- Department of Neurosurgery, Hull Royal Infirmary, Northern Humbershire, United Kingdom,
- Department of Neurosurgery, Liaquat National Hospital and Medical College, Karachi, Sindh, Pakistan.
- Department of Neurosurgery, Liaquat National Hospital, Karachi, Sindh, Pakistan.
Correspondence Address:
Muhammad Samir Irfan Wasi
Department of Neurosurgery, Liaquat National Hospital, Karachi, Sindh, Pakistan.
DOI:10.25259/SNI_408_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Muhammad Samir Irfan Wasi, Salman Yousuf Sharif, Farhan Gulzar. Implication of image guidance in endoscopic third ventriculostomy: Technical note. Surg Neurol Int 02-May-2020;11:87
How to cite this URL: Muhammad Samir Irfan Wasi, Salman Yousuf Sharif, Farhan Gulzar. Implication of image guidance in endoscopic third ventriculostomy: Technical note. Surg Neurol Int 02-May-2020;11:87. Available from: https://surgicalneurologyint.com/surgicalint-articles/9993/
Abstract
Background: Endoscopic third ventriculostomy (ETV) is an advanced surgical procedure and plays a major role in the management of hydrocephalus. The complications associated with this procedure are grave and unforgiving. Image guidance system (IGS) can help reduce these complications. This technical note describes the technique for utilizing image guidance in carrying out ETV with safety and efficacy.
Methods: The authors have performed ETV on more than 75 cases. We describe a step-by-step technique for the implication of image guidance while performing ETV including the trajectory planning, coregistration, approach, and third ventricular floor perforation. For illustration, we present the case of a 54-year-old female with moderate-intensity headache and central vertigo for 2 months presented with no significant findings on examination. Magnetic resonance imaging (MRI) showed dilated lateral and third ventricles with normal sized fourth ventricle. A diagnosis of aqueductal stenosis was made and ETV was performed under image guidance.
Results: Since 2012, we performed 78 cases of ETV with the help of image guidance. None of the patients had any episode of intraoperative hemorrhage. Two patients (2.56%) had fornix contusions.
Conclusion: Image guidance can help reduce complications and is becoming an essential tool in performing ETV. IGS ETV technique may benefit young neurosurgeons the most and can help them overcome the learning curve with safety.
Keywords: Basilar artery hemorrhage, Endoscopic third ventriculostomy, Fornix injury, Image guidance, Third ventricle
BACKGROUND
Endoscopic third ventriculostomy (ETV) has emerged as the latest pinnacle in the management of hydrocephalus. In this age of minimally invasive surgery, ETV offers the safest and the most productive procedure in terms of outcome for treating hydrocephalus.[
The main indication for ETV is obstructed hydrocephalus when a patient typically presents with dilated lateral and third ventricles and a normal sized fourth ventricle. The introduction of better neuroendoscopes, 3D and HD cameras, and latest imaging techniques has broadened the spectrum of indications for ETV. Nonobstructive causes for hydrocephalus, for example, normal pressure hydrocephalus, are now subjectively indicated for ETV.
Radiological indications for successful ETV include several MRI findings that can be pinned out in the sagittal films. A thinned out, bowing corpus callosum, lack of aqueductal flow void, low arching floor of third ventricle, and anteriorly bulging lamina terminalis are consistent with patients requiring ETV.[
The authors describe an image-guided technique to ensure safe and easy endoscopic access to the third ventricle to land on the foramen of Monro.
METHODS
We have performed this procedure with the help of image guidance system (IGS) in more than 75 cases since 2012. In this technical note, we describe the step-by-step technique for implicating image guidance in ETV procedure on an illustrative case. This technique would help carry out the procedure without creating an erroneous trajectory into the eloquent areas of the brain. This technique may reduce complication rates that arise as a consequence of diverging from the straight forward path to the lateral ventricle.
We describe an illustrative case of a 54-year-old patient who complained of moderate-intensity headache associated with central vertigo for 2 months. She had walking difficulty and gait disturbance. Her neurological examination was normal. MRI brain scan showed dilation of lateral and third ventricles and the fourth ventricle appears to be normal. Findings were suggestive of obstructive hydrocephalus secondary to aqueductal stenosis.
ETV was performed with image guidance [
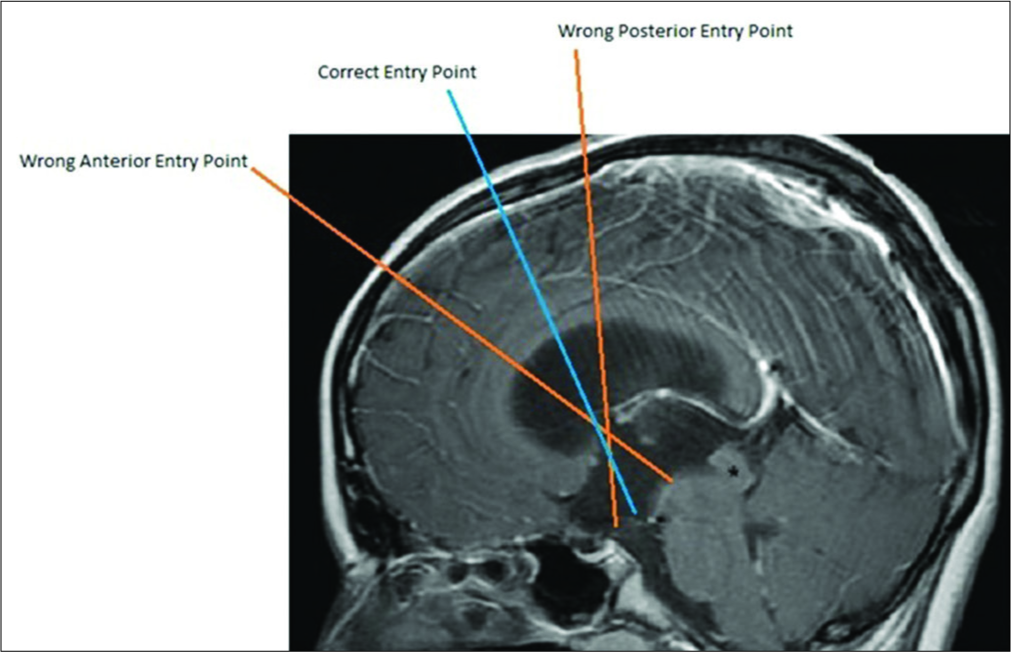
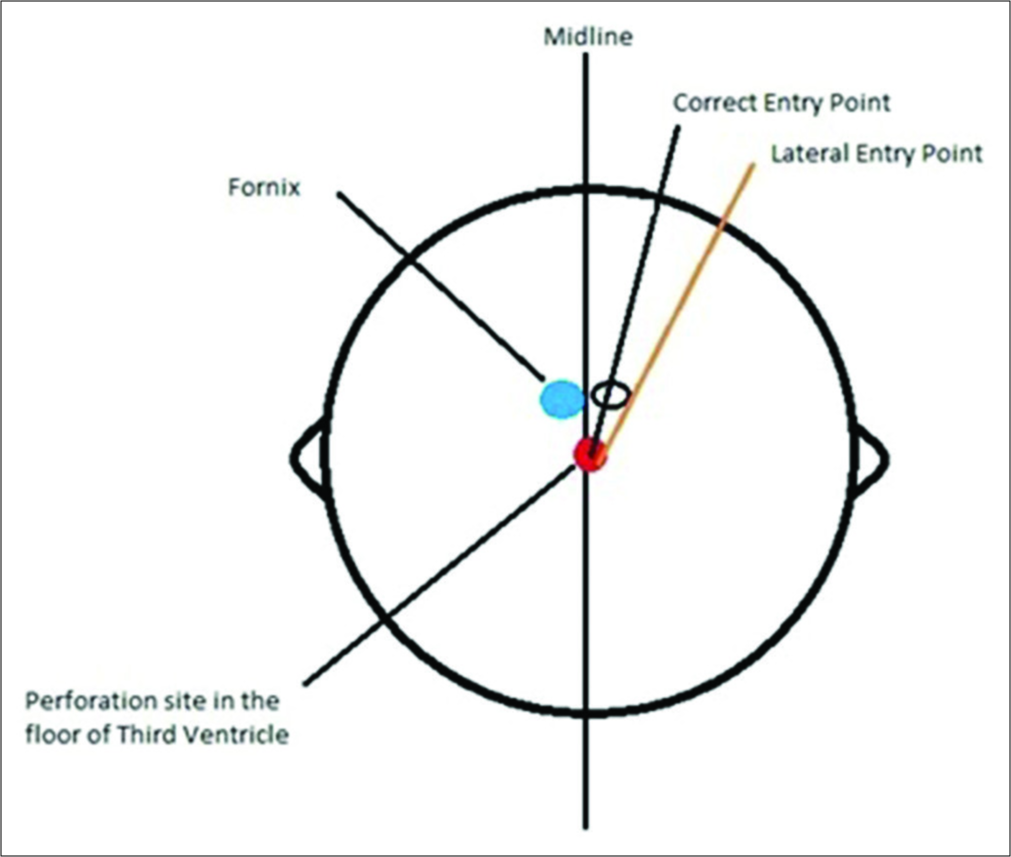
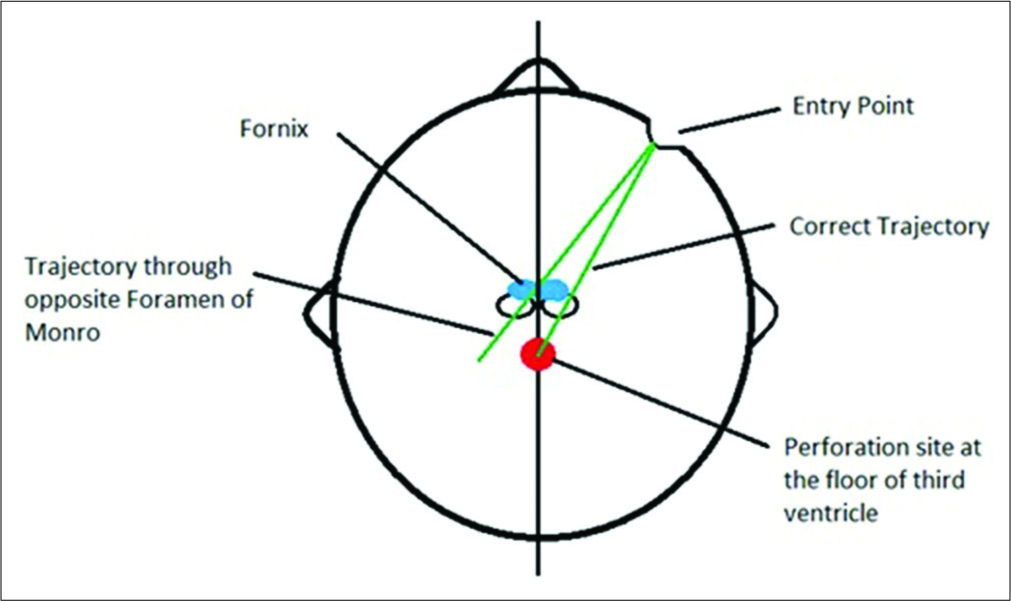
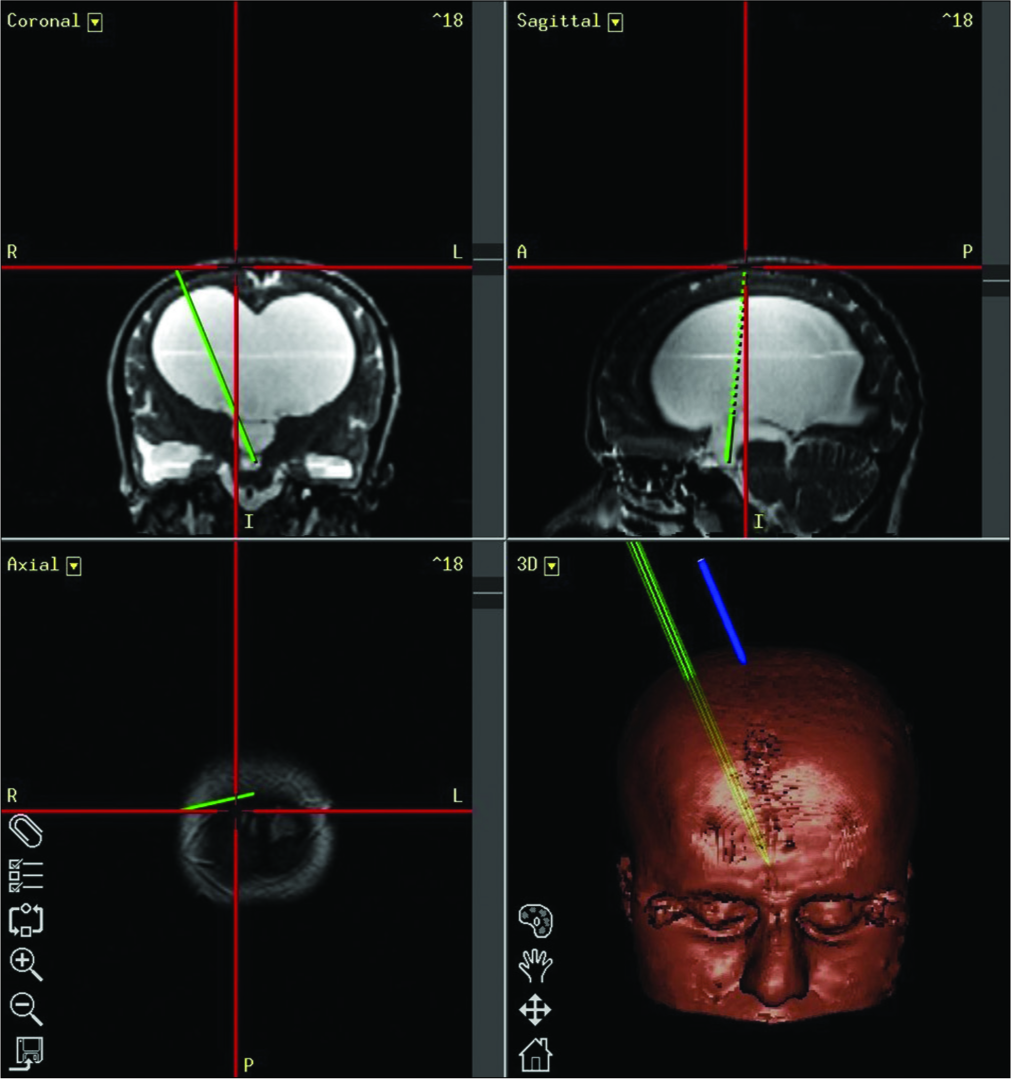
Once the three-dimensional reconstruction of the anatomy is visible on the system, a trajectory was planned on the workstation of IGS [
Figure 4:
Workstation screen of planning for image guidance system endoscopic third ventriculostomy on coronal, sagittal, and axial views. A line (plain green) is extended from mid-point of foramen of Monro to mid-point of the third ventricular floor anterior to the basilar artery. The line is then extended upward (dotted green line) toward the scalp giving us the entry point.
The patient was positioned supine on the operating table. The head of patient was slightly flexed and fixed with a Mayfield head holder. The head end was elevated to about 20–30° in a reverse Trendelenburg position.
At this point, mapping of the patient’s anatomy called “coregistration” was done by means of an optical probe. This created a map of patient’s anatomy correlating with the MR images uploaded on the IGS. Thus, whenever the optical probe was placed on any desired structure, the IGS displayed the corresponding point on MRI.
Once the coregistration was done, care was taken not to change the position of either the patient or the optical camera as this would distort the optical referencing of the anatomy. The optical probe was then attached to the endoscope to navigate the path, thus avoiding the endoscope to land at a blind end. The navigation system at this point was ready to use.
A horseshoe incision was given at the optimal entry point already defined. This helped in double breasting of the wound and avoided CSF leak. A burr hole was made and dura was cut in a cruciate fashion. An endoscope was then introduced through the burr hole following the defined trajectory. All steps of surgery were performed with image guidance to ensure avoiding damage to vital structures.
Once the endoscope has reached the lateral ventricle, we were able to identify the foramen of Monro easily along with the choroid plexus, thalamostriate, and septal veins. Fornix was seen forming the roof of the foramen. The fornix was inspected carefully revealing no signs of contusion.
The endoscope was then advanced into the foramen to enter the third ventricle and its floor was clearly visualized. The thin membrane forming the floor was punctured with the help of blunt probe and a stoma was made between the third ventricle and prepontine subarachnoid space. The endoscope was passed through the stoma into the underlying subarachnoid space and the contents including basilar artery were visualized to ensure no complication.
The fornix was inspected again as endoscope was pulled out of the foramen of Monro to exclude any injury. A piece of Gelfoam was placed at the burr hole site followed by meticulous skin closure.
RESULTS
Since 2012, we performed 78 cases of ETV with the help of image guidance. The mean age of the patients was 31.3 years. None of the patients had any episode of intraoperative hemorrhage. Two patients (2.56%) had fornix contusions. These contusions were clinically insignificant as neither of them had postoperative memory impairment which was assessed through Mini-Mental State Examination through registration recall. No other iatrogenic injury was observed in any of the patients.
DISCUSSION
Conventionally, ETV was done without image guidance. Cortical hemorrhage was a known complication when advancing endoscope through brain parenchyma. This was either due to cortical vein damage or surgeon denting lateral walls and causing ventricular bleed. This urged us to implicate image-guided navigation to help place the endoscope at our desired point.
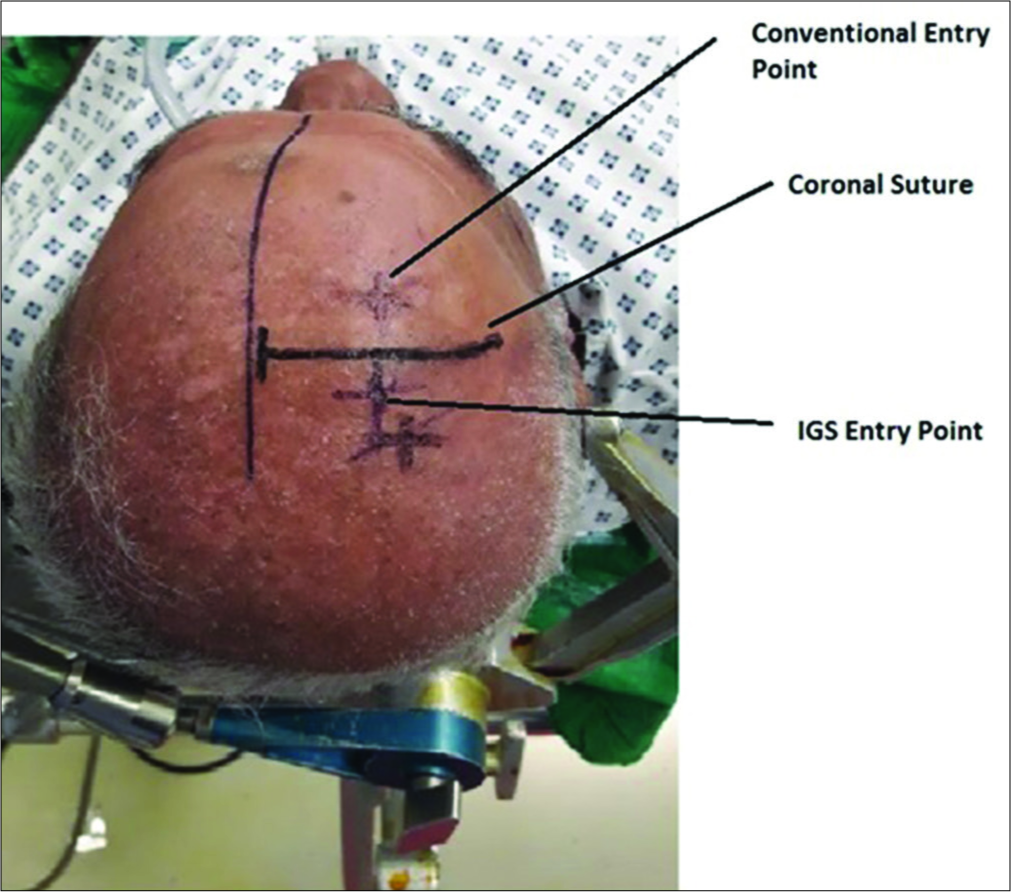
The trajectory defined by the surgeon through the image guidance helps determine the incision site. The standard practice for ETV is to put knife to skin at the Kocker’s point, lying 1 cm anterior to the coronal suture[
The introduction of endoscope poses risk of forniceal contusion and short-term memory loss could clinically be implicated in this situation. Image guidance can help reduce this complication as the surgeon can locate the position of the tip of endoscope during his maneuvers and can halt the movement of endoscope before it reaches near the fornix. Foramen of Monro should always be measured radiologically before surgery. It must be wide enough to allow the endoscope to proceed further down and reach the floor of third ventricle. This avoids iatrogenic injuries to structures forming the boundaries of the foramen.
When an endoscope is then advanced through the foramen of Monro to enter the third ventricle, the floor is clearly visualized. The thin membrane forming the floor of the third ventricle allows the structures lying underneath to be adequately visible with infundibulum anteriorly, the mammillary bodies posteriorly, and a translucent, triangular tuber cinereum in between. The most important structure to look for underneath the floor is the basilar artery and its branches because the surgeon needs to avoid them while perforating the floor. The fenestration of the floor of the third ventricle can be performed with a blunt probe, bipolar diathermy, the endoscope itself, or microscissors depending on surgeon’s choice. The puncture site is then enlarged using a 3F Fogarty catheter or microalligators. The optimal site for the ventriculostomy is the center of hypophysiomamillary triangle.
In some instances, the floor is not typically as thin as the surgeon expects. The opacity of the membrane in some cases makes the visualization of basilar artery difficult and a blind puncture at this occasion would increase the risk of hemorrhage secondary to basilar artery rupture.[
The endoscope must always be advanced through the puncture site down into the prepontine subarachnoid space to visualize the contents of the cistern. Continuous irrigation with Ringer’s lactate solution, at 37.5°C, must be done during the procedure for better visualization of structures.
CONCLUSION
We have repeatedly implicated the IGS ETV technique described above and observed reduced forniceal contusions. No cases with either hemorrhage or iatrogenic injury to other neurological structures were observed.
Young neurosurgeons can use this surgical technique to overcome the learning curve associated with the ETV. If available, Image guidance must be used in every case to avoid potential complications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos available on:
www.surgicalneurologyint.com
References
1. Dlouhy BJ, Capuano AW, Madhavan K, Torner JC, Greenlee JD. Preoperative third ventricular bowing as a predictor of endoscopic third ventriculostomy success. J Neurosurg Pediatr. 2012. 9: 182-90
2. Hingwala D, Chatterjee S, Kesavadas C, Thomas B, Kapilamoorthy TR. Applications of 3D CISS sequence for problem solving in neuroimaging. Indian J Radiol Imaging. 2011. 21: 90-7
3. Moorthy RK, Rajshekhar V. Endoscopic third ventriculostomy for hydrocephalus: A review of indications, outcomes, and complications. Neurol India. 2011. 59: 848-54
4. Ocuz C. Endoscopic third ventriculostomy: Indications, surgical technique and potential problems. Turk Neurosurg. 2002. 12: 65-73
5. Schroeder HW, Niendorf WR, Gaab MR. Complications of endoscopic third ventriculostomy. J Neurosurg. 2002. 96: 1032-40
6. Spennato P, Tazi S, Bekaert O, Cinalli G, Decq P. Endoscopic third ventriculostomy for idiopathic aqueductal stenosis. World Neurosurg. 2013. 79: e13-20
7. Stefan S, Daniel H, David MA.editors. Critical Care of the Stroke Patient. Cambridge, United Kingdom: Cambridge University Press; 2014. p. 148-