Interscapular pain with Chiari Type I malformation attributed to atypical spinal accessory neuralgia
- Department of Neurosurgery, Lifeline Hospital and Research Center, Azamgarh, Uttar Pradesh, India.
DOI:10.25259/SNI_67_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Anoop Kumar Singh, Gayatri Kumari. Interscapular pain with Chiari Type I malformation attributed to atypical spinal accessory neuralgia. 17-May-2021;12:226
How to cite this URL: Anoop Kumar Singh, Gayatri Kumari. Interscapular pain with Chiari Type I malformation attributed to atypical spinal accessory neuralgia. 17-May-2021;12:226. Available from: https://surgicalneurologyint.com/surgicalint-articles/10813/
Abstract
Background: The spinal accessory nerve (XI) is traditionally considered a motor nerve. However, as some studies have documented the presence of nociceptive fibers in XI, vascular XI neural compression may lead to an atypical neuralgia.
Case Description: A 27-year-old male presented with a Chiari Type I malformation contributing to interscapular pain. Following a posterior fossa and microvascular decompression of XI, the patient improved, thus confirming the underlying diagnosis of a XI atypical neuralgia.
Conclusion: Unilateral, posterior-interscapular deep pain may be due to an atypical spinal accessory nerve (XI) neuralgia rather than a Chiari Type I malformation or syrinx. Posterior fossa decompression, subpial tonsillar resection, and XI nerve microvascular decompression resolved this patient’s complaints. In the future, CTA or MRA vascular studies along with a balanced steady-state gradient echo MRI sequence would be better to document the presence of XI nerve neurovascular compromise.
Keywords: Chiari malformation Type I, Spinal Accessory nerve, Spinal accessory neuralgia
INTRODUCTION
The spinal accessory nerve (CNXI) is traditionally considered a motor nerve. However, the extent of its’ sensory components has been underestimated.[
CASE REPORT
A 27-year-old male presented with a left-sided chest, shoulder, suprascapular/interscapular pain, and burning paresthesia in the left upper extremity of 3 months’ duration. On examination, the only neurological deficit was 50% hypoesthesia involving the left C5 to D2 distributions (i.e., pain and temperature). The preoperative cervical MRI T2-weighted study showed a Type I Chiari malformation and syrinx (i.e., cerebellar tonsillar herniation up to the C1 level, diffusely dilated central canal from C5 to D3, and nonenhancing hyperintensity, present in the upper cervical cord [
Surgery
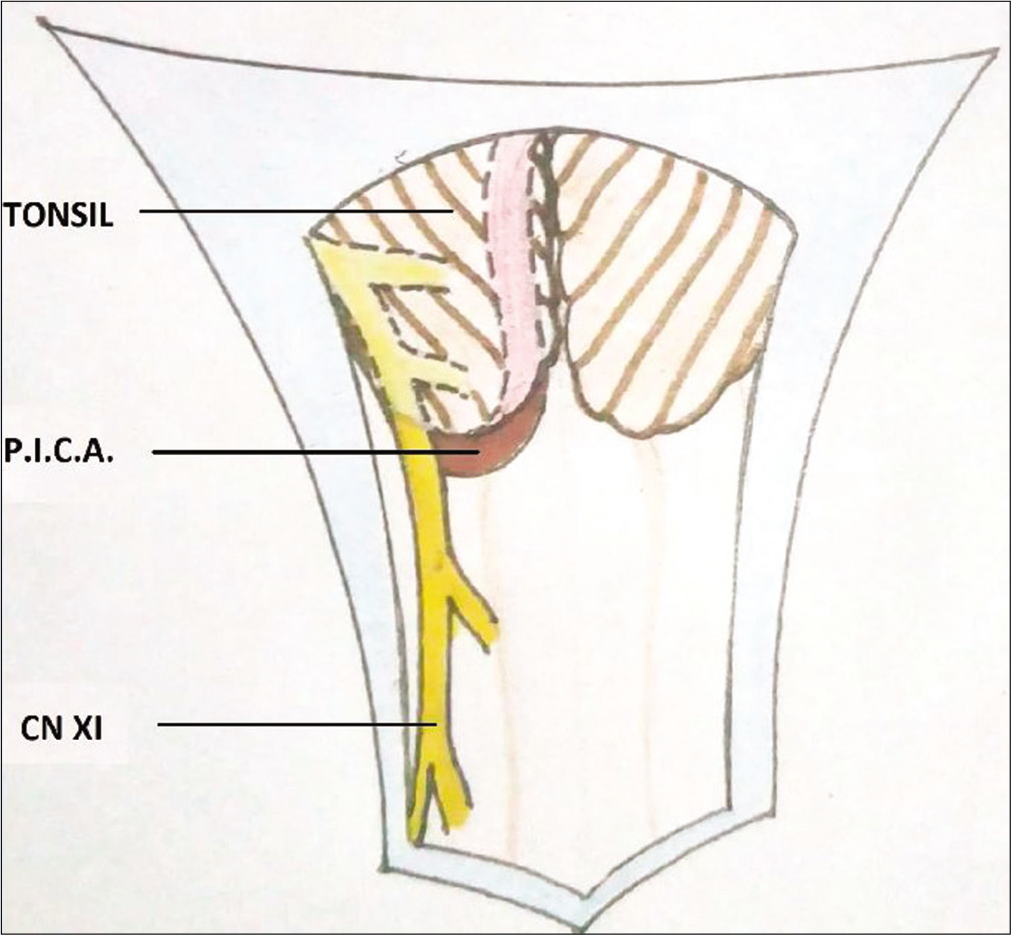
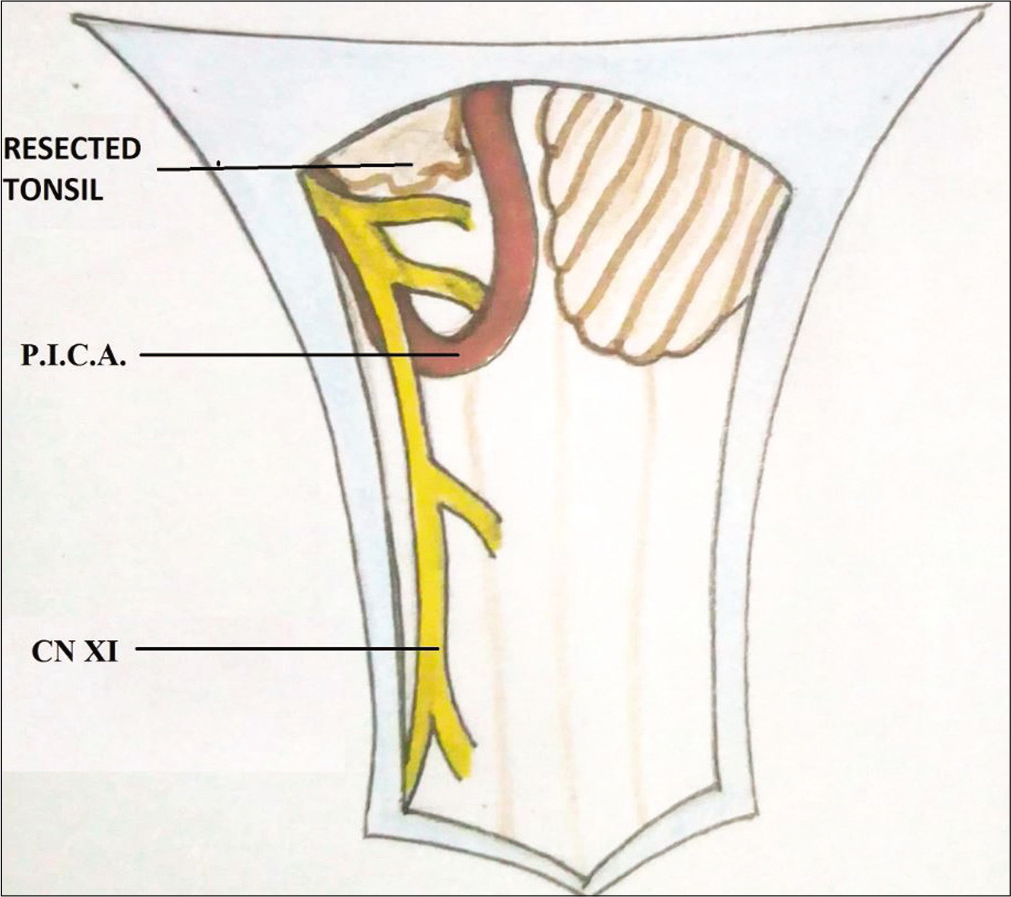
The patient underwent a posterior fossa decompression consisting of a suboccipital craniectomy, C1 laminectomy, and “Y” shape dural incision. Once the dura was opened, the tonsils were found to be herniated into the spinal canal up to the C1 level; arachnoidal adhesions between the tonsils and cord were removed. Further, at the level of the foramen magnum, the left XI cranial nerve was severely compressed between the left-sided herniated tonsil and posterior inferior cerebellar artery (PICA) [
Postoperative recovery
Postoperatively, the left interscapular pain reduced significantly with immediate effect; however, the left upper extremity burning paresthesia took 2 months to subside, while the sensory hypoesthesia persisted even after 18 months.
DISCUSSION
Chiari I malformation is characterized by herniation of the cerebellar tonsils or PICA loops below the foramen magnum. Neurological complaints may include; spastic paraparesis, amyotrophy, dissociated sensory loss, cerebellar signs, and lower cranial nerve palsies.[
Spinal accessory nerve (XI) anatomy
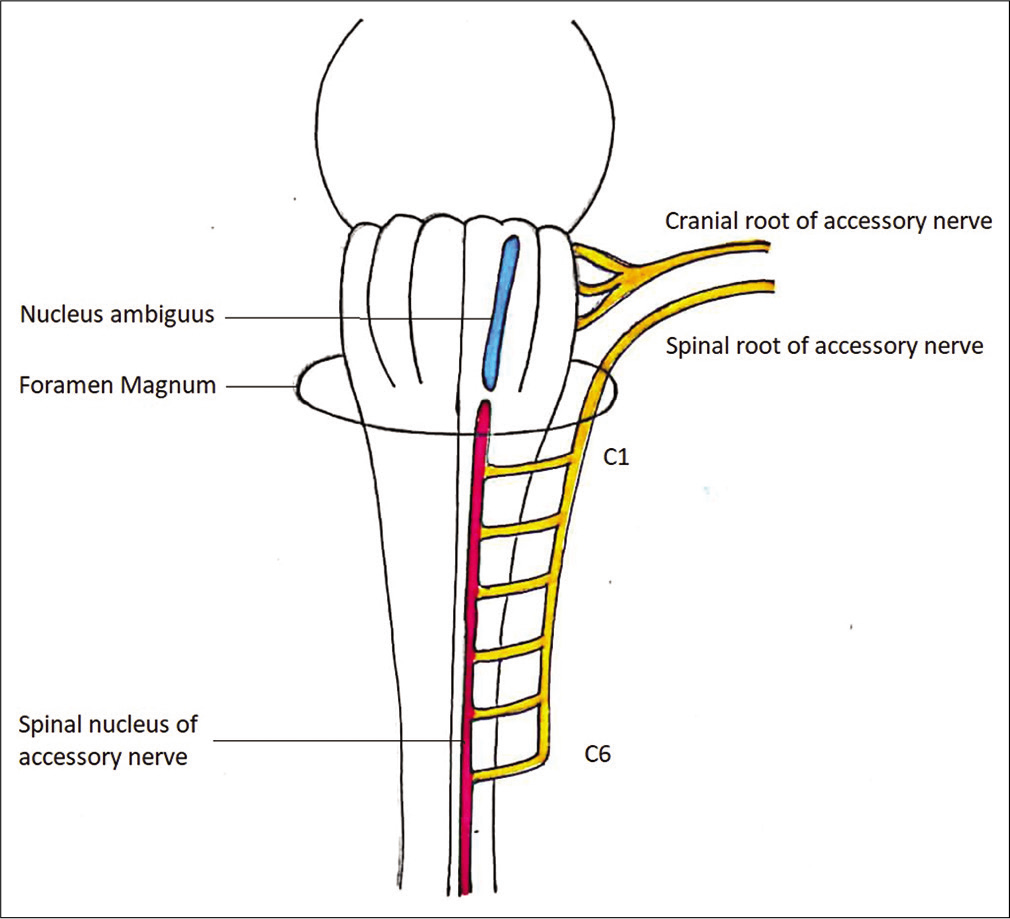
The spinal accessory nerve (CNXI) includes two parts; a smaller cranial and a major spinal component. The cranial division emerges from the medulla oblongata. The fibers of the spinal portion arise from special visceral efferent motor cells in the spinal accessory nucleus from C2 to C6. The spinal part leaves the anterior surface of the spinal cord between the dorsal and ventral sulci; after fusion of rootlets, the nerve travels cranially [
CNXI nociceptive fibers
Although the literature shows that CNXI is predominantly a motor nerve and conveys proprioceptive information only, there is pathological evidence that CNXI also contains nociceptive sensory components.[
Anatomy of the PICA
The tonsillomedullary segment of PICA passes posterior to lower cranial nerves. At the craniovertebral junction, PICA frequently has a tortuous course with complex loops, and the relationship between the tonsillomedullary segment of PICA, tonsils, and the foramen magnum vary; this creates a potential site for an anatomical anomaly (i.e., ACM Type 1 can cause vascular compression syndrome).[
Syringomyelia
Conventionally, nuchal and scapular pain in ACM patients is attributed to associated syringomyelia. Still, showing the presence of nociceptive fibers in CNXI, we have raised the question of whether atypical XI cranial nerve neuralgic pain is actually responsible for these symptoms.
CONCLUSION
Posterior fossa decompression along with subpial resection of the left-sided cerebellar tonsil and microvascular decompression of the left cranial nerve XI resolved this patient’s interscapular pain/dysesthesias/atypical XI nerve neuralgia.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bremner-Smith AT, Unwin AJ, Williams WW. Sensory Pathways in the spinal accessory nerve. J Bone Joint Surg Br. 1999. 81: 226-8
2. Ning L, Wei-Guo Z, Chun-Hua P, Wen-Lei Y. Hemifacial spasm associated with Type 1 chiari malformation: A retrospective study of 13 cases. Neurosurg Rev. 2017. 40: 275-9
3. Rhoton AL. The cerebellar arteries. Rhotons Anat. 2003. 53: 461-500
4. Suresh N, Grish M, Rao BR.editors. Syringomyelia. Ramamurthi and Tandon’s Textbook of Neurosurgery. 3rd ed Ch. 24. New Delhi. Jaypee Brothers Medical Publishers. 2012. p. 293-305
5. Wetmore C, Elde R. Detection and characterization of a sensory microganglion associated with the spinal accessory nerve: A scanning laser confocal microscopic study of the neurons and their processes. J Comp Neurol. 1991. 305: 148-63
6. William WC.editors. The spinal accessory nerve. DeJong’s the Neurologic Examination. Philadelphia, PA: Lippincott Williams and Wilkins; 2005. p. 263-9
7. Williams WW, Twyman RS, Donell ST, Birch R. The posterior triangle and the painful shoulder: Spinal accessory nerve injury. Ann R Coll Surg Engl. 1996. 78: 521-5
8. Windle WF. The sensory components of the spinal accessory nerve. J Comp Neurol. 1931. 53: 115-27