- Department of Neurological Surgery, Ryofukai Satoh Neurosurgical Hospital, Fukuyama, Japan
Correspondence Address:
Toru Satoh, Department of Neurological Surgery, Ryofukai Satoh Neurosurgical Hospital, Fukuyama, Japan.
DOI:10.25259/SNI_584_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Toru Satoh. Hemodynamic analysis of a thrombosed bleb in an unruptured cerebral aneurysm. 04-Oct-2024;15:357
How to cite this URL: Toru Satoh. Hemodynamic analysis of a thrombosed bleb in an unruptured cerebral aneurysm. 04-Oct-2024;15:357. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13135
Abstract
Background: The intricate hemodynamic mechanisms of thrombosis in the bleb and/or dome of cerebral aneurysms remain unresolved. We encountered a unique case where the bleb of an unruptured internal carotid-posterior communicating artery (IC-PC) aneurysm underwent thrombosis over 7 years. Complete spontaneous thrombosis of a bleb in an unruptured cerebral aneurysm has not been previously reported. Therefore, a hemodynamic evaluation using computational fluid dynamics (CFD) analysis was conducted to examine the thrombotic development within the bleb of this aneurysm.
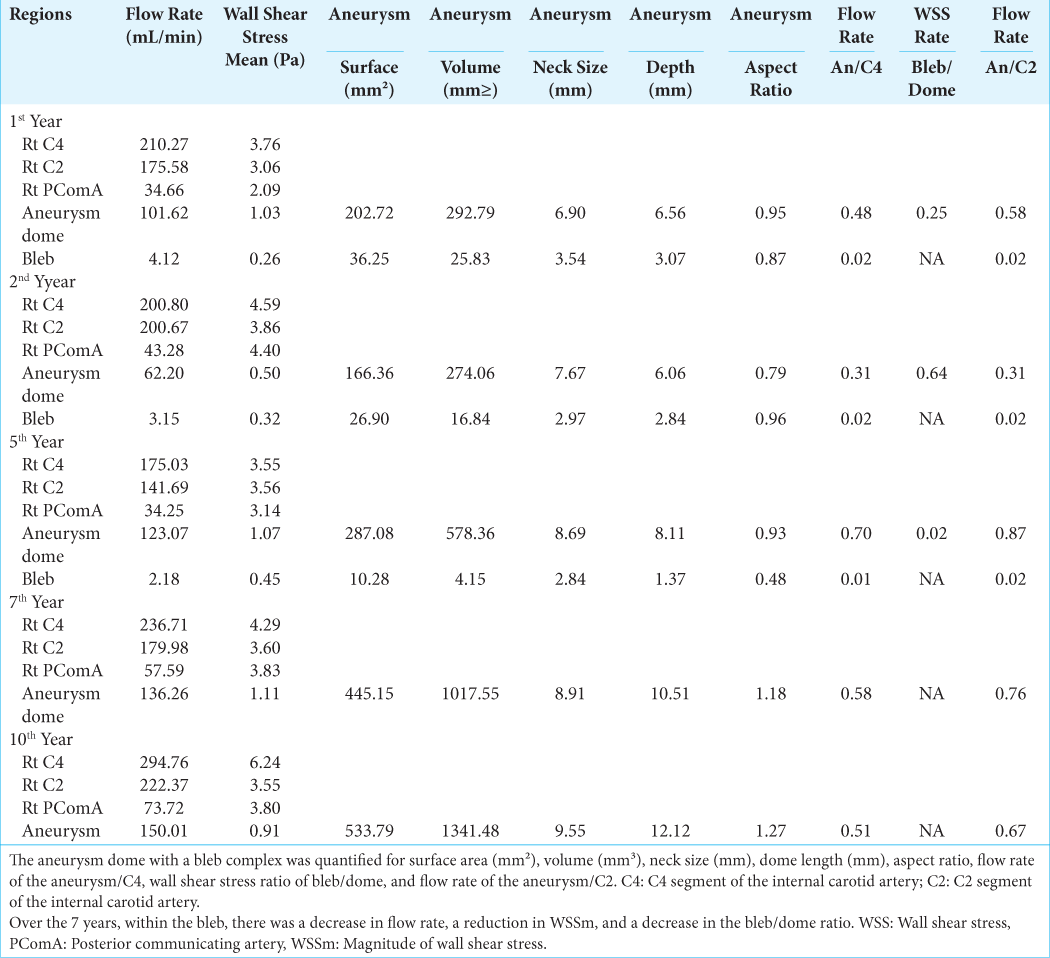
Case Description: We observed a case in which thrombosis led to the disappearance of a bleb in the dome of an unruptured IC-PC aneurysm over 7 years. CFD analysis was employed to investigate the hemodynamics of bleb thrombosis and the thrombosed bleb-neck regions of the dome in this IC-PC aneurysm. The reduction and disappearance of the bleb were associated with a decreased flow rate within the bleb, reduced magnitude of wall shear stress (WSSm), a lower WSSm ratio between the bleb and dome, increased vector direction of wall shear stress (WSSv), and discrete streamlines entering the bleb-neck region, resulting in stasis and subsequent thrombosis within the bleb. Seven years later, the dome region corresponding to the thrombosed bleb-neck exhibited localized areas with low WSSm and high WSSv along the dome wall.
Conclusion: Hemodynamically, spontaneously thrombosed bleb and thrombosed post-bleb-neck dome walls were characterized by low WSSm and high WSSv. These findings underscore the importance of CFD analysis in predicting thrombotic events in cerebral aneurysms, which can inform better clinical management strategies.
Keywords: Aneurysmal bleb, Computational fluid dynamics, Computed tomography angiography, Thrombosis, Wall shear stress
INTRODUCTION
The intricate hemodynamic mechanism underlying spontaneous thrombosis in cerebral aneurysms remains elusive.[
CASE DESCRIPTION
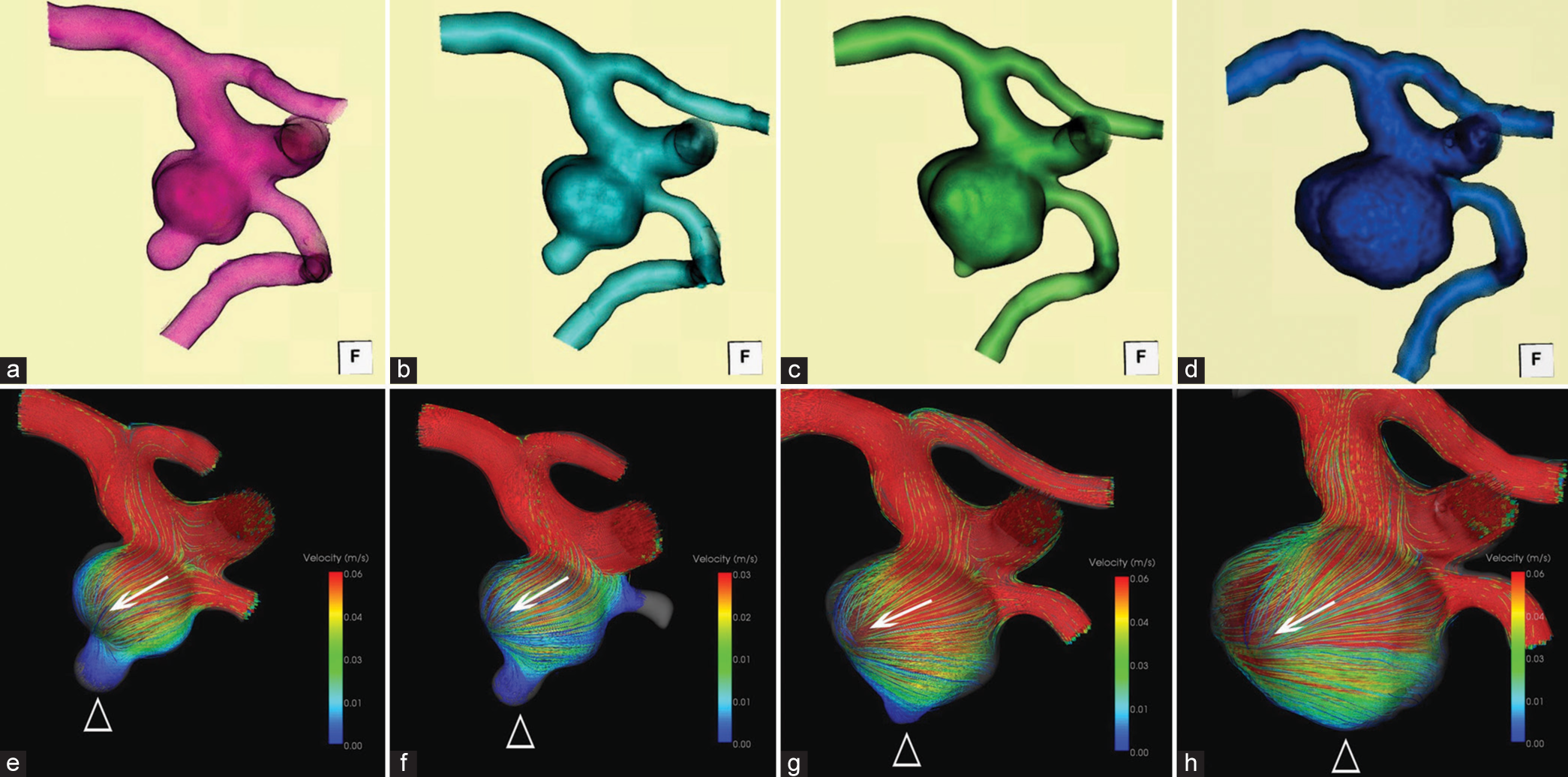
The necessary patient informed consent was obtained for this study. A female in her 70s presented with headaches and mild cognitive impairment. Computed tomography angiography (CTA) revealed an unruptured right IC-PC aneurysm with a bleb. The patient and her family opted for conservative management, avoiding aggressive treatments such as neck clipping or embolization. Instead, they focused on blood pressure management without antiplatelet treatment and underwent clinicoradiological follow-up. Over a 7-year observational period, the bleb gradually diminished and disappeared by the 7th year. The patient remained asymptomatic, with no rupture of the cerebral aneurysm, and later passed away from an unrelated condition. The morphology of the bleb and dome was sequentially reconstructed using 3D CTA obtained during the 1st, 2nd, 5th, and 7th years, all projected from similar view directions [
Figure 1:
Seven-year follow-up of 3D-CTA and hemodynamics of the right unruptured IC-PC aneurysm. The morphology of the bleb and dome was sequentially reconstructed using 3D-CTA obtained (a) at the 1st year, (b) 2nd year, (c) 5th year, and (d) 7th year, projected from similar view directions. Hemodynamics (streamline and WSS) of the aneurysm were sequentially analyzed (e) at the 1st year, (f) 2nd year, (g) 5th year, and (h) 7th year. Arrows indicate the axis of the streamline, and empty arrowheads indicate the location of the bleb.
CFD analysis
The hemodynamics of the IC-PC aneurysm were sequentially analyzed using CTA datasets obtained at the 1st, 2nd, 5th, and 7th years with a commercial CFD package (Hemoscope v1.4, EBM and AMIN Corp., Tokyo), as described. In the previous studies,[
CFD follow-up in the bleb of the dome region
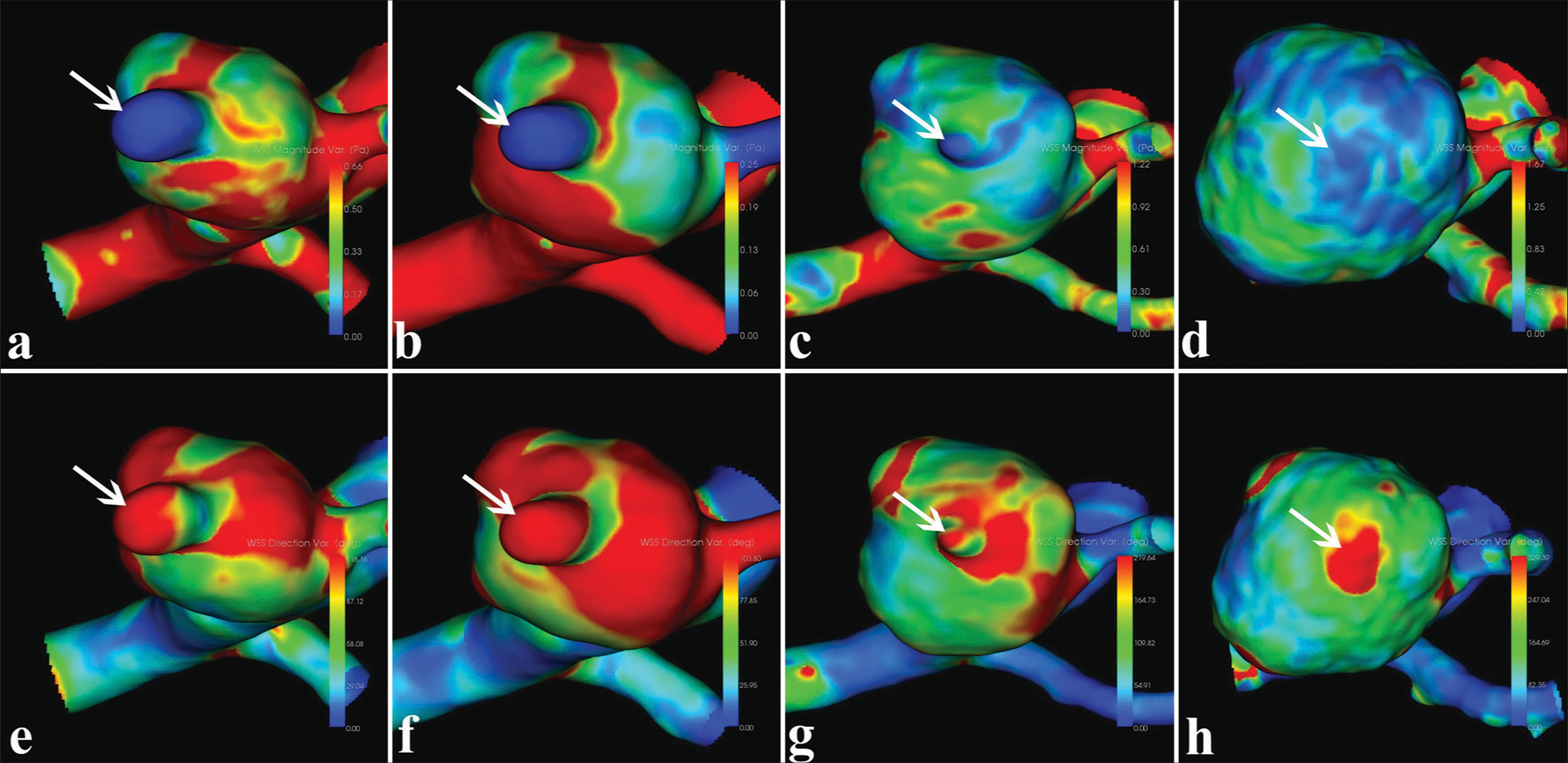
We presented a refined 7-year follow-up of hemodynamic analysis, specifically examining WSSm [
Figure 2:
Seven-year follow-up CFD analysis of WSSm and WSSv at the bleb of the right unruptured IC-PC aneurysm. (a) at the 1st year, (b) 2nd year, (c) 5th year, and (d) 7th year, respectively. Note: At the 7-year follow-up, the bleb completely disappeared due to thrombosis, but localized areas with low WSSm-variation and high WSSv-variation were observed in the dome region corresponding to the thrombosed bleb area. Arrows indicate the location of the bleb and the corresponding thrombosed bleb at the dome wall.
DISCUSSION
Thrombosis in the bleb and/or dome of cerebral aneurysms
Spontaneous thrombosis commonly occurs in the dome of ruptured cerebral aneurysms, with an incidence rate of 1–2%.[
Hemodynamic perspectives of cerebral aneurysms
Numerous studies employing CFD have investigated the occurrence and growth of cerebral aneurysms, with many reports available.[
Hemodynamic analysis of a thrombosed bleb in the presented case
In this instance, the outer surface of the aneurysmal dome extended into and impinged on the inner aspect of the temporal lobe hippocampal gyrus, where a bleb was identified. The emergence of such blebs has been linked to various factors, including intraluminal blood flow dynamics, pathological changes within the aneurysm wall, and interactions with adjacent tissues (peri-aneurysmal contact).[
Hemodynamic perspectives of the thrombosed bleb-neck region of the dome
The thrombosed bleb persists morphologically without disappearing and remains at the bleb-neck region. Hemodynamic analysis of the bleb-neck region revealed that spontaneous thrombosis and disappearance of the bleb occurred due to interruption of blood flow within the bleb, resulting in a lack of contrast enhancement observed by CTA. However, localized areas with low WSSm and high WSSv were noted in the dome region corresponding to the thrombosed bleb-neck. It is speculated that the thrombosed bleb-neck region exhibited different wall characteristics compared to the surrounding dome wall. From the hemodynamic analysis in this case, both the spontaneously thrombosed bleb and the thrombosed post-bleb-neck dome region exhibited characteristic hemodynamic findings of reduced variation in WSSm and multidirectional changes in WSSv.
CONCLUSION
CFD analysis enabled the hemodynamic evaluation of bleb thrombosis and the post-thrombosis bleb-neck dome wall. Complete thrombosis was observed in spontaneously thrombosed blebs due to stagnation of blood flow within the bleb. Localized areas with low values of WSSm and high values of WSSv were observed in dome wall regions corresponding to the thrombosed bleb-neck post-thrombosis. These findings underscore the importance of CFD analysis in predicting thrombotic events in cerebral aneurysms, which can inform better clinical management strategies.
Ethical approval
The research/study approved by the Institutional Review Board at The Institutional Review Board (IRB) of Satoh Neurosurgical Hospital, number 2024–04, dated May 03, 2024.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Boussel L, Rayz V, McCulloch C, Mertin A, Acevedo-Bolton G, Lawton M. Aneurysm growth occurs at region of low wall shear stress: Patient-specific correlation of hemodynamics and growth in a longitudinal study. Stroke. 2008. 39: 2997-3002
2. Cebral JR, Sheridan M, Putman CM. Hemodynamics and bleb formation in intracranial aneurysms. AJNR Am J Neuroradiol. 2010. 31: 304-10
3. Humphrey JD, Canham PB. Structure, mechanical properties and mechanics of intracranial saccular aneurysms. J Elast. 2000. 61: 49-81
4. Kulcsar Z, Ugron A, Marosfoi M, Berentei Z, Paal G, Szikora I. Hemodynamics of cerebral aneurysm initiation: The role of wall shear stress and spatial wall shear stress gradient. AJNR Am J Neuroradiol. 2011. 32: 587-94
5. Ngoepe MN, Frangi AF, Byrne JV, Ventikos Y. Thrombosis in cerebral aneurysms and computational modeling thereof: A review. Front Physiol. 2018. 9: 306
6. Rayz VL, Boussel L, Ge L, Leach JR, Martin AJ, Lawton MT. Flow residence time and regions of intraluminal thrombus deposition in intracranial aneurysms. Ann Biomed Eng. 2010. 38: 3058-69
7. Satoh T, Yagi T, Sawada Y, Sugiu K, Sato Y, Date I. Association of bleb formation with peri-aneurysmal contact in unruptured intracranial aneurysms. Sci Rep. 2022. 12: 6075
8. Satoh T, Sato Y, Sawada Y. Peri-aneurysmal contact as a risk factor for aneurysmal rupture in unruptured intracranial aneurysms: An overview. Med Res Arch. 2024. 12:
9. Satoh T, Sugiu K, Hiramatsu M, Haruma J, Date I. Evaluation of the shrinkage process of a neck remnant after stent-coil treatment of a cerebral aneurysm using silent magnetic resonance angiography and computational fluid dynamics analysis: Illustrative case. J Neurosurg Case Lessons. 2024. 15: CASE24141
10. Vandenbulcke A, Messerer M, Starnoni D, Puccinelli F, Daniel RT, Cossu G. Complete spontaneous thrombosis in unruptured non-giant intracranial aneurysms: A case report and systematic review. Clin Neurol Neurosurg. 2021. 200: 106319