- Department of Neurosurgery, Medical College of Wisconsin, Children's Hospital of Wisconsin, Milwaukee, WI, USA
- Department of Infectious Diseases, Children's Hospital of Wisconsin, Milwaukee, WI, USA
Correspondence Address:
Ha Son Nguyen
Department of Infectious Diseases, Children's Hospital of Wisconsin, Milwaukee, WI, USA
DOI:10.4103/2152-7806.182388
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nguyen HS, Foy A, Havens P. Intracranial subdural empyema after surgery for lumbar lipomyelomeningocele: A rare complication. Surg Neurol Int 13-May-2016;7:
How to cite this URL: Nguyen HS, Foy A, Havens P. Intracranial subdural empyema after surgery for lumbar lipomyelomeningocele: A rare complication. Surg Neurol Int 13-May-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/intracranial-subdural-empyema-after-surgery-for-lumbar-lipomyelomeningocele-a-rare-complication/
Abstract
Background:Surgery is routinely recommended for lumbar lipomyelomeningocele, especially in the setting of tethered cord syndrome. The most common complications are wound infections and cerebrospinal fluid (CSF) leak, which remain confined to the surgical site. To the best of our knowledge, there have been no prior reports relating an intracranial subdural empyema following detethering surgery. Prompt diagnosis is essential since subdural empyema is a neurosurgical emergency.
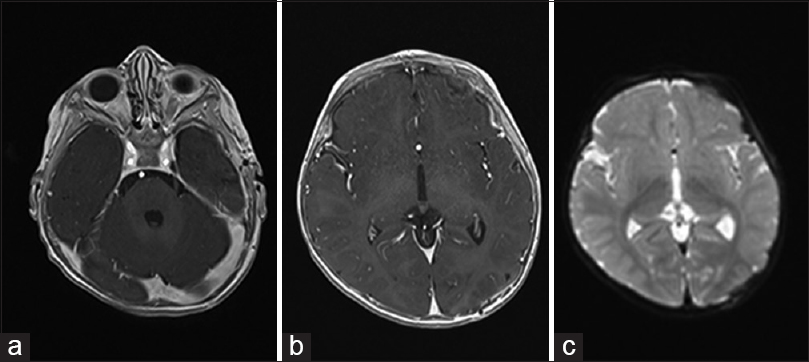
Case Description:The patient was an 11-month-old male who underwent detethering surgery for a lumbar lipomyelomeningocele. This was followed by wound drainage consistent with CSF leak, requiring revision. Cultures grew three aerobes (Escherichia coli, Enterococcus, and Klebsiella) and three anaerobes (Clostridium, Veillonella, and Bacteroides). He was started on cefepime, vancomycin, and flagyl. The patient required two more wound revisions and placement of an external ventricular drain (EVD) secondary to persistent wound leakage. A subsequent magnetic resonance imaging (MRI) brain was carried out due to protracted irritability, which revealed extensive left subdural empyema along the parietooccipital region and the inferior and anterior temporal lobe. He underwent evacuation of the subdural empyema where cultures exhibited no growth. Subsequently, he progressed well. His lumbar incision continued to heal. Serial MRI brains and inflammatory markers were reassuring. He weaned off his EVD and went home to complete a 6-week course of antibiotics. Upon completion of his antibiotics, he returned for a clinic visit; he exhibited no interim fevers or wound issues; cranial imaging documented no evidence of a residual or recurrent subdural empyema.
Conclusion:Intracranial subdural empyema may occur after wound complications from detethering surgery despite early initiation of broad-spectrum antibiotics. Possible etiology may be local wound infection that seeds the subdural space and travels to the cranium, leading to meningitis and subdural empyema. Such a scenario should prompt surveillance imaging of the head as undiagnosed subdural empyema may lead to devastating consequences.
Keywords: Lipomyelomeningocele, subdural empyema, tethered cord syndrome
INTRODUCTION
Lumbar lipomyelomeningocele is a form of occult spinal dysraphism that can cause tethered cord syndrome, leading to neurological, urological, and orthopedic dysfunction.[
CASE PRESENTATION
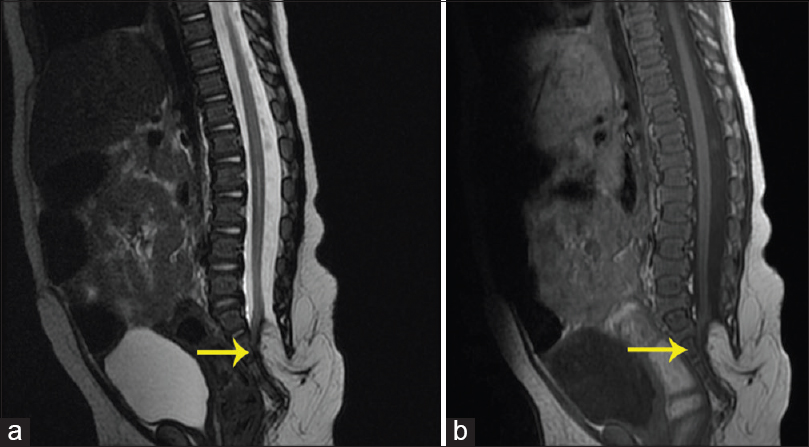
The patient was a male who had been followed for an S-shaped gluteal crease since age 2 weeks. At age 3 months, a magnetic resonance imaging (MRI) L spine revealed a lumbar lipomyelomeningocele (2.7 cm rostrocaudal × 1.4 cm transverse × 1 cm anterior-posterior). There was absence of the posterior elements at S3, S4, and S5 vertebrae. The conus medullaris terminated at S2 [
Postoperatively, he exhibited his baseline neurological function. He was kept flat for 2 days, sedated with a dexmedetomidine drip in the Intensive Care Unit. Initial course was complicated by profuse diarrhea, emesis, and intermittent fevers up to 40.3°C, attributed to viral gastroenteritis. On 5 days later, the wound was draining CSF. Wound exploration revealed a CSF fistula at the lower third of the incision with no gross signs of infection. The child was started on vancomycin, cefepime, and flagyl. Cultures grew three aerobes (Escherichia coli, Enterococcus, and Klebsiella) and three anaerobes (Clostridium, Veillonella, and Bacteroides). Because of persistent fevers and CSF drainage 2 days later, a right frontal external ventricular drain (EVD) was placed, and the lumbar wound was reexplored. The leak emanated from the superior 1 cm part of the incision where devitalized tissue was evident; this was debrided to bleeding tissue and closed. EVD was left at 5 cm above his external auditory canal. He was kept flat bed rest, intubated and sedated. Unfortunately, the wound exhibited further wound drainage 4 days later and was again re-explored. Frank purulent discharge was immediately encountered as the wound fell open superiorly. The suprafascial space was cultured, which eventually grew E. coli. There was no pus extending from the epidural/subfascial space. He was kept sedated and paralyzed postoperatively for 3 days to allow for wound healing.
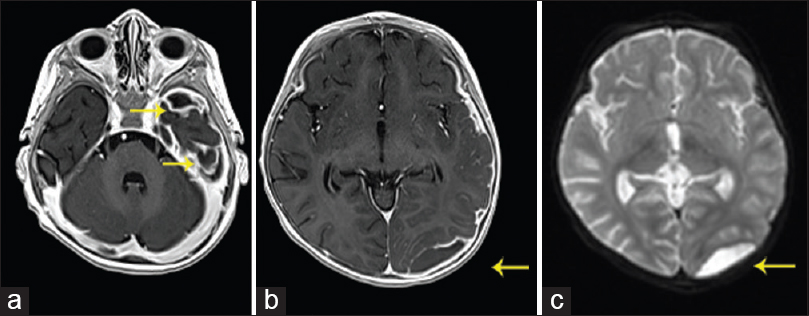
MRI brain performed because of persistent irritability showed extensive left-sided subdural empyema, greatest at the parietooccipital region and the inferior and anterior temporal lobe [
DISCUSSION
Intracranial subdural empyema may cause headaches, fevers, altered mental status, motor deficits, and seizures.[
The spread of infection from a spinal location to a cranial location is rare. Lumbar punctures, spinal anesthesia, and infected intrathecal baclofen pumps have been associated with meningitis.[
Our patient had several neurosurgical procedures: A right frontal EVD placement and the initial detethering surgery followed by three wound revisions. It seems reasonable that the etiology of the subdural empyema was from a wound infection after the initial surgery (secondary to wound drainage coupled with profuse diarrhea/wound contamination); the wound infection may seed the CSF space and travel to the cranium to form an empyema from the beginning. On the other hand, the persistent CSF leakage from the wound, compounded by EVD drainage, may induce formation of a left subdural hygroma/effusion, which was subsequently seeded with infection from the lumbar wound. The patient was kept flat for a prolonged period, which may facilitate the spread of infection to the cranium. Nevertheless, his MRI spine rostral to the surgical site did not exhibit any signs of infection. The polymicrobial bacteria from the cultures were consistent with a gastrointestinal source. Another possible source was EVD though its location was contralateral to the subdural empyema; moreover, the CSF was tested daily and remained negative throughout the hospitalization course. In addition, there were no signs of infection along the ventricular catheter on the MRI brain. On the other hand, only about 9% of CSF cultures are positive in patients with subdural empyema.[
The patient was on prolonged sedation/paralysis to encourage wound healing, but such a scenario limits the ability to assess for intracranial complications based on a physical examination. Given this rare complication, we recommend routine surveillance cranial imaging to rule out subdural empyema, as prompt diagnosis is associated with better outcomes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ackerman LL, Menezes AH. Spinal congenital dermal sinuses: A 30-year experience. Pediatrics. 2003. 112: 641-7
2. Baer ET. Post-dural puncture bacterial meningitis. Anesthesiology. 2006. 105: 381-93
3. Bruner DI, Littlejohn L, Pritchard A. Subdural empyema presenting with seizure, confusion, and focal weakness. West J Emerg Med. 2012. 13: 509-11
4. Chern JJ, Tubbs RS, Patel AJ, Gordon AS, Bandt SK, Smyth MD. Preventing cerebrospinal fluid leak following transection of a tight filum terminale. J Neurosurg Pediatr. 2011. 8: 35-8
5. Dashti SR, Baharvahdat H, Spetzler RF, Sauvageau E, Chang SW, Stiefel MF. Operative intracranial infection following craniotomy. Neurosurg Focus. 2008. 24: E10-
6. Dickerman RD, Piatt JH, Hsu F, Frank EH. Subdural empyema complicating cerebrospinal fluid shunt infection. Pediatr Neurosurg. 1999. 30: 310-1
7. Dill SR, Cobbs CG, McDonald CK. Subdural empyema: Analysis of 32 cases and review. Clin Infect Dis. 1995. 20: 372-86
8. Emami-Naeini P, Mahdavi A, Ahmadi H, Baradaran N, Nejat F. Brain abscess as a manifestation of spinal dermal sinus. Ther Clin Risk Manag. 2008. 4: 1143-7
9. French H, Schaefer N, Keijzers G, Barison D, Olson S. Intracranial subdural empyema: A 10-year case series. Ochsner J. 2014. 14: 188-94
10. Givner LB, Baker CJ. Anaerobic meningitis associated with a dermal sinus tract. Pediatr Infect Dis. 1983. 2: 385-7
11. Haranhalli N, Anand D, Wisoff JH, Harter DH, Weiner HL, Blate M. Intrathecal baclofen therapy: Complication avoidance and management. Childs Nerv Syst. 2011. 27: 421-7
12. Hayashi T, Takemoto J, Ochiai T, Kimiwada T, Shirane R, Sakai K. Surgical indication and outcome in patients with postoperative retethered cord syndrome. J Neurosurg Pediatr. 2013. 11: 133-9
13. Hsieh MH, Perry V, Gupta N, Pearson C, Nguyen HT. The effects of detethering on the urodynamics profile in children with a tethered cord. J Neurosurg. 2006. 105: S391-5
14. Idowu OE, Adekoya VA, Adeyinka AP, Beredugo-Amadasun BK, Olubi OO. Demography, types, outcome and relationship of surgically treated intracranial suppuration complicating chronic suppurative otitis media and bacterial rhinosinusitis. J Neurosci Rural Pract. 2014. 5: S48-52
15. James HE, Williams J, Brock W, Kaplan GW, Hoi SU. Radical removal of lipomas of the conus and cauda equina with laser microneurosurgery. Neurosurgery. 1984. 15: 340-3
16. Kasliwal MK, Sinha S, Kumar R, Sharma BS. Giant hemicranial calcified subdural empyema – Unusual complication following ventriculoperitoneal shunt insertion. Indian J Pediatr. 2009. 76: 651-2
17. Kumar A, Mahapatra AK, Satyarthee GD. Congenital spinal lipomas: Role of prophylactic surgery. J Pediatr Neurosci. 2012. 7: 85-9
18. Le Roux PC, Wood M, Campbell RA. Subdural empyema caused by an unusual organism following intracranial haematoma. Childs Nerv Syst. 2007. 23: 825-7
19. Lee GY, Paradiso G, Tator CH, Gentili F, Massicotte EM, Fehlings MG. Surgical management of tethered cord syndrome in adults: Indications, techniques, and long-term outcomes in 60 patients. J Neurosurg Spine. 2006. 4: 123-31
20. Mehta VA, Bettegowda C, Ahmadi SA, Berenberg P, Thomale UW, Haberl EJ. Spinal cord tethering following myelomeningocele repair. J Neurosurg Pediatr. 2010. 6: 498-505
21. Miller ES, Dias PS, Uttley D. Management of subdural empyema: A series of 24 cases. J Neurol Neurosurg Psychiatry. 1987. 50: 1415-8
22. Mount LA. Congenital dermal sinuses as a cause of meningitis, intraspinal abscess and intracranial abscess. J Am Med Assoc. 1949. 139: 1263-8
23. Pang D, Zovickian J, Oviedo A. Long-term outcome of total and near-total resection of spinal cord lipomas and radical reconstruction of the neural placode: Part I-surgical technique. Neurosurgery. 2009. 65: 511-28
24. Pathak A, Sharma BS, Mathuriya SN, Khosla VK, Khandelwal N, Kak VK. Controversies in the management of subdural empyema. A study of 41 cases with review of literature. Acta Neurochir (Wien). 1990. 102: 25-32
25. Proctor MR, Scott RM. Long-term outcome for patients with split cord malformation. Neurosurg Focus. 2001. 10: e5-
26. Radmanesh F, Nejat F, El Khashab M. Dermal sinus tract of the spine. Childs Nerv Syst. 2010. 26: 349-57
27. Salomão JF, Cervante TP, Bellas AR, Boechat MC, Pone SM, Pone MV. Neurosurgical implications of Pott's puffy tumor in children and adolescents. Childs Nerv Syst. 2014. 30: 1527-34
28. Santarius T, Qureshi HU, Sivakumaran R, Kirkpatrick PJ, Kirollos RW, Hutchinson PJ. The role of external drains and peritoneal conduits in the treatment of recurrent chronic subdural hematoma. World Neurosurg. 2010. 73: 747-50
29. Scheld MW, Marra CM, Whitley RJ.editorsInfections of the Central Nervous System. Philadelphia, Pennsylvania: Wolters Kluwer Health; 2014. p.
30. Tewari MK, Sharma RR, Shiv VK, Lad SD. Spectrum of intracranial subdural empyemas in a series of 45 patients: Current surgical options and outcome. Neurol India. 2004. 52: 346-9
31. Thuy M, Chaseling R, Fowler A. Spinal cord detethering procedures in children: A 5 year retrospective cohort study of the early post-operative course. J Clin Neurosci. 2015. 22: 838-42