- Department of Neurosurgery, Southern TOHOKU Research Institute for Neuroscience, Yatsuyamada, Koriyama, Fukushima,
- Research Group for Kampo Medication Based on Modern Science,
- Director, Hidaka Tokushukai Hospital, Shizunai Kosei, Shin-Hidaka, Hidaka, Hokkaido, Japan.
Correspondence Address:
Yoshitaka Hirano
Department of Neurosurgery, Southern TOHOKU Research Institute for Neuroscience, Yatsuyamada, Koriyama, Fukushima,
DOI:10.25259/SNI_62_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yoshitaka Hirano, Hideya Isai, Akinori Onuki, Kazuo Watanabe. Integrative treatment of paralytic small intestine following acute cervical cord injury: A case report. 25-Apr-2020;11:80
How to cite this URL: Yoshitaka Hirano, Hideya Isai, Akinori Onuki, Kazuo Watanabe. Integrative treatment of paralytic small intestine following acute cervical cord injury: A case report. 25-Apr-2020;11:80. Available from: https://surgicalneurologyint.com/surgicalint-articles/9973/
Abstract
Background: A patient developed paralysis of the small intestine following an acute traumatic hyperextension cervical spinal cord injury attributed to the ossification of the posterior longitudinal ligament (OPLL) C3–C6. The persistent ileus finally resolved utilizing Kampo medications (traditional Chinese therapy) consisting of both bukuryoin (TJ-69) and hangekobokuto (TJ-16).
Case Description: A 63-year-old male became acutely quadriplegic secondary to a hyperextension injury incurred during a fall. Radiographic studies confirmed mixed OPLL extending from C3–C6 resulting in marked cord compression, there was a clear spinal cord contusion. His neurological status using the American Spinal Injury Association (ASIA) Scale was Grade “A;” there were was complete motor and sensory loss below the C5 level. After a C3–C6 expansive laminoplasty, the ASIA scale improved to Grade B. However, he then developed a persistent small intestine ileus resulting in marked abdominal distention. When conventional therapies failed to resolve the problem, Kampo medicines, consisting of both bukuryoin (TJ-69) and hangekobokuto (TJ-16), were administered. The ileus improved within 2 days and fully resolved within the 1st postoperative week.
Conclusion: The utilization of Kampo medications, consisting of both bukuryoin (TJ-69) and hangekobokuto (TJ-16), or the combined bukuryoingohangekobokuto (TJ-116) effectively resolved a postoperative paralytic small bowel ileus following a cervical laminoplasty performed in a quadriplegic patient.
Keywords: Acute cervical cord injury, Cervical ossification of the posterior longitudinal ligamentOPLL, Complication management, Integrative medicine, Paralytic small intestine
INTRODUCTION
A patient with underlying severe stenosis from C3 to C6 due to cervical ossification of the posterior longitudinal ligament (OPLL) sustained a traumatic hyperextension cervical cord injury due to a fall, resulting in quadriplegia. His deficit was, according to the American Spinal Injury Association (ASIA), Grade “A”; a complete sensory/motor below the C5 level. Following a C3–C6 laminoplasty, he developed a persistent small intestine ileus that failed 3 days of conventional therapy. After 7 days of Kampo therapy (e.g., traditional Chinese–Japanese medicine) consisting of both bukuryoin (TJ-69) and hangekobokuto (TJ-16), the ileus finally fully resolved.
CASE DESCRIPTION
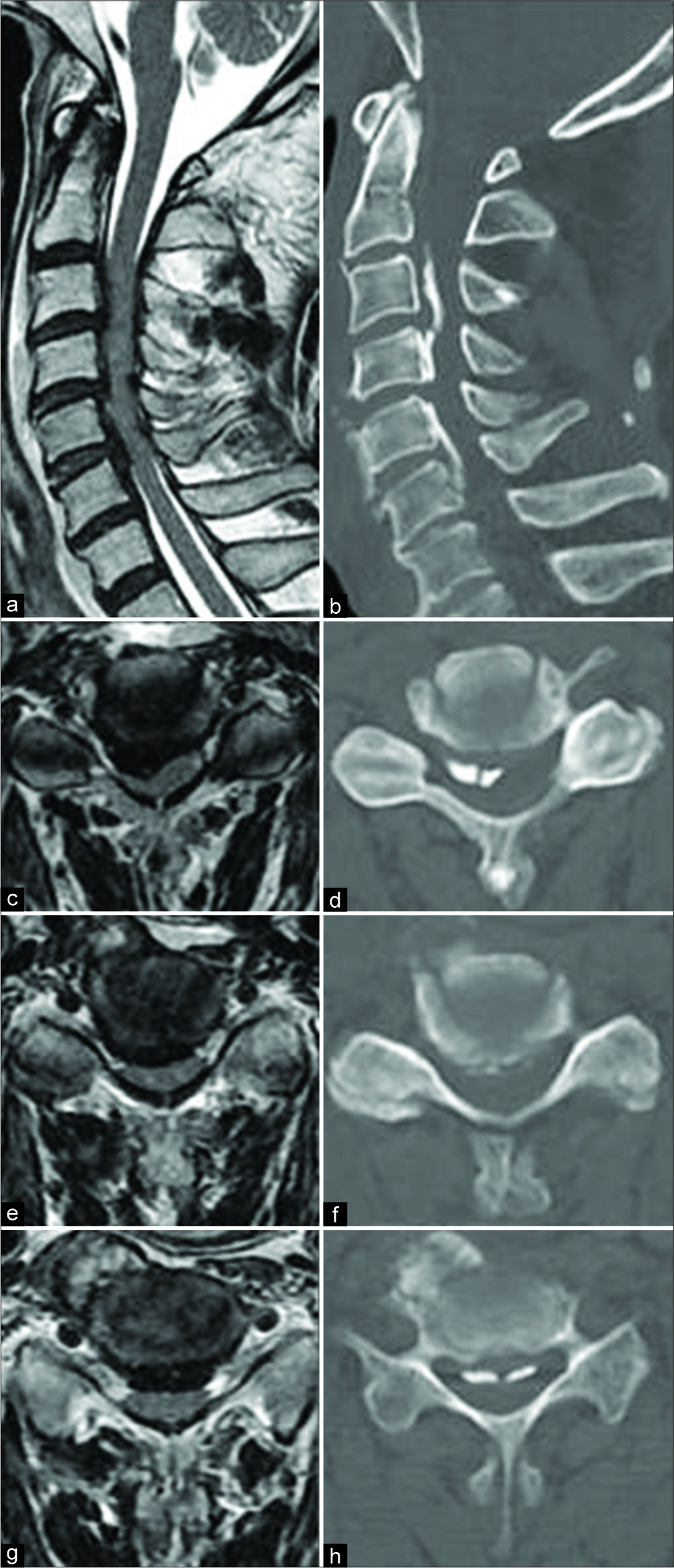
A 63-year-old male, with a history of diabetes (type 2), hypertension, hyperlipidemia, and cardiac disease, was quadriplegic after a traumatic hyperextension injury (e.g., due to a fall). He rendered immediately quadriplegic ASIA Grade “A” indicative of a complete C5 motor/sensory deficit. Radiological studies revealed cervical C3–C6 OPLL resulting in marked cervical cord compression; the T2- weighted MR images revealed a hyperintense intrinsic cord signal indicative of a spinal cord injury [
Figure 1:
T2-weighted magnetic resonance images (a-d) and computed tomography scans (e-h) of the cervical spine revealing multilevel cervical cord injury associated with ossified posterior longitudinal ligament of the mixed type. Sagittal images (a,e) were obtained on the midline, and axial images at the levels of C3–4 (b,f), C4–5 (c, g), and C5–6 (d,h).
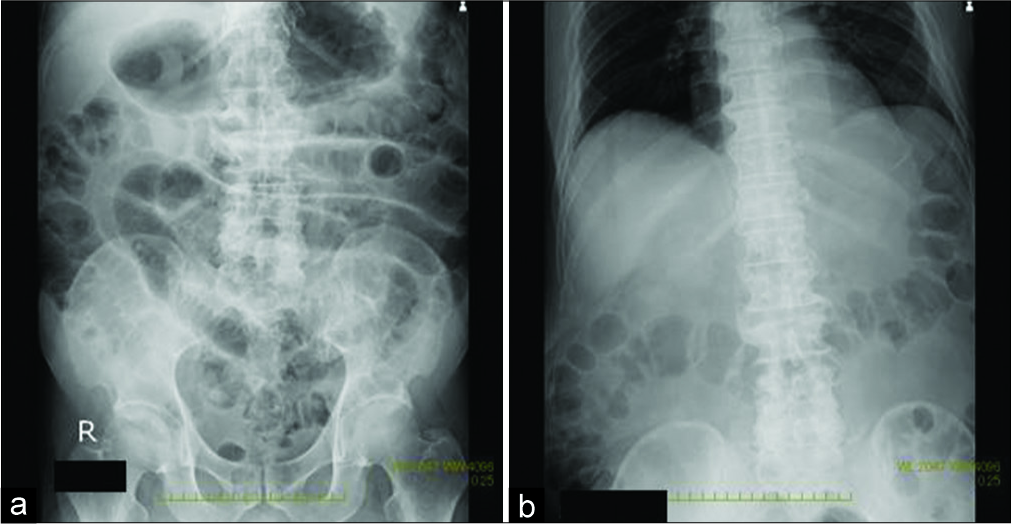
However, following the surgery, the patient developed a persistent small bowel ileus. When conventional therapy (e.g., gastric suction, laxatives, dimethicone, and dinoprost) failed to resolve the ileus over the first 3 postoperative days, the patient was given Kampo medications consisting of bukuryoin (TJ-69, Tsumura & Co., Tokyo, Japan) 7.5 g/day and hangekobokuto (TJ-16, Tsumura & Co.) 7.5 g/day [
DISCUSSION
After the spinal cord injury, abdominal distention due to paralysis of the gastrointestinal tract is commonly observed.[
CONCLUSION
In a 63-year-old male who was quadriplegic following a hyperextension cervical cord injury, the MR and CT studies documented severe OPLL and spinal cord edema from C3 to C6. When the patient developed a persistent small intestine ileus unresponsive to the typical medications, TJ-116 Kampo therapy was instituted and effectively resolved the problem.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Hirano Y, Ohara Y, Mizuno J, Itoh Y. History and evolution of laminoplasty. Neurosurg Clin N Am. 2018. 29: 107-13
2. Isai H.editors. Handbook of the Kampo Medicines for Clinical Practice, 147 Prescriptions at a Glance. Tokyo: Nanzando; 2018. p.
3. Matsumoto K, Mine K. Significance of Kampo medicine on treatment of gas type of irritable bowel syndrome. J Jpn Assoc Orient Psychosom Med. 1992. 7: 12-7
4. Nagai A, Shibamoto Y, Ogawa K, Inoda K, Yoshida M, Kikuchi Y. Analysis and management of rectal gas with kampo formulas during intensity-modulated radiotherapy of prostate cancer: A case series study. J Altern Complement Med. 2016. 22: 480-5
5. Watson N. Late ileus in paraplegia. Paraplegia. 1981. 19: 13-6