- Faculty of Medicine, Universidad del Norte, Barranquilla, Colombia
- Faculty of Medicine, Universidad de los Andes, Colombia
- Department of Neurosurgery, Fundación Santa Fe de Bogotá, Bogotá, Colombia
Correspondence Address:
Raul Fernando Vega Alvear, Faculty of Medicine, Universidad del Norte, Barranquilla, Colombia.
DOI:10.25259/SNI_52_2025
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Raul F. Vega-Alvear1, Luisa F. Fonseca Perea2, Juan Armando Mejia3, Juan F. Ramón3. Gerstmann syndrome as a sequela of a brain abscess in a non-dominant hemisphere: A case report. 28-Mar-2025;16:107
How to cite this URL: Raul F. Vega-Alvear1, Luisa F. Fonseca Perea2, Juan Armando Mejia3, Juan F. Ramón3. Gerstmann syndrome as a sequela of a brain abscess in a non-dominant hemisphere: A case report. 28-Mar-2025;16:107. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13468
Abstract
BackgroundBrain abscesses often present with headache, altered state of consciousness, and/or fever. Depending on their location, they may present with other clinical manifestations. Gerstmann syndrome, characterized by acalculia, agraphia, digital agnosia, and right-left confusion, occurs classically with lesions of the dominant parietal lobe.
Case DescriptionA 50-year-old immunocompetent female presented to the emergency department with seizures, headaches, and visual hallucinations. Brain magnetic resonance imaging revealed a right space-occupying lesion causing a mass effect consistent with a brain abscess. The patient was promptly started on ceftriaxone and metronidazole, followed by successful surgical drainage of the abscess. Cultures confirmed an infection with Streptococcus intermedius. During follow-up, the patient exhibited symptoms of acalculia, agraphia, digital agnosia, and right-left confusion, consistent with Gerstmann syndrome, attributed to significant postoperative edema. Although these cognitive sequelae showed partial improvement over time, they substantially impacted the patient’s functional abilities and psychological well-being.
ConclusionGerstmann syndrome is traditionally associated with lesions in the left angular gyrus. However, in our case, the lesion was located on the right side. Interestingly, there is only one other documented case of Gerstmann syndrome linked to a brain infection in the medical literature. Furthermore, our patient presented without the typical risk factors for brain abscesses, such as immunosuppression, an identifiable infectious source, or epidemiological connections commonly associated with this pathogen. This case highlights a rare and impactful condition, significantly affecting the patient’s quality of life while also contributing valuable insights to the understanding of this uncommon neurological syndrome.
Keywords: Brain abscess, Case report, Focal epilepsy, Gerstmann syndrome, Streptococcus intermedius
INTRODUCTION
Brain abscesses have an incidence of 0.4–0.9 cases/100,000 people and can be caused by bacteria, mycobacteria, fungi, or parasites. Their clinical presentation is often nonspecific, with common symptoms including headache, altered consciousness, and fever. However, depending on the location of the abscess, symptoms can vary – such as behavioral changes often observed in abscesses affecting the frontal lobe.[
Gerstmann syndrome is a rare neurological disorder marked by four key symptoms: acalculia, agraphia, digital agnosia, and right-left confusion. While it is most associated with vascular pathologies, the syndrome typically results from damage to the dominant parietal lobe. However, cases involving lesions in other brain regions have also been reported.[
CASE DESCRIPTION
A 50-year-old, right-handed female patient, a pharmaceutical chemist and researcher, with a medical history of bipolar disorder type I (managed with valproic acid and quetiapine), antiphospholipid syndrome, and migraine, was admitted to the emergency department after being referred from another facility. She had experienced two focal-onset seizures, which evolved into tonic-clonic generalization, along with a right temporal headache and occasional visual hallucinations. Neurological examination revealed generalized hyperreflexia and bilateral extensor plantar response, with no additional abnormalities. An external cerebrospinal fluid study yielded normal results, while a brain magnetic resonance imaging (MRI) showed a right parietal corticosubcortical space-occupying lesion, suggesting differential diagnoses such as brain abscess, neurocysticercosis or an oncological mass.
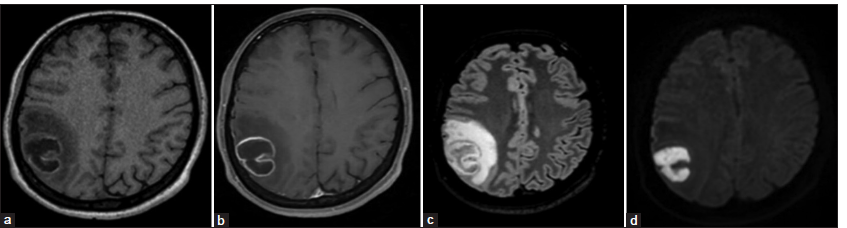
Empirical antibiotic therapy was initiated with ceftriaxone and metronidazole, alongside anti-seizure management using valproic acid, levetiracetam, and lacosamide. A follow-up brain MRI revealed an increase in the lesion’s size, consistent with a brain abscess causing a significant mass effect [
Figure 1:
Preoperative brain magnetic resonance imaging. (a) Non-enhanced T1 imaging showing intra-axial corticosubcortical lesion in the right parietal lobe (b) with peripheral ring enhancement after gadolinium injection. (c) The fluid-attenuated inversion recovery demonstrates a hyperintense lesion with perilesional vasogenic edema that causes a 4 mm midline shift. (d) The diffusion-weighted imaging shows diffusion restriction, consistent with a brain abscess.
The culture of the brain abscess sample, along with blood cultures, confirmed the presence of Streptococcus intermedius. The infectious disease department recommended continuing the established antibiotic therapy. Paraclinical tests revealed mild neutrophilia, normal C-reactive protein levels, negative human immunodeficiency virus, and cysticercosis antibodies, and a normal transthoracic echocardiogram. In addition, a CT scan of the paranasal sinuses showed no abnormalities. A dental evaluation did not identify any odontogenic sources of infection. Following a favorable clinical and radiological evolution postoperatively, the patient was discharged with anti-seizure medication, home hospitalization to complete 42 days of antibiotic therapy, and referrals for physical and occupational therapy.
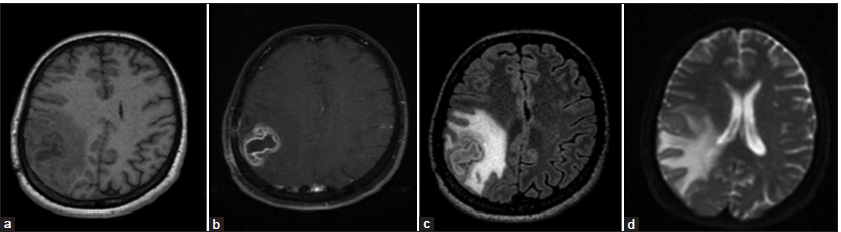
During the monthly follow-up appointment, the patient reported experiencing three seizure episodes, along with dyscalculia and agraphia, which were confirmed during the neurological examination. In addition, she exhibited signs of digital agnosia and right-left confusion, consistent with Gerstman syndrome. The patient also experienced a single episode of right facial asymmetry accompanied by a self-limiting speech arrest. A follow-up brain MRI revealed a significant reduction in the size of the abscess, although persistent vasogenic edema was observed, leading to midline deviation [
Figure 2:
1-month postoperative magnetic resonance imaging. (a) Non-enhanced T1, (b) contrast-enhanced T1, (c) fluid-attenuated inversion recovery, and (d) diffusion-weighted imaging sequences demonstrated a decrease in the size of the brain abscess, although there was an increase in perilesional edema, mass effect, and midline shift of approximately 7 mm.
Three months later, a follow-up brain MRI revealed a significant reduction in edema and mass effect [
DISCUSSION
Gerstmann syndrome, first described in 1924, is primarily recognized as a vascular condition, with an occurrence rate of approximately 1% in some studies.[
Gerstmann syndrome is thought to arise from lesions in the dominant parietal lobe, typically the left lobe in most individuals, particularly in the angular gyrus with subcortical extension. However, there is controversy regarding the exact localization of this syndrome. There are reports of unexpected localization of this clinical presentation, including subangular and middle frontal gyrus lesions.[
The clinical manifestations of brain abscesses can vary significantly based on their location. For instance, behavioral changes may arise from abscesses situated in the frontal lobe, while cranial nerve palsies can occur with brainstem abscesses and gait disorders may be seen with cerebellar abscesses. Seizures are reported in approximately one-fourth of patients. Brain abscesses often develop in individuals with predisposing factors, such as immunosuppression, damage to the brain’s protective barriers, or underlying para meningeal or systemic infections. Notably, in up to one-third of patients, no identifiable mechanisms facilitating the formation of abscesses can be determined.[
This microorganism is commonly found in dogs and cats and is recognized as a zoonotic pathogen in reported human infections. Interestingly, in 21% of cases, there was no association between animal exposure and the isolation of this pathogen, suggesting that humans may also act as carriers of this microorganism.[
The literature contains only one other case of a brain abscess located in the left parietal lobe that presented with Gerstmann syndrome. In that case, the syndrome was not isolated; it was accompanied by paresthesia, apalesthesia, kinetic apraxia in the right extremities, and ipsilateral hemiparesis that progressed to hemiplegia. The patient underwent stereotactic surgery for decompression and biopsy, which confirmed a diagnosis of tuberculous brain abscess. Although the patient experienced significant clinical improvement, he did not achieve complete remission, necessitating multimodal rehabilitation, a path also followed by our patient.[
CONCLUSION
This case highlights a rare clinical presentation in an immunocompetent patient with a parietal lobe brain abscess that resulted in Gerstmann syndrome as a neurological sequela. Although the patient experienced a partial and favorable recovery from the neurological effects, the impact on her functionality was significant. This report adds to the growing body of literature on this neurological condition, which continues to be a subject of controversy.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Altabakhi IW, Liang JW, editors. Gerstmann syndrome. Statpearls. Treasure Island, FL: StatPearls Publishing; 2023. p. Available at: https://www.ncbi.nlm.nih.gov/books/NBK519528/
2. Ardila A. Gerstmann syndrome. Curr Neurol Neurosci Rep. 2020. 20: 48
3. Brouwer MC, Tunkel AR, McKhann GM 2nd, Van De Beek D. Brain abscess. N Engl J Med. 2014. 371: 447-56
4. Issa E, Salloum T, Tokajian S. From normal flora to brain abscesses: A review of Streptococcus intermedius. Front Microbiol. 2020. 11: 826
5. Kuo CL, Lo SF, Liu CL, Chou CH, Chou LW. Effect of rehabilitation on a patient suffering from a tuberculous brain abscess with Gerstmann’s syndrome: Case report. Neuropsychiatr Dis Treat. 2012. 8: 217-20
6. Mishra AK, Fournier PE. The role of Streptococcus intermedius in brain abscess. Eur J Clin Microbiol Infect Dis. 2013. 32: 477-83
7. Nicastro N, Tafer N, Schnider A, Di Pietro M. Gerstmann’s syndrome associated with right parietal hemorrhage and arteriovenous malformation. J Clin Neurol. 2017. 13: 306-7
8. Tekgol Uzuner G, Ubur A, Erten M, Uzuner N. A rare clinical antity; Pure Gerstmann syndrome. J Stroke Cerebrovasc Dis. 2020. 29: 105161
9. Wang N, Neilan AM, Klompas M. Staphylococcus intermedius infections: Case report and literature review. Infect Dis Rep. 2013. 5: e3
10. Yoon SH, Lee JI, Kang MJ, Lee HI, Pyun SB. Gerstmann syndrome as a disconnection syndrome: A single case diffusion tensor imaging study. Brain Neurorehabil. 2023. 16: e3