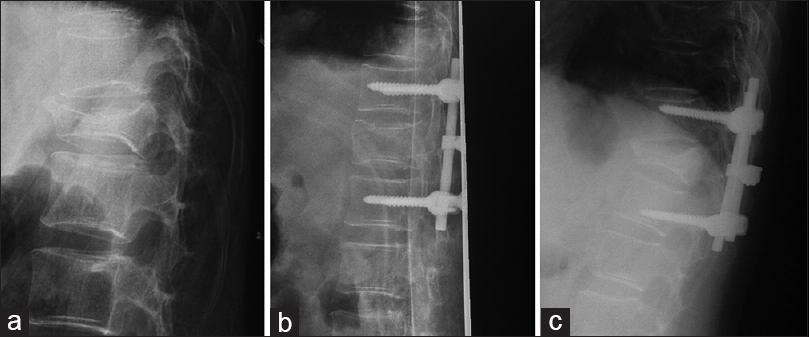
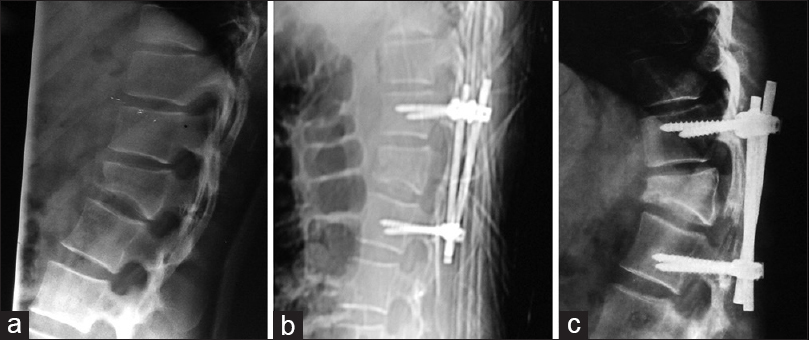
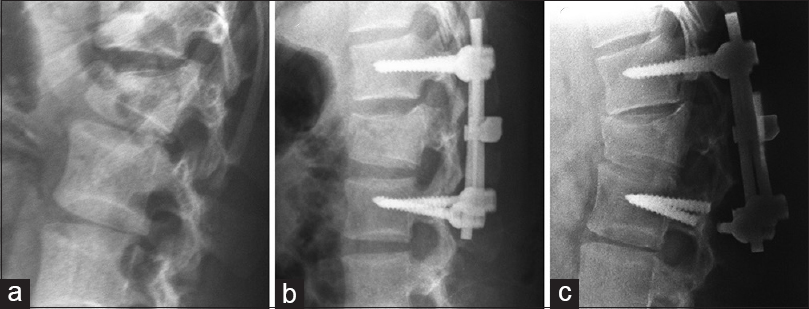
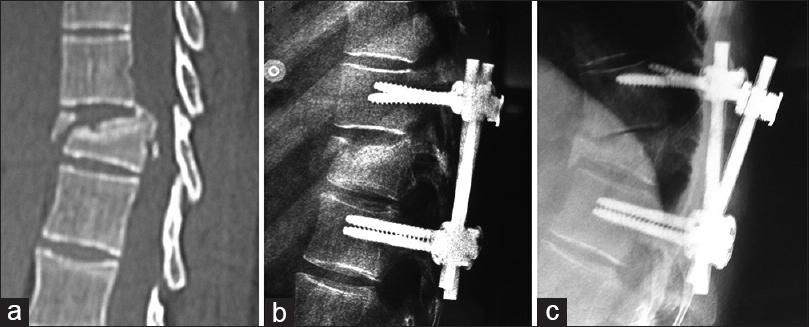
Patients with posttraumatic, single-level thoracolumbar fracture/dislocations undergoing SSPF with pedicle screws/rods with a minimum clinical/radiological follow-up of 18 months were included in the study [
Preoperative data acquisition
Using the ASIA classification system, patients were divided into two groups – ASIA grades A to C (nonambulatory in the postoperative period; no axial load bearing) and ASIA grades D to E (those ambulatory without support in the postoperative period; axial load bearing present). Preoperative assessment included X-rays (anterior-posterior and lateral views), computed tomography (CT thin cuts and 2D reconstructions), and magnetic resonance imaging (MRI). Preoperative radiological parameters studied included assessment of vertebral body height at the fractured segment, regional kyphosis/angular displacement, and evaluation of translation/dislocation. The LSC score was measured for all patients.
Operative intervention
Laminectomy was performed in 43 patients to decompress the neural elements (e.g. those with severe kyphotic deformity and a compromised canal diameter). Next, all had SSPF performed, with two screws placed one level above and two screws placed one level below the fractured segment. A transverse bar connected the longitudinal rods in cases of translation/dislocation (e.g., to reduce rotational motion at the fracture site). Fracture reduction and correction of vertebral body heights was achieved utilizing the distraction/manipulation of the vertebral bodies with screws. Facets were manipulated or partially removed to correct translation/dislocation. Bone chips/dust was inserted into the drilled joint spaces or laid over decorticated joints/lamina to achieve bony fusion.
Postoperative assessment and follow-up
Patient's postoperative ASIA grade and changes in neurological status were noted. Postoperative X-rays/CT studies evaluated: anterior VBH (vertebral body height), posterior VBH, regional kyphotic angle (RKA), change in RKA, and percentage of correction of anterior VBH and posterior VBH. Only patients in whom clinical and radiological follow-up of 18 months could be assessed were included in the study.
Outcome analysis and failure definition
Assessment of outcomes included the evaluation of construct failure rates and the time to construct failure. Construct failure was defined by breakage of a rod/screw (implant failure), increase in kyphotic angle (vs. preoperative scans), decrease in VBH (collapse of vertebral body), and screw pull-out.[
Statistical analysis
Data were presented as mean (±SD) or median [interquartile range (IQR)] in normally distributed or skewed variables, respectively. Normality of data was checked using Kolmogorov–Smirnov tests. For normally distributed data, means were compared using unpaired Student's t-test. For skewed data, Mann–Whitney test was applied. Logistic regression analysis described variables associated with failure of SSPF. Failure-free survivals among different categories were calculated and plotted using Kalpan–Meier curves. All statistical tests were twosided and a probability value <0.05 was considered significant.
RESULTS
Failure of short-segment posterior fixation
In our study, 91 patients with posttraumatic single-level thoracic and lumbar spine fractures underwent SSPF of the unstable spine with pedicle screw and rod fixation [
Factors affecting failure
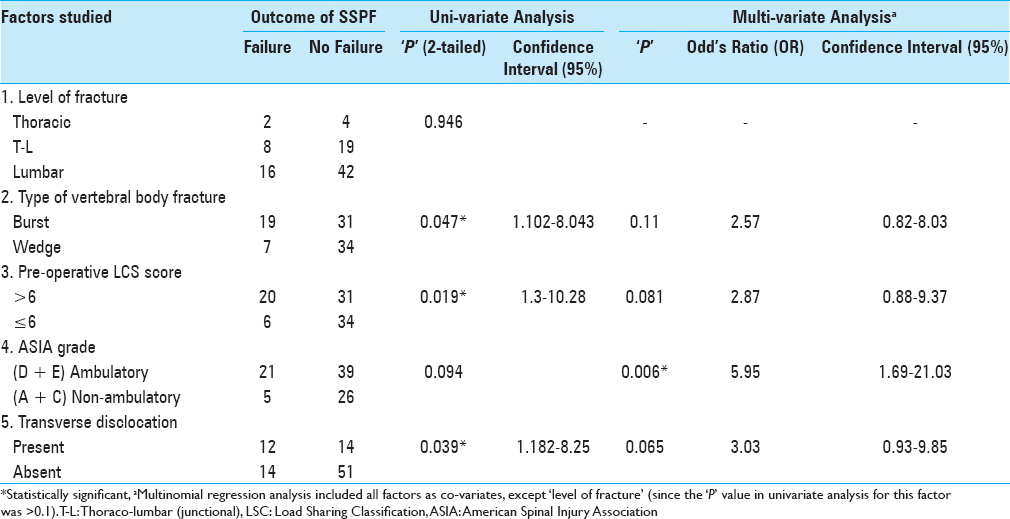
On univariate analysis, the factors with a statistically significant association with failure of SSPF included: the presence of a burst fracture, a preoperative LSC score >6, and translation/dislocation. On multinomial regression analysis (taking factors with P value <1 on univariate analysis as covariates), the only factor which was predictive of failure in SSPF was the postoperative ambulatory status. Patients in ASIA grade D and E were likely to have failure of SSPF (P = 0.0060 and OR = 5.95; 95% CI: 1.69–21.03) [
Failure of SSPF was twice as high in patients with burst-fractures compared to patients with wedge compression fractures (38% versus 17.1%; P = 0.047). Failure of SSPF was seen in 6/40 (15%) patients with LSC 6 (P = 0.019). Failure of SSPF was higher with translation/dislocation [46.2% (12/26)] patients versus those [14/65 (21.5%)] without translation/dislocation (P = 0.039). Failure of SSPF did not significantly correlate with the level of injury – 2/6 (33.3%) thoracic, 8/27 (29.6%) thoracolumbar, and 16/58 (27.5%) lumbar spine injuries. Failure of SSPF was higher (approaching statistical significance) in the ambulatory group [21/60 (35%)] versus the nonambulatory group [5/31 (16.1%)] [
Timing of failure and factors affecting it
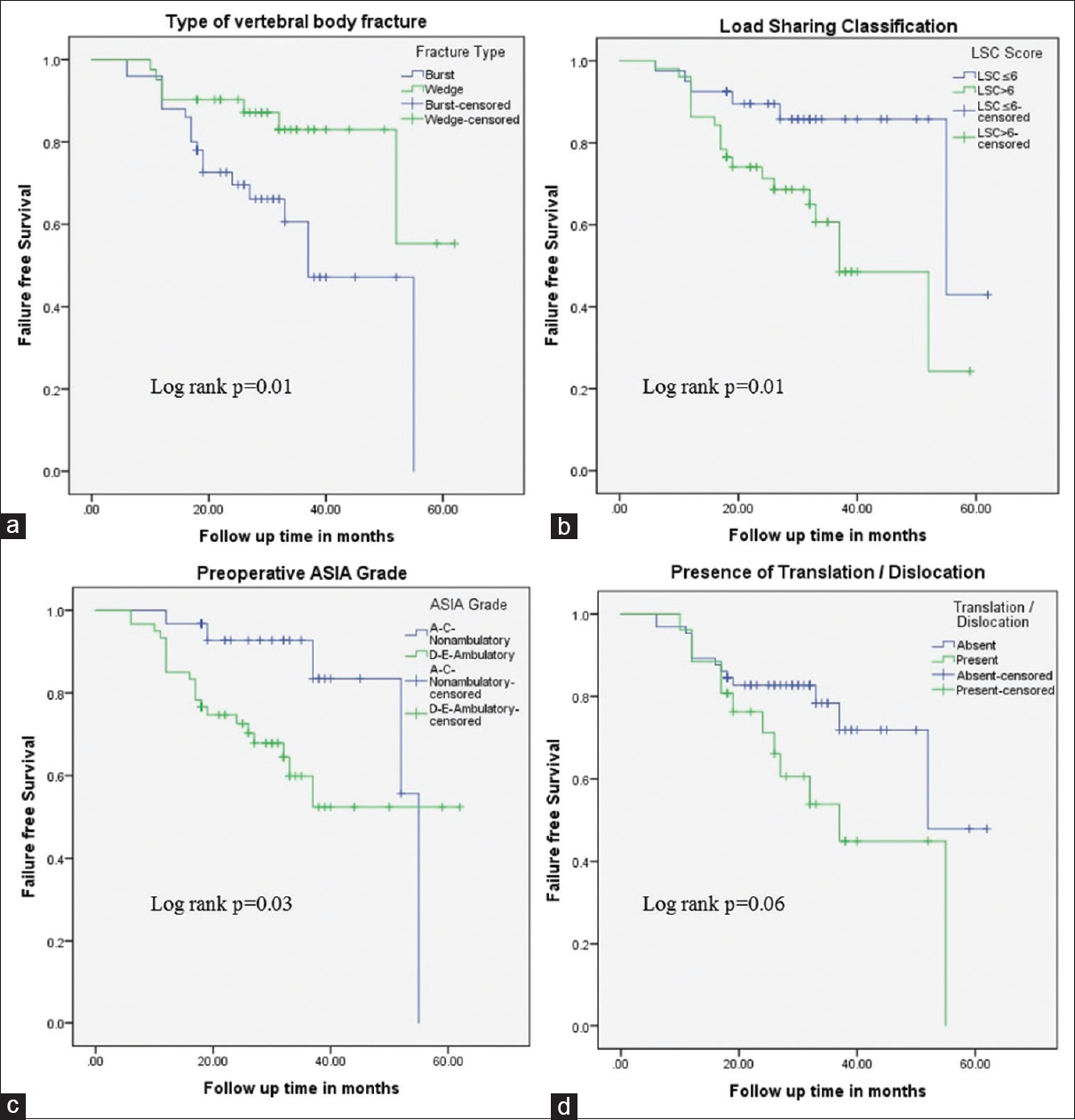
The median time for failure of SSPF was 17 months (IQR: 12–28.2 months). Nearly a quarter failed within 1 year and >90% failed by 4 years after surgery. SSPF in burst fractures failed more than a year earlier than in wedge fractures (38.3 months vs 51.9 months; P = 0.01). Those with preoperative LSC score >6 had early failure versus those with LSC score ≤6 (38.9 months vs. 52.4 months, P = 0.01). Postoperative ambulatory patients (ASIA grade D-E) had early failure than nonambulatory patients (42.9 months vs 49.6 months, P = 0.03). The level of vertebral fracture and presence of transverse dislocation did not affect the timing of failure significantly (P = 0.8 and 0.06, respectively). Kaplan–Meier curves showing difference in the failure-free survivals are shown in
Figure 5
Kaplan–Meier curves showing difference in failure-free survivals. The presence of burst fracture (a) preoperative LSC score >6 (b) and ambulatory status (c) (ASIA grade D and E) affect the timing of failure in patients undergoing standalone SSPF. The presence of translation/dislocation (d) and the level of fracture did not significantly affect the timing of failure in the study group
DISCUSSION
There is considerable controversy regarding the number of vertebral levels to be included in the fixation of thoracolumbar fractures. SSPF involves fixation of one level above and below the fractured vertebra, whereas LSPF involves fixation of at least two levels above and below the fractured vertebra.[
Lazaro et al. compared SSPF versus LPSF of the thoracic spine in an ex-vivo trauma model (3-column injury) and concluded that short-segment fixation provided significantly less stability than long-segment fixation.[
Analysis of outcome in our study group
Construct failure after SSPF can range from 9% to 54%.[
Implant removal
Implant removal was recommended only if the implants were prominent and painful, had lost fixation or had broken, or if revision was indicated for progressive kyphosis.[
McLain et al. reported ten instrumentation failures with SSPF (transpedicular screws) among 19 fractures in their study.[
Factors affecting failure of short-segment posterior fixation and timing of failure
The presence of burst fracture had a statistically significant association with SSPF failure and was associated with early failure after SSPF [
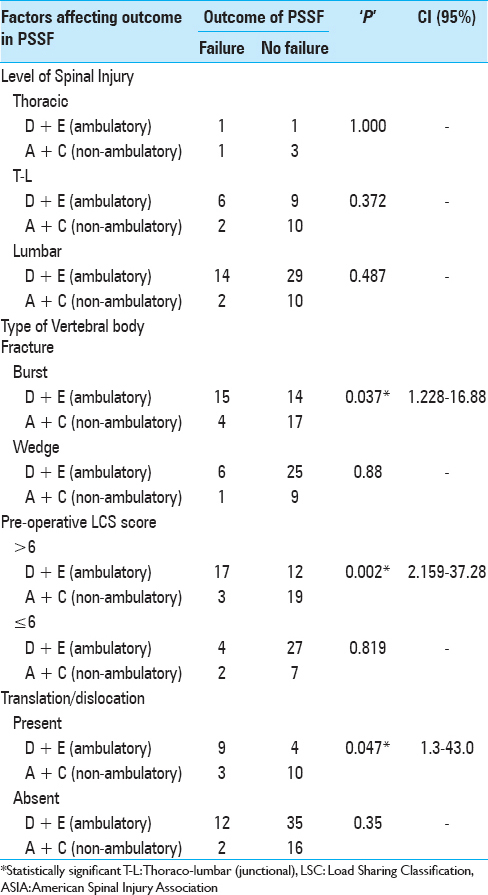
Postoperative ambulation increases short-segment posterior fixation failure
In our study, postoperative ambulatory status was predictive of failure of SSPF. Further subgroup analysis [
Translation/Dislocation
We emphasized the role of translation/dislocation as a cause of recurrent collapse or implant failure with SSPF. This is similar to the results of Parker et al. where a high incidence of recurrent collapse was present in patients with translation/dislocation.[
Limitations of our study
This study only reports on the long-term outcome of one surgical procedure for thoracolumbar fractures, i.e. SSPF.
CONCLUSION
Although SSPF is the most common procedure performed for thoracolumbar fracture-dislocations, is standalone SSPF adequate in treating patients with thoracolumbar fracture- dislocation? Standalone SSPF can be used in a subset of patients with thoracolumbar injuries, if carefully selected. However, those with thoracolumbar facture-dislocations who will be ambulatory in the postoperative period (e.g., subjected to axial loading) should not be considered for SSPF alone particularly if they have accompanying burst fractures, preoperative LSC score >6, and/or translation/dislocation.
Ethical approval: Yes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Altay M, Ozkurt B, Aktekin CN, Ozturk AM, Dogan O, Tabak AY. Treatment of unstable thoracolumbar junction burst fractures with short- or long-segment posterior fixation in magerl type a fractures. Eur Spine J. 2007. 16: 1145-55
2. Alvine GF, Swain JM, Asher MA, Burton DC. Treatment of thoracolumbar burst fractures with variable screw placement or Isola instrumentation and arthrodesis: Case series and literature review. J Spinal Disord Tech. 2004. 17: 251-64
3. Kim HY, Kim HS, Kim SW, Ju CI, Lee SM, Park HJ. Short Segment Screw Fixation without Fusion for Unstable Thoracolumbar and Lumbar Burst Fracture: A Prospective Study on Selective Consecutive Patients. J Korean Neurosurg Soc. 2012. 51: 203-7
4. Lazaro BC, Deniz FE, Brasiliense LB, Reyes PM, Sawa AG, Theodore N. Biomechanics of thoracic short versus long fixation after 3-column injury. J Neurosurg Spine. 2011. 14: 226-34
5. McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine. 1994. 19: 1741-44
6. McLain RF. The biomechanics of long versus short fixation for thoracolumbar spine fractures. Spine. 2006. 31: S70-9
7. McLain RF, Burkus JK, Benson DR. Segmental instrumentation for thoracic and thoracolumbar fractures: Prospective analysis of construct survival and five-year follow-up. Spine J. 2001. 1: 310-23
8. McLain RF, Sparling E, Benson DR. Early failure of short-segment pedicle instrumentation for thoracolumbar fractures. A preliminary report. J Bone Joint Surg. 1993. 75: 162-7
9. Parker JW, Lane JR, Karaikovic EE, Gaines RW. Successful short-segment instrumentation and fusion for thoracolumbar spine fractures: A consecutive 41/2-year series. Spine. 2000. 25: 1157-70
10. Sapkas G, Kateros K, Papadakis SA, Brilakis E, Macheras G, Katonis P. Treatment of unstable thoracolumbar burst fractures by indirect reduction and posterior stabilization: Short-segment versus long-segment stabilization. Open Orthop J. 2010. 4: 7-13
11. Vaccaro AR, Lehman RA, Hurlbert RJ, Anderson PA, Harris M, Hedlund R. A new classification of thoracolumbar injuries: The importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976). 2005. 30: 2325-33
12. Waqar M, Van-Popta D, Barone DG, Bhojak M, Pillay R, Sarsam Z. Short versus long-segment posterior fixation in the treatment of thoracolumbar junction fractures: A comparison of outcomes. Br J Neurosurg. 2017. 31: 54-7