- Department of Radiology, The Aga Khan University Hospital, Karachi, Pakistan
Correspondence Address:
Ashok Kumar, Department of Radiology, The Aga Khan University Hospital, Karachi, Pakistan.
DOI:10.25259/SNI_1021_2024
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ashok Kumar, Shayan Sirat Maheen Anwar, Khawar Bilal, Anwar Ahmed, Saira Samnani, Burhan Zafar. Frequency of trigeminal neurovascular contacts identified on 3D-fast imaging employing steady-state acquisition magnetic resonance imaging in asymptomatic adults. 31-Jan-2025;16:31
How to cite this URL: Ashok Kumar, Shayan Sirat Maheen Anwar, Khawar Bilal, Anwar Ahmed, Saira Samnani, Burhan Zafar. Frequency of trigeminal neurovascular contacts identified on 3D-fast imaging employing steady-state acquisition magnetic resonance imaging in asymptomatic adults. 31-Jan-2025;16:31. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13354
Abstract
Background: Neurovascular conflict is considered one of the main causes of Trigeminal neuralgia, and 3D fast imaging employing steady-state acquisition magnetic resonance imaging (MRI) is the diagnostic imaging of choice. However, no tool is available to confirm imaging findings as the primary cause of trigeminal neuralgia because neurovascular contact is frequently found in asymptomatic individuals, according to some literature, although very little data is available till now. Therefore, we aim to determine the frequency of trigeminal neurovascular contact, involved nerve segment, culprit vessel, and characteristics of contacts in asymptomatic individuals. Knowledge about this is very crucial so that every patient may not be labeled as having neurovascular conflict as the primary cause and can be saved from unnecessary surgeries.
Methods: A retrospective observational study was conducted on 105 MRI brain scans of asymptomatic individuals for trigeminal neurovascular relationships by two expert neuro-radiologists. Percentages calculated for categorical variables and for continuous variables Shapiro–Wilk test were used. The Fisher Exact test is used to assess the association between conflict and other variables. Inter-rater reliability was computed for the outcome and other variables and Cohen’s kappa to evaluate the strength of agreement. All calculations were performed using STATA version 17.0.
Results: Out of 105 cases, neuro-vascular contact was identified in 64 cases. The most common contacting vessel was the superior cerebellar artery. The most common nerve segment involved was the cisternal segment, followed by the Root entry zone and porous trigeminus. In about 54 cases, the vessel was abutting the nerve, while in eight cases, it was compressing and, in two cases, displacing the nerve. The superior surface of the nerve was commonly involved. The inter-rater reliability between both neuroradiologists showed significant agreement.
Conclusion: Neurovascular contact is found in asymptomatic individuals, so just the presence of contact in symptomatic individuals on MRI should not be considered as only the cause of trigeminal neuralgia. It is important to identify nerve thinning and distortion, which are more reliable signs.
Keywords: 3D-constructive interference in steady state, 3D-fast imaging employing steady-state acquisition magnetic resonance imaging, Magnetic resonance image, Neurovascular conflict, Trigeminal neuralgia
INTRODUCTION
Trigeminal neuralgia is sudden, severe, paroxysmal, and recurrent neuropathic pain affecting the sensory supply of one or more branches of the trigeminal nerve. Vascular compression is considered one of the most common causes of refractory Trigeminal neuralgia.[
Microvascular decompression is the most widely used surgical intervention for neurovascular conflicts.[
Magnetic resonance image (MRI) with high-resolution three-dimensional fast imaging employing steady-state acquisition (FIESTA) sequence or constructive interference in steady state (CISS) sequence is considered as diagnostic imaging of choice to determine neurovascular conflict.[
MATERIALS AND METHODS
A retrospective observational study was conducted, and about 105 MRI brain scans containing complimentary FIESTA sequences were selected from an institutional database, which was done for some other reason, that is, persistent frontal or occipital headache, vertigo, dizziness, and tinnitus but without any complaint of facial pain or trigeminal neuralgia. This was a retrospective study and did not involve the patient directly, so patient’s consent was not required, and an Ethical Review Committee exemption certificate was also taken. These scans were reviewed for relationships of vascular structures with Trigeminal nerves by two expert neuro-radiologists with 5 years of experience in neuroradiology.
Inclusion criteria
All the patients undergoing an MRI brain with FIESTA sequence for reasons other than trigeminal neuralgia will be included in the study.
Exclusion criteria
Patients have cerebellopontine (CP) angle tumor Patients who underwent surgery for trigeminal neuralgia Age <18 years or more than 80 years.
Imaging acquisition techniques
All patients were scanned on a 1.5 Tesla general electric (GE) MRI machine, with the 3D FIESTA sequence acquired in axial sections using the following parameters: Matrix 320 × 320, slice thickness 0.8 mm, time to echo (TE) 2.47 ms, repetition time (TR) 6.5 ms, and number of excitations (NEX) 1.73. The images were subsequently reviewed on the departmental AGFA picture archiving and communication system (PACS) using the Multi-Planar Reconstruction technique. This allowed for the reconstruction of images in sagittal and coronal views and enabled adjustment of the angle as needed to clearly assess the course of the trigeminal nerve [
Image analysis
All images were reviewed by two neuroradiologists, each with at least 5 years of experience. Only cases with consensus between the two neuroradiologists were considered to have neurovascular contact. When a contact was identified between the trigeminal nerve and a vessel, the following details were recorded on an Excel data sheet: Patient’s side (left or right), type of vessel (artery or vein), surface of the nerve in contact (superior, inferior, lateral, or medial), segment of the nerve (at the porus trigeminus, at the cisternal segment, or the root entry zone [
The degree of compression was classified according to Sindou et al.,[
Statistical analysis
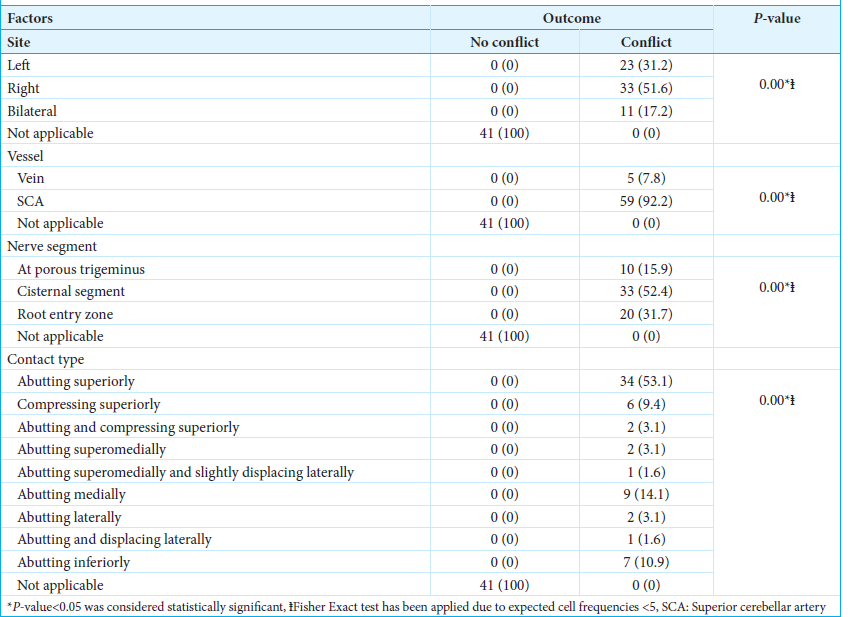
Frequencies and percentages were reported for categorical variables, including conflicts, gender, site, vessel, contact type, and nerve segment. For the continuous variable age, the Shapiro–Wilk test was used to assess the normality of the data, and the median and interquartile range (IQR) were reported due to its skewed distribution. The Fisher Exact test was employed to assess the association between conflict and other variables, as the expected cell frequencies were <5. Inter-rater reliability was computed for the outcome (conflict) and other variables, reported as percent agreement, expected agreement, and Cohen’s kappa to evaluate the strength of agreement. P < 0.05 was considered statistically significant. All calculations were performed using STATA version 17.0.
RESULTS
The study included a total of 105 patients who underwent MRI brain scans for various reasons. The median age of the patients was 55 years (IQR: 22), with 55 (59.1%) being female. A total of 105 MRI brain scans containing complementary FIESTA sequences were analyzed. Conflict was identified in 64 cases (61%) [
There was excellent agreement between both neuroradiologists regarding the presence of conflict and various factors in patients who underwent MRI brain scans, with a statistically significant P = of 0.00 for all variables, as presented in
DISCUSSION
Previous literature review shows that trigeminal neurovascular contact is common in asymptomatic individuals and increases with age due to the elongation of cisternal portions of arteries. Peker et al.[
Klun and Prestor assessed neurovascular relationships in the root entry zone of trigeminal nerves of 65 cadavers and found 52 examples of vascular contact with or without compression of the trigeminal nerve and concluded that vascular compression of the trigeminal root entry zone may be the predominant cause, but not the sole cause of trigeminal neuralgia.[
Maurya et al. observed contact between trigeminal nerve and vessel in 41 (80.4%) symptomatic individuals (Significant P < 0.001), but neurovascular contact was also seen in 17 (28.3%) asymptomatic individuals, so they concluded that just the presence of neurovascular contact is not sufficient to say that there is a conflict between offending vessel and nerve.[
The most common vessel that contacts the trigeminal nerve is the superior cerebellar artery, followed by the anterior inferior cerebellar artery. Yoshino et al,[
Miller et al.,[
Maarbjerg et al.,[
Hence, our study and literature review suggest that neuroradiologists must differentiate between just neurovascular contacts from a true neurovascular conflict while evaluating MRI of trigeminal neuralgia patients. This will help the neurosurgeons to opt for unnecessary surgeries and proceed with medical management.
Limitations
This study has several limitations. Its retrospective design and reliance on single-center data may limit the generalizability of the findings. In addition, we lacked follow-up information on the included patients to determine whether anyone developed symptoms of trigeminal neuralgia over time, so a prospective study is also required in which patients are followed with a detailed questionnaire.
CONCLUSION
Neurovascular contacts can be found frequently in asymptomatic individuals, as shown by our study and other literature reviews. Just the presence of neurovascular contact in a symptomatic individual on MRI should not be considered the only cause of trigeminal neuralgia. It is important to identify the thinning and distortion of the nerve by the vessel as these are more reliable signs of a conflict between the vessel and the nerve. This will help prevent unnecessary microvascular decompression and its complications.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study as it is retrospective study.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ahmad HS, Blue R, Ajmera S, Heman-Ackah S, Spadola M, Lazor JW. The influence of radiologist practice setting on identification of vascular compression from magnetic resonance imaging in trigeminal neuralgia. World Neurosurg. 2023. 171: e398-403
2. Anwar HA, Ramya Krishna M, Sadiq S, Ramesh Kumar R, Venkatarathnam V, Saikiran G. A study to evaluate neurovascular conflict of trigeminal nerve in trigeminal neuralgia patients with the help of 1.5 T MR imaging. Egypt J Radiol Nucl Med. 2022. 53: 66
3. Bora N, Parihar P, Raj N, Shetty N, Nunna B. A Systematic review of the role of magnetic resonance imaging in the diagnosis and detection of neurovascular conflict in patients with trigeminal neuralgia. Cureus. 2023. 15: e44614
4. Cavusoglu M, Cılız DS, Duran S, Ozsoy A, Elverici E, Karaoglanoglu R. Temporal bone MRI with 3D-FIESTA in the evaluation of facial and audiovestibular dysfunction. Diagn Interv Imaging. 2016. 97: 863-9
5. Darrow DP, Mulford KL, Quinn C, Spano A, Nixdorf DR, Grande A. The practical limits of high-quality magnetic resonance imaging for the diagnosis and classification of trigeminal neuralgia. Clin Neurol Neurosurg. 2022. 221: 107403
6. Gardner WJ. Concerning the mechanism of trigeminal neuralgia and hemifacial spasm. J Neurosurg. 1962. 19: 947-58
7. Haines SJ, Jannetta PJ, Zorub DS. Microvascular relations of the trigeminal nerve: An anatomical study with clinical correlation. J Neurosurg. 1980. 52: 381-6
8. Hardy DG, Rhoton AL. Microsurgical relationships of the superior cerebellar artery and the trigeminal nerve. J Neurosurg. 1978. 49: 669-78
9. Hitchon PW, Bathla G, Moritani T, Holland MT, Noeller J, Nourski KV. Predictability of vascular conflict by MRI in trigeminal neuralgia. Clin Neurol Neurosurg. 2019. 182: 171-6
10. Hughes MA, Frederickson AM, Branstetter BF, Zhu X, Sekula RF. MRI of the trigeminal nerve in patients with trigeminal neuralgia secondary to vascular compression. AJR Am J Roentgenol. 2016. 206: 595-600
11. Jannetta PJ. Arterial compression of the trigeminal nerve at the pons in patients with trigeminal neuralgia. J Neurosurg. 1967. 26: 159-62
12. Klun B, Prestor B. Microvascular relations of the trigeminal nerve: an anatomical study. Neurosurgery. 1986. 19: 535-9
13. Leal PR, Hermier M, Froment JC, Souza MA, Cristino-Filho G, Sindou M. Preoperative demonstration of the neurovascular compression characteristics with special emphasis on the degree of compression, using high-resolution magnetic resonance imaging: a prospective study, with comparison to surgical findings, in 100 consecutive patients who underwent microvascular decompression for trigeminal neuralgia. Acta Neurochir (Wien). 2010. 152: 817-25
14. Lin W, Chen YL, Zhang QW. Vascular compression of the trigeminal nerve in asymptomatic individuals: A voxel-wise analysis of axial and radial diffusivity. Acta Neurochir (Wien). 2014. 156: 577-80
15. Maarbjerg S, Wolfram F, Gozalov A, Olesen J, Bendtsen L. Association between neurovascular contact and clinical characteristics in classical trigeminal neuralgia: A prospective clinical study using 3.0 Tesla MRI. Cephalalgia. 2015. 35: 1077-84
16. Maurya V, Sreedhar CM, Khera A, Bhatia M, Sharma V. Trigeminal neuralgia: When does neurovascular contact turn into a conflict?. Med J Armed Forces India. 2019. 75: 134-9
17. Meaney JF, Eldridge PR, Dunn LT, Nixon TE, Whitehouse GH, Miles JB. Demonstration of neurovascular compression in trigeminal neuralgia with magnetic resonance imaging. Comparison with surgical findings in 52 consecutive operative cases. J Neurosurg. 1995. 83: 799-805
18. Miller JP, Acar F, Hamilton BE, Burchiel KJ. Radiographic evaluation of trigeminal neurovascular compression in patients with and without trigeminal neuralgia. J Neurosurg. 2009. 110: 627-32
19. Mooney J, Erickson N, Pittman B, Agee BS, Guthrie BL. The use of MRI in Preoperative decision-making for trigeminal neuralgia: A single-center study. World Neurosurg. 2021. 146: e651-7
20. Panczykowski DM, Frederickson AM, Hughes MA, Oskin JE, Stevens DR, Sekula RF. A Blinded, case-control trial assessing the value of steady state free precession magnetic resonance imaging in the diagnosis of trigeminal neuralgia. World Neurosurg. 2016. 89: 427-33
21. Peker S, Dinçer A, Necmettin Pamir M. Vascular compression of the trigeminal nerve is a frequent finding in asymptomatic individuals: 3-T MR imaging of 200 trigeminal nerves using 3D CISS sequences. Acta Neurochir (Wien). 2009. 151: 1081-8
22. Rasche D, Kress B, Stippich C, Nennig E, Sartor K, Tronnier VM. Volumetric measurement of the pontomesencephalic cistern in patients with trigeminal neuralgia and healthy controls. Neurosurgery. 2006. 59: 614-20
23. Ruiz-Juretschke F, González-Quarante LH, García-Leal R, Martínez de Vega V. Neurovascular relations of the trigeminal nerve in asymptomatic individuals studied with high-resolution three-dimensional magnetic resonance imaging. Anat Rec (Hoboken). 2019. 302: 639-45
24. Sindou M, Howeidy T, Acevedo G. Anatomical observations during microvascular decompression for idiopathic trigeminal neuralgia (with correlations between topography of pain and site of the neurovascular conflict). Prospective study in a series of 579 patients. Acta Neurochir (Wien). 2002. 144: 1-3
25. Yoshino N, Akimoto H, Yamada I, Nagaoka T, Tetsumura A, Kurabayashi T. Trigeminal neuralgia: Evaluation of neuralgic manifestation and site of neurovascular compression with 3D CISS MR imaging and MR angiography. Radiology. 2003. 228: 539-45
26. Zhou Q, Liu ZL, Qu CC, Ni SL, Xue F, Zeng QS. Preoperative demonstration of neurovascular relationship in trigeminal neuralgia by using 3D FIESTA sequence. Magn Reson Imaging. 2012. 30: 666-71