- Department of Neurosurgery, Ibrahim Cardiac Hospital and Research Institute (A Centre for Cardiovascular, Neuroscience and Organ Transplant Units), Dhaka, Bangladesh
- Department of Orthopaedic Surgery, Bangladesh Medical University, Dhaka, Bangladesh
Correspondence Address:
Nazmin Ahmed, Department of Neurosurgery, Ibrahim Cardiac Hospital and Research Institute (A Centre for Cardiovascular, Neuroscience and Organ Transplant Units), Dhaka, Bangladesh.
DOI:10.25259/SNI_571_2025
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nazmin Ahmed1, Mohammad Nazrul Hossain1, Shahidul Islam Khan2, Md. Raad Kazi1. Hugely dilated/partially calcified epidural varicose vein caused intraspinal neural compression/sciatica. 01-Aug-2025;16:315
How to cite this URL: Nazmin Ahmed1, Mohammad Nazrul Hossain1, Shahidul Islam Khan2, Md. Raad Kazi1. Hugely dilated/partially calcified epidural varicose vein caused intraspinal neural compression/sciatica. 01-Aug-2025;16:315. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13749
Abstract
Background: A patient presented with lumbago/sciatica attributed to a magnetic resonance (MR)-documented hugely dilated, partially calcified, and extrinsically compressive epidural varicose vein (EVV).
Case Description: A 36-year-old male presented with 2 months of lumbago-sciatica; the only finding was a positive left-sided straight leg sign to 50°. The MR imaging demonstrated a hugely dilated, branching pattern flow void that caused marked displacement/compression of thecal sac and left S1 nerve root. The X-rays and computed tomography (CT) studies additionally showed a linear “string of beads” pattern of calcification at the L5/S1 level. Intraoperatively, an encapsulated, hugely dilated, compressive epidural vein was encountered; partial vein coagulation and gross total removal decompressed the neural elements. He recovered normal neurological function within 1 post-operative month.
Conclusion: A 36-year-old male presented with left-sided sciatica attributed to an MR and CT documented hugely dilated, partially calcified L5/S1 EVV. Once the EVV was coagulated and removed, the patient’s symptoms resolved.
Keywords: Disc herniation, Epidural varicose vein, Radiology
INTRODUCTION
Few studies document that an epidural varicose vein (EVV) can mimic a disc herniation, resulting in lumbar thecal sac and compression.[
CASE REPORT
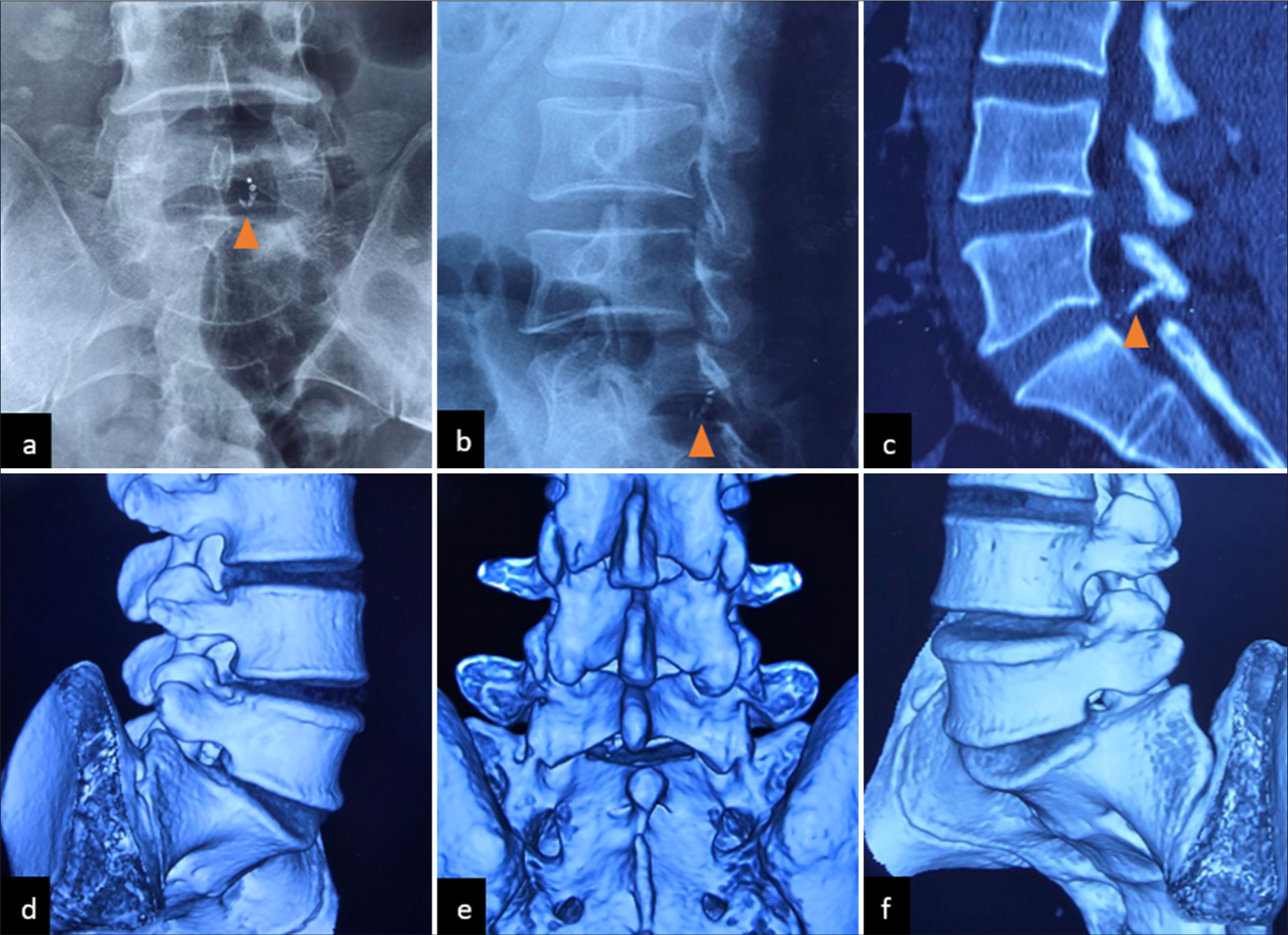
A 36-year-old male presented with left lower extremity sciatica of 2 months’ duration. His only neurological finding was a left-sided positive straight leg raising sign to 50°. The MR imaging demonstrated a hugely dilated, branching pattern flow void that caused displacement of the thecal sac, and compression of the left S1 nerve root [
Figure 1:
Magnetic resonance imaging of L/S spine, (a) T1 weighted image (T1WI), (b) T1 weighted image (T2WI) sagittal and (c) coronal section demonstrated a well-defined linear, penetrating like flow void, indenting and compressing the thecal sac from left posterolateral aspect. This flow void was surrounded by hyperintense cleft in both sequences. Mild disc herniation at L4/L5 and L5/S1 was also evident. (d) T2WI and (e and f) T1WI, axial section demonstrated a hugely dilated malformation, displacing the thecal sac and compressing the left S1 traversing nerve root.
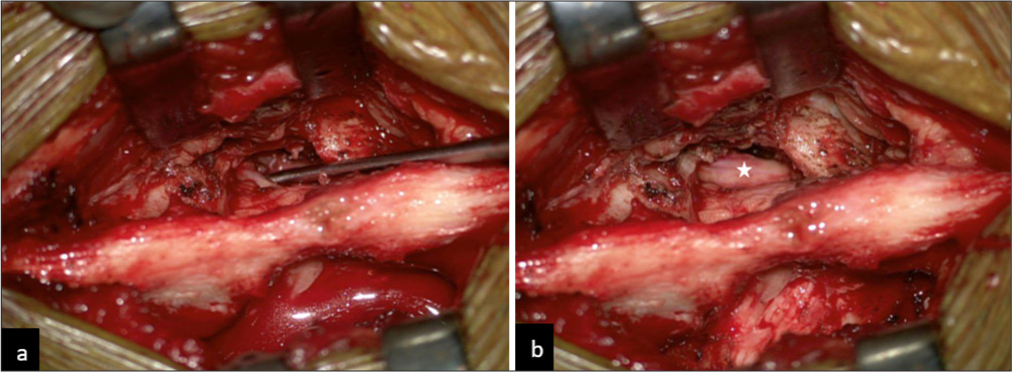
Figure 2:
X-ray, L/S spine, (a) anteroposterior and (b) oblique view demonstrated a “string of beads” pattern calcification at left L5/S1 level (marked by yellow arrowhead); (c) this calcified string seems to be adherent with inner aspect of L5 lamina (marked by yellow arrowhead); computed tomography scan of L/S spine, 3D reconstruction (d) right oblique, (e) posterior and (f) left oblique view demonstrated normal anatomical configuration of lumbosacral spine with no congenital or acquired bone abnormalities.
DISCUSSION
As the epidural venous plexus is valveless, disc herniations, spinal stenosis, tumors, abscesses, hematomas, conjoined nerve roots, and/or perineural cysts can all contribute to the development of EVVs.[
CONCLUSION
A 36-year-old male presented with 2 months of increased left lower extremity radiculopathy. Both MR and CT studies documented a hugely dilated left-sided L5/S1 EVV that, once coagulated and successfully removed, was asymptomatic.
Ethical approval:
Institutional review board approval is not required.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship:
Nil.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Ahmed N, Hossain MN, Khan SI, Kazi R. Conjoined nerve root, epidural varicose vein, and extruded lumbar disc: Triad of refractory sciatica. Surg Neurol Int. 2025. 16: 200
2. Jeong HJ, Sim WS, Park HJ, Lee SH, Oh MS, Cho MK. Severe lumbar radiculopathy with epidural venous plexus engorgement in a morbidly obese pediatric patient: A case report. Medicine (Baltimore). 2019. 98: e16842
3. Ju JH, Ha HG, Jung CK, Kim HW, Lee CY, Kim JH. Patterns of epidural venous varicosity in lumbar stenosis. Korean J Spine. 2012. 9: 244-9
4. Lee YS, Choi ES, Kim JO, Ji JH. A rare calcified thrombosis of the dilated epidural venous plexus presenting with lumbar radiculopathy: A case report. Spine J. 2011. 11: e28-31