- Department of Surgery, Chiang Mai University, Chiang Mai, Thailand.
Correspondence Address:
Jirapong Vongsfak, Department of Surgery, Chiang Mai University, Chiang Mai, Thailand.
DOI:10.25259/SNI_221_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kriengsak Limpastan, Thunya Norasetthada, Wanarak Watcharasaksilp, Tanat Vaniyapong, Chumpon Jetjumnong, Chanon Srihagulang, Todsapon Praphanuwat, Jirapong Vongsfak. Intracranial pressure monitoring for severe traumatic brain injury: A retrospective study of 273 consecutive patients. 21-Jun-2024;15:208
How to cite this URL: Kriengsak Limpastan, Thunya Norasetthada, Wanarak Watcharasaksilp, Tanat Vaniyapong, Chumpon Jetjumnong, Chanon Srihagulang, Todsapon Praphanuwat, Jirapong Vongsfak. Intracranial pressure monitoring for severe traumatic brain injury: A retrospective study of 273 consecutive patients. 21-Jun-2024;15:208. Available from: https://surgicalneurologyint.com/surgicalint-articles/intracranial-pressure-monitoring-for-severe-traumatic-brain-injury-retrospective-study-of-273-consecutive-patients/
Abstract
Background: Intracranial pressure (ICP) monitoring is essential in severe traumatic brain injury (sTBI) cases; yet, the frequency of high ICP occurrences remains debated. This study presents a 9-year analysis of ICP monitoring using intraventricular catheters among sTBI patients.
Methods: A retrospective review of 1760 sTBI patients (Glasgow Coma Score 20 mmHg for 10–15 min during 72 h were categorized with high ICP. Data collected included demographics, computed tomography (CT) findings, intra- and post-operative ICP, and complications.
Results: Of 273 patients, 228 were male and 45 females, aged 18–80 (71.30% aged 18–45). Traffic accidents were the primary cause (90.48%). Fifty-two-point seventy-five percent experienced high ICP, correlating significantly with subdural hematoma (P P P = 0.046) on initial CT. Twenty patients (7.3%) developed meningitis. Lower mortality rates and improved outcomes were observed in the low ICP group across discharge 3-and 6-month follow-ups.
Conclusion: Adherence to BTF guidelines yielded a 52.75% high ICP rate. Significant correlations were found between high ICP and specific CT abnormalities. This study underscores the benefits of ICP monitoring in selected sTBI cases, suggesting a need to review criteria for initiating monitoring protocols.
Keywords: Functional outcome, Intracranial pressure monitoring, Severe traumatic brain injury
INTRODUCTION
Traumatic brain injury (TBI) is one of the leading causes of death and severe disability globally, especially in most developing countries. Morbidity and mortality remain high even considering the major improvements in medical, surgical, and intensive care in the last couple of decades. Improved intensive care and several monitoring techniques among patients with severe TBI (sTBI) may prolong life and decrease mortality rates, but long-term morbidity and functional outcome have remained questionable.[
MATERIALS AND METHODS
The Ethics Committee approved our study in our institute before data collection, and informed consent was waived as a retrospective design (IRB225/2014). We retrospectively studied patients with sTBI admitted to our hospital between January 2011 and December 2019. Our inclusion criteria comprised patients with sTBI (Glasgow coma scale [GCS] <9) exhibiting abnormal CT findings and lacking indications for emergency hematoma evacuation surgery. Patients with multiple injuries, loss of follow-up, or insufficient medical records during the follow-up period were excluded from the study.
After cranial CT scanning verified the indication for ICP monitoring, all patients were operated on for a ventricular catheter insertion through the right frontal burr hole. The ICP was recorded at the intraoperative period and continuously monitored for 48–72 hours postoperation. Patients having ICP >20 mmHg for 10–15 min during monitoring were grouped as the high ICP group and the rest were grouped as the low ICP group. Patient’s demographic data, GCS, and ICP parameters were recorded at the first insertion of external ventricular drainage (EVD) and were continuously monitored for 48–72 h. During the postoperation period, Glasgow outcome scale (GOS) and complications were recorded at discharge and 3 and 6 months after discharge. All intracranial lesions were calculated in volume using the modified ellipsoid method.
RESULTS
One thousand seven hundred and sixty patients with sTBI were admitted to our hospital between January 2011 and December 2019. Exactly 1224 patients harboring intracranial lesions, indicating emergency surgical evacuation, were excluded from the study.
All totaled, 536 patients presented salvageable sTBI (GCS <9) with abnormal CT findings on admission and age ≥18 years old. Of those recommended by BTF guidelines for ICP monitoring, 276 patients proceeded to ICP monitoring, and the remaining 260 were managed without ICP monitoring, affirmed by the attending neurosurgeon’s opinion, surgical procedure refused by the patient’s relatives or the patients who die in the emergency department. Three patients failed ICP measurement after surgery.
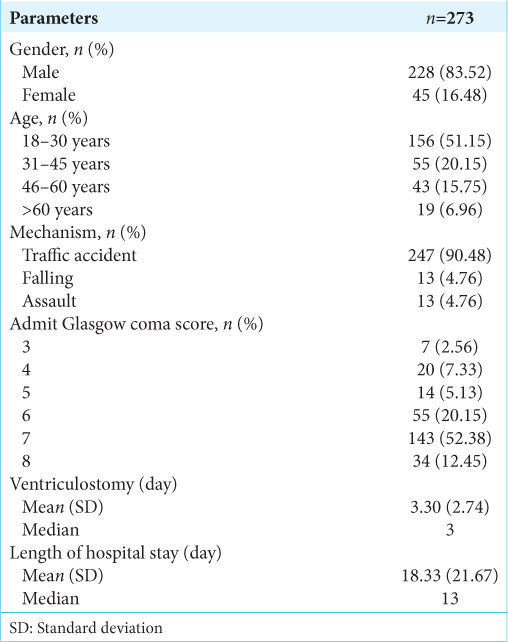
Among 273 patients with TBI, 228 (83.5%) were male and 45 (16.5%) were female. Age ranged from 18 to 80 years old. In all, 71.3% of patients were 18–45 years old. The most common cause of injury was traffic accidents (90.48%), while falling and assault were minor causes, as shown in
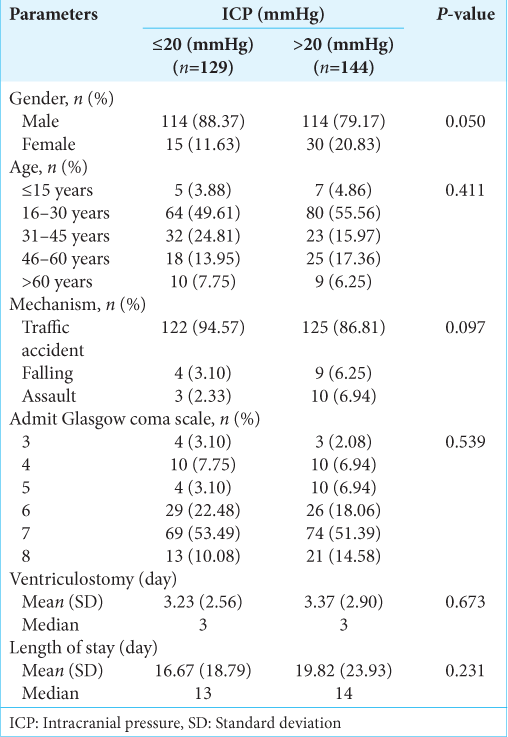
In total, 144 (52.75%) patients experienced high ICP (>20 mmHg) for 10 ~ 15 min during ICP monitoring, and 129 (47.25%) patients never had high ICP during the monitoring period. No statistically significant demographics differed between the two groups, as shown in
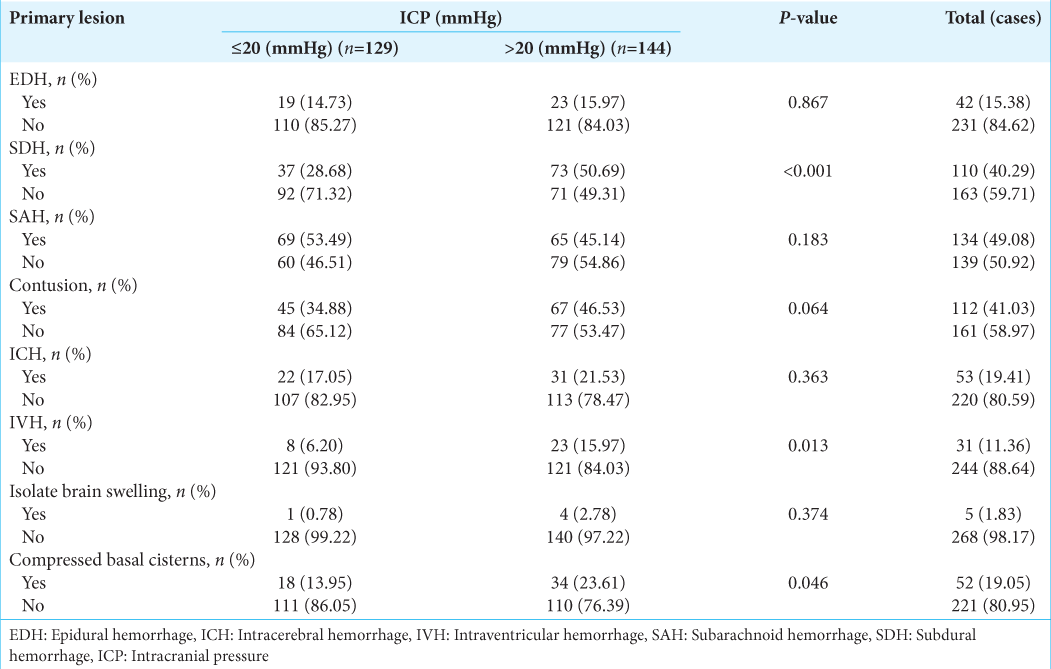
Present of subdural hemorrhage (SDH), intraventricular hemorrhage (IVH), and compressed basal cisterns on cranial CT on admission were significantly related to high ICP during admission (P < 0.001, P < 0.013, and P < 0.046, respectively), as shown in
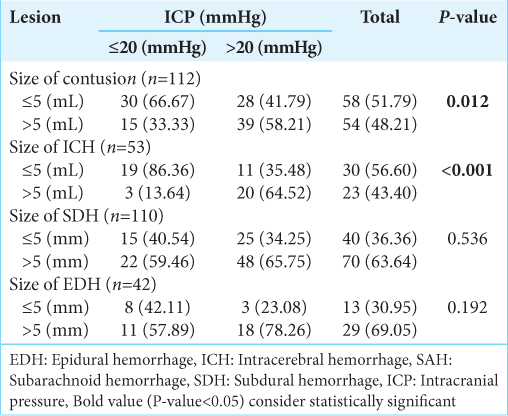
Among the intracranial lesions found on the initial cranial CT scan, intraparenchymal lesions, including cerebral contusion and intracerebral hematoma size of >5 mL, compared with volume <5 mL, were significantly related to high ICP (P < 0.012 and P < 0.001, respectively) while size of other lesions was not significantly related to high intracranial pressure, as shown in
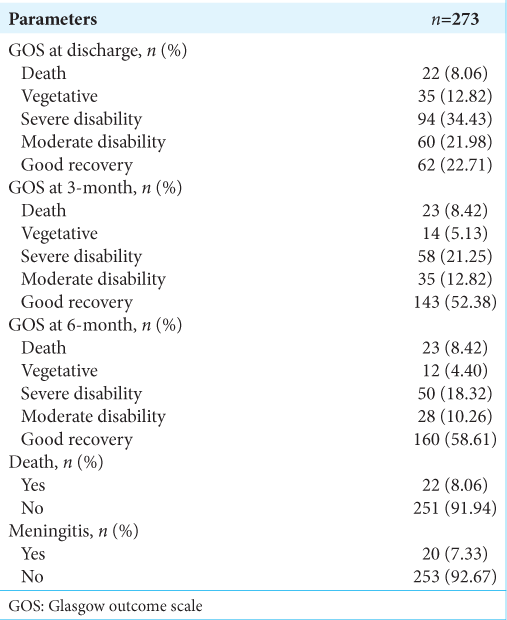
Overall, the mortality rate was 8.06% at discharge and 8.42% at 3 and 6 months after discharge. About 47.25% had poor outcomes (vegetative state and severe disability) at discharge and decreased to 26.38% and 22.72% at 3 and 6 months after discharge, while 44.69% had good outcomes (Good recovery and moderate disability) at discharge and increased to 65.20% and 68.87% at 3 and 6 months after discharge. Meningitis is the only procedural-related complication found in 7.33%, as shown in
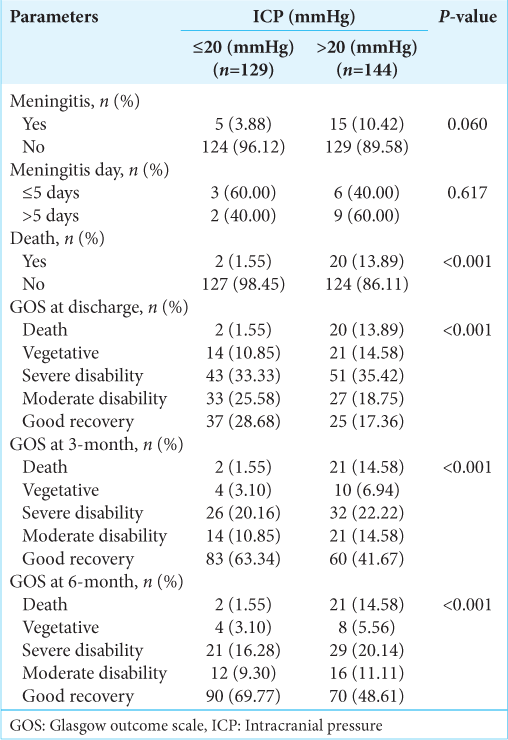
The mortality rate was significantly high in the high intracranial pressure group (P < 0.001), while meningitis was not significantly different between the two groups. GOS at discharge, 3 and 6 months were all significantly better in the low intracranial pressure group (P < 0.001), as shown in
DISCUSSION
This study examined the role of ICP monitoring in sTBI according to BTF recommendations.[
The principal management of TBI is to avoid intracranial hypertension to maintain cerebral perfusion pressure and minimal secondary brain injury. This is important to maintain ICP <20 mmHg for the management strategy of sTBI. The current trend in ICP monitoring, as recommended by the BTF, suggests that ICP should be monitored in all cases of severe TBI with abnormal CT findings, such as hematoma, contusion, swelling, brain herniation, or cistern compression. It also advises considering ICP monitoring in cases where the CT scan is negative but meets two or more of the following criteria: age over 40 years, unilateral or bilateral motor posturing, or systolic blood pressure below 90 mmHg.[
The two different types of ICP monitoring in TBI included intraventricular and intraparenchymal, with their benefits and drawbacks.[
Due to different study designs, low rate of ICP monitoring, different types of ICP monitoring, and various management practices, that is, increased ICP protocol and limited randomized trials, the result of ICP monitoring with the clinical benefit in sTBI remains difficult to conclude. Our study confirms that increased ICP (ICP >20 mmHg) was associated with high mortality and poor outcome among patients with sTBI. However, the rate of patients with high ICP was only 50% in our study, following BTF guidelines. Abnormal CT findings on admissions, including SDH, IVH, and compressed basal cistern, were significantly associated with high ICP. These findings should inform guideline modifications to enable more precise patient selection for ICP monitoring, leading to cost-effective benefits and reduced complication rates from unnecessary monitoring. Therefore, further studies are warranted to assess the long-term and cost-effective benefits of these modifications.
Our study encountered limitations due to the retrospective study nature and prospective design using a single institute. In addition, our center monitored only ICP with an intraventricular catheter. Other intracranial monitoring techniques such as brain tissue oxygenation or jugular bulb oxygen saturation, may provide more details affecting treatment outcome.
CONCLUSION
ICP monitoring in TBI remains beneficial for selected patients in reducing mortality and improving functional outcomes. However, the current yield of high ICP following BTF guidelines for monitoring is relatively low (52.75%). Modifications are needed to identify more specific candidates, particularly those with subdural hematoma, IVH, and compressed basal cisterns, which were significantly associated with high ICP . Future studies must provide clear conclusions about the current state of ICP monitoring in alignment with BTF guidelines, emphasizing both its limitations and potential benefits for patient management.
Ethical approval
The Ethics Committee approved our study in our institute before data collection, (IRB225/2014).
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Aiolfi A, Khor D, Cho J, Benjamin E, Inaba K, Demetriades D. Intracranial pressure monitoring in severe blunt head trauma: Does the type of monitoring device matter?. J Neurosurg. 2018. 128: 828-33
2. Biersteker HA, Andriessen TM, Horn J, Franschman G, van der Naalt J, Hoedemaekers CW. Factors influencing intracranial pressure monitoring guideline compliance and outcome after severe traumatic brain injury. Crit Care Med. 2012. 40: 1914-22
3. Carney N, Totten AM, O’Reilly C, Ullman JS, Hawryluk GW, Bell MJ, editors. Guidelines for the management of severe traumatic brain injury 4th edition. Brain Trauma Foundation. 2016. p. 244 Available from: https://braintraumaorg/uploads/03/12guidelines_for_management_of_severe_tbi_4th_edition.pdf [Last accessed on 2019 Jun 26]
4. Chesnut RM, Temkin N, Carney N, Dikmen S, Rondina C, Videtta W. A trial of intracranial-pressure monitoring in traumatic brain injury. N Engl J Med. 2012. 367: 2471-81
5. Dawes AJ, Sacks GD, Cryer HG, Gruen JP, Preston C, Gorospe D. Intracranial pressure monitoring and inpatient mortality in severe traumatic brain injury: A propensity score–matched analysis. J Trauma Acute Care Surg. 2015. 78: 492-502
6. Dimitriou J, Levivier M, Gugliotta M. Comparison of complications in patients receiving different types of intracranial pressure monitoring: A retrospective study in a single center in Switzerland. World Neurosurg. 2016. 89: 641-6
7. Hoffman H, Bunch KM, Furst T, Chin LS. Use of intracranial pressure monitoring in patients with severe traumatic brain injury. World Neurosurg. 2020. 142: e385-95
8. Kasotakis G, Michailidou M, Bramos A, Chang Y, Velmahos G, Alam H. Intraparenchymal vs extracranial ventricular drain intracranial pressure monitors in traumatic brain injury: Less is more?. J Am Coll Surg. 2012. 214: 950-7
9. Khormi YH, Senthilselvan A, O’Kelly C, Zygun D. Adherence to brain trauma foundation guidelines for intracranial pressure monitoring in severe traumatic brain injury and the effect on outcome: A population-based study. Surg Neurol Int. 2020. 11: 118
10. Murthy SB, Moradiya Y, Shah J, Hanley DF, Ziai WC. Incidence, predictors, and outcomes of ventriculostomy-associated infections in spontaneous intracerebral hemorrhage. Neurocrit Care. 2016. 24: 389-96
11. Okazaki T, Kawakita K, Kuroda Y. Hospital-level intracranial pressure monitoring utilization and functional outcome in severe traumatic brain injury: A post hoc analysis of prospective multicenter observational study. Scand J Trauma Resusc Emerg Med. 2021. 29: 5
12. Rosenfeld JV, Thomas PA, Hunn MK. Intracranial pressure monitoring in severe traumatic brain injury: Quo Vadis?. ANZ J Surg. 2021. 91: 2568-70
13. Shen L, Wang Z, Su Z, Qiu S, Xu J, Zhou Y. Effects of intracranial pressure monitoring on mortality in patients with severe traumatic brain injury: A meta-analysis. PLoS One. 2016. 11: e0168901
14. Suehiro E, Fujiyama Y, Koizumi H, Suzuki M. Directions for use of intracranial pressure monitoring in the treatment of severe traumatic brain injury using data from the Japan Neurotrauma Data Bank. J Neurotrauma. 2017. 34: 2230-4
15. Yang C, Ma Y, Xie L, Wu X, Hui J, Jiang J. Intracranial pressure monitoring in the intensive care unit for patients with severe traumatic brain injury: Analysis of the CENTER-TBI China registry. Neurocrit Care. 2022. 37: 160-71
16. Yuan Q, Wu X, Yu J, Sun Y, Li Z, Du Z. Effects and clinical characteristics of intracranial pressure monitoring-targeted management for subsets of traumatic brain injury: An observational multicenter study. Crit Care Med. 2015. 43: 1405-14