- Department of Neurosurgery, Hospital Santa Maria, Centro Hospitalar Universitário Lisboa Norte EPE, Lisbon, Portugal.
Correspondence Address:
Diogo Roque, Department of Neurosurgery, Hospital Santa Maria, Centro Hospitalar Universitário Lisboa Norte EPE, Lisbon, Portugal.
DOI:10.25259/SNI_1091_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Diogo Roque, José Hipólito-Reis, Pedro Duarte-Batista, Maria Manuel Santos. Fourth ventricle neurocysticercosis presenting with Bruns’ syndrome: A case report. 20-Dec-2021;12:616
How to cite this URL: Diogo Roque, José Hipólito-Reis, Pedro Duarte-Batista, Maria Manuel Santos. Fourth ventricle neurocysticercosis presenting with Bruns’ syndrome: A case report. 20-Dec-2021;12:616. Available from: https://surgicalneurologyint.com/surgicalint-articles/11301/
Abstract
Background: Neurocysticercosis (NCC) is the most common helminthic infection of the central nervous system. We present a case of the fourth ventricle NCC that presented with Bruns’ syndrome (with headaches worsened by head movements, gait ataxia, and vomiting) and the operative technique used for cyst removal.
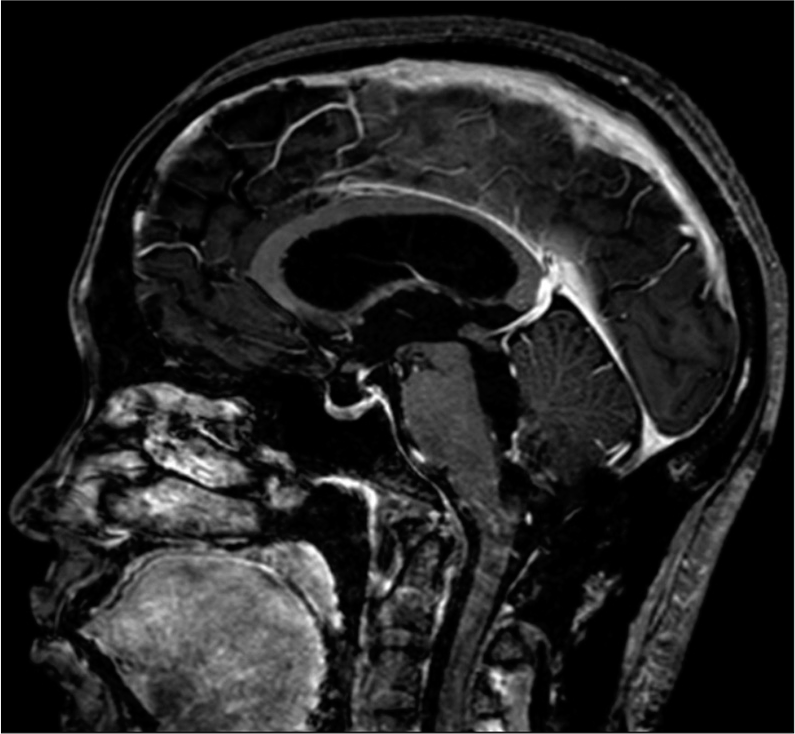
Case Description: A 39-year-old woman was admitted to the emergency department with moderate-to-severe headaches that got worse in the afternoon and were triggered by head movements, relieved on prone position, and were associated with gait ataxia and vomiting. A brain magnetic resonance imaging (MRI) showed a fourth ventricle cyst, with an eccentric enhancing nodule compatible with a larvae scolex and associated obstructive hydrocephalus. The patient was positioned prone and underwent a microsurgical resection of the cyst without rupture through a telovelar approach to the fourth ventricle. The postoperative MRI confirmed complete cyst removal and resolution of the hydrocephalus. At 12-month follow-up, the patient remains with no signs of disease recurrence.
Conclusion: In this report, we depict a case of intraventricular NCC successfully treated with a single surgery, allowing intact cyst removal and achieving effective hydrocephalus treatment with no need to resort to cerebrospinal fluid diversion techniques.
Keywords: Bruns’ syndrome, Hydrocephalus, Intraventricular neurocysticercosis, Telovelar approach
INTRODUCTION
Neurocysticercosis (NCC) is the most common helminthic infection of the central nervous system.[
The disease is endemic to low-income countries where proper sanitation is unavailable. However, high-income regions are not NCC-free mainly due to immigration from endemic areas.[
CASE REPORT
A 39-year-old woman from Cape Verde was referred to the emergency department with severe headaches triggered by head movements, gait ataxia, and vomiting. The clinical picture had a protracted course and had been worsening in the past few months. Neurological and laboratorial evaluation was unremarkable.
The brain magnetic resonance imaging (MRI) showed a fourth ventricle cyst, 2.6 × 1.8 cm (cephalocaudal × transverse axis) with an enhancing nodule compatible with a scolex and associated obstructive hydrocephalus [
We devised a surgical approach to achieve both cyst removal and hydrocephalus treatment. The patient was placed in the prone position with the head supported by a three-point head holder. The fourth ventricle was accessed through a median suboccipital craniotomy and telovelar approach [
The postoperative period was uneventful and the patient was discharged to the ward from intensive care in the first 24 h. Postoperatively, she fully recovered from the presenting symptoms over 72 h. MRI showed complete cyst removal and no complications [
The patient repeated an MRI at 1-, 6-, and 12-month follow-up with no signs of recurrence.
DISCUSSION
Extraparenchymal NCC is associated with high mortality due to hydrocephalus.[
In 12% of patients, the disease presents with hydrocephalus, caused by blockage of CSF flow through the ventricles, occlusion of foramina of Magendie and Luschka, or inflammatory reaction causing aqueduct stenosis.[
Differential diagnoses of intraventricular cystic lesions comprise infectious, neoplastic, and nonneoplastic cysts.[
Therapeutic approaches include surgery and medical treatment (corticosteroids and antihelminthics).[
The medical treatment for intraventricular NCC remains controversial. Antihelminthics are recommended in parenchymal NCC but have no clear benefits in intraventricular NCC when surgery is feasible with intact cyst removal.[
CONCLUSION
Intraventricular NCC remains a surgically treated disease. Herein, we depicted a case of a patient presenting with an unusual type of obstructive hydrocephalus – Bruns’ syndrome. In this case, the cyst location at the fourth ventricle strategically blocked CSF flow and its removal resolved the hydrocephalus. The patient was successfully treated with a single surgical approach and a ventriculoperitoneal shunt placement was avoided.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Campbell BR, Reynoso D, White AC. Intraventricular neurocysticercosis and Bruns’ syndrome: A review. J Rare Dis Res Treat. 2017. 2: 1-5
2. Carpio A, Santillán F, León P, Flores C, Hauser WA. Is the course of NCC modified by treatment with antihelminthic agents?. Arch Intern Med. 1995. 155: 1982-8
3. Del Brutto O. Diagnostic criteria for neurocysticercosis, revisited. Pathog Glob Health. 2012. 106: 299-304
4. Garcia H, Nash T, Del Brutto O. Clinical symptoms, diagnosis, and treatment of neurocysticercosis. Lancet Neurol. 2014. 13: 1202-15
5. Garcia H. Neurocysticercosis. Neurol Clin. 2018. 36: 851-64
6. Goel R, Ahmad FU, Vellimana AK, Suri A, Chandra PS, Kumar R. Endoscopic management of intraventricular neurocysticercosis. J Clin Neurosci. 2008. 15: 1096-101
7. Gripper L, Welburn S. Neurocysticercosis infection and disease a review. Acta Trop. 2017. 166: 218-24
8. Krasnianski M, Müller T, Stock K, Zierz S. Bruns syndrome caused by intraventricular tumor. Eur J Med Res. 2008. 13: 179-81
9. Lobato R, Lamas W, Portillo JM, Roger R, Esparza J, Rivas JJ. Hydrocephalus in cerebral cysticercosis. Pathogenic and therapeutic considerations. J Neurosurg. 1981. 55: 786-93
10. Mayorga-Corvacho J, Vergara-Garcia D, Riveros WM, Torres J. Tuberculoma in the fourth ventricle: An unusual location. Turk Neurosurg. 2021. 31: 658-60
11. Muly S, Liu S, Lee R, Nicolaou S, Rojas R, Khosa F. MRI of intracranial intraventricular lesions. Clin Imaging. 2018. 52: 226-39
12. Nash T, Ware JA, Mahanty S. Intraventricular neurocysticercosis: Experience and long-term outcome from a tertiary referral center in the United States. Am J Trop Med Hyg. 2018. 98: 1755-62
13. Nash TE, Garcia HH. Diagnosis and treatment of neurocysticercosis. Nat Rev Neurol. 2011. 7: 584-94
14. Raibagkar P, Berkowitz A. The many faces of neurocysticercosis. J Neurol Sci. 2018. 390: 75-6
15. Rangel-Castilla L, Serpa JA, Gopinath SP, Graviss EA, Diaz-Marchan P, White AC. Contemporary neurosurgical approaches to neurocysticercosis. Am J Trop Med Hyg. 2009. 80: 373-8
16. Roman RA, Soto-Hernandez JL, Sotelo J. Effects of prednisone on ventriculoperitoneal shunt function in hydrocephalus secondary to cysticercosis: A preliminary study. J Neurosurg. 1996. 84: 629-33
17. Shahani L, Garnes ND, Mejia R. Intraventricular Taenia solium cysts presenting with Bruns’ syndrome and indications for emergent neurosurgery. Am J Trop Med Hyg. 2015. 92: 1261-4
18. Sinha S, Sharma BS. Intraventricular neurocysticercosis: A review of current status and management issues. Br J Neurosurg. 2012. 26: 305-9
19. Westermaier T, Vince GH, Meinhardt M, Monoranu C, Roosen K, Matthies C. Arachnoid cysts of the fourth ventricle short illustrated review. Acta Neurochir (Wien). 2010. 152: 119-24
20. White AC, Coyle CM, Rajshekhar V, Singh G, Hauser WA, Mohanty A. Diagnosis and treatment of neurocysticercosis: 2017 clinical practice guidelines by the IDSA and the ASTMH. Am J Trop Med Hyg. 2018. 98: 945-66
21. Yilmazlar S, Aksoy K. Approach via the floor of the fourth ventricle for hydatid cyst of the pons. Pediatr Neurosurg. 1999. 31: 326-9